CT Case 003
A 35yo male is transferred from a peripheral hospital with suspected GI bleed.
He has a background of liver cirrhosis secondary to alcohol excess and presented with shortness of breath and light-headedness. Initial investigations revealed a Hb of 47 g/dL.
Vital signs: BP 105/70, HR 110, RR 28, sats 97% 2LNP
Clinical examination: Multiple small bruises to abdomen and limbs, no external bleeding, no abdominal pain.
In light of no overt evidence of GI bleed (no haematemesis, no melaena) a CT abdomen was performed to look for a potential source of occult blood loss.
Describe and interpret the images
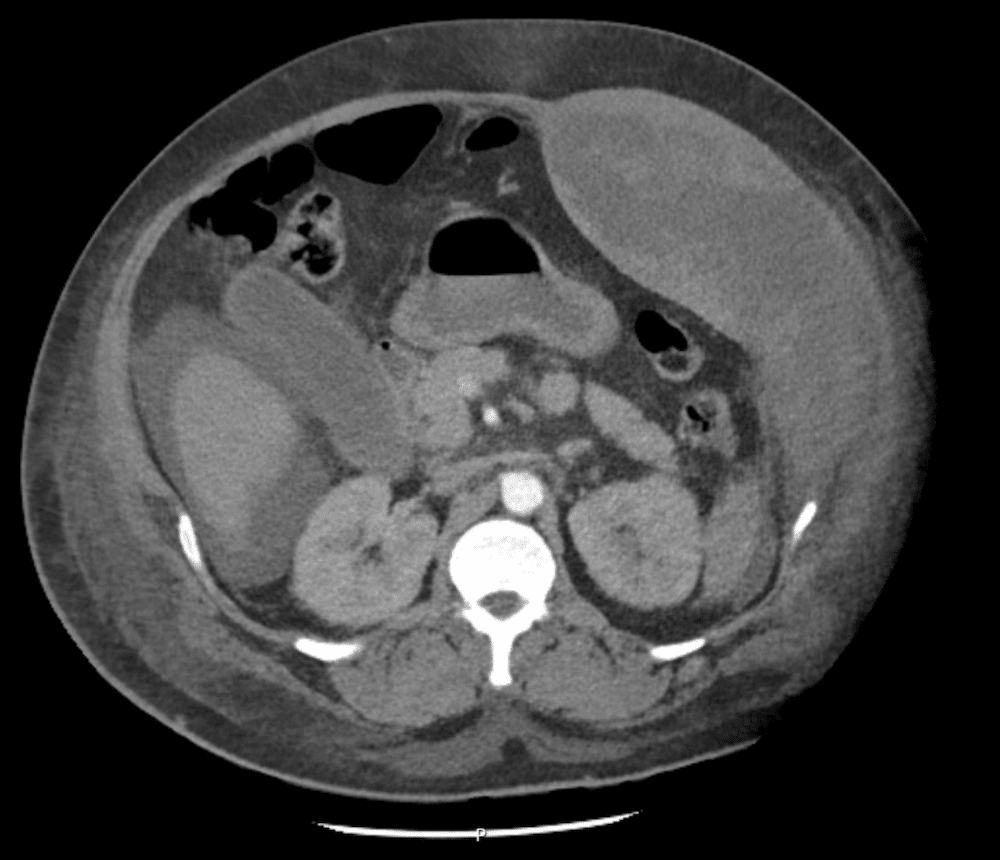
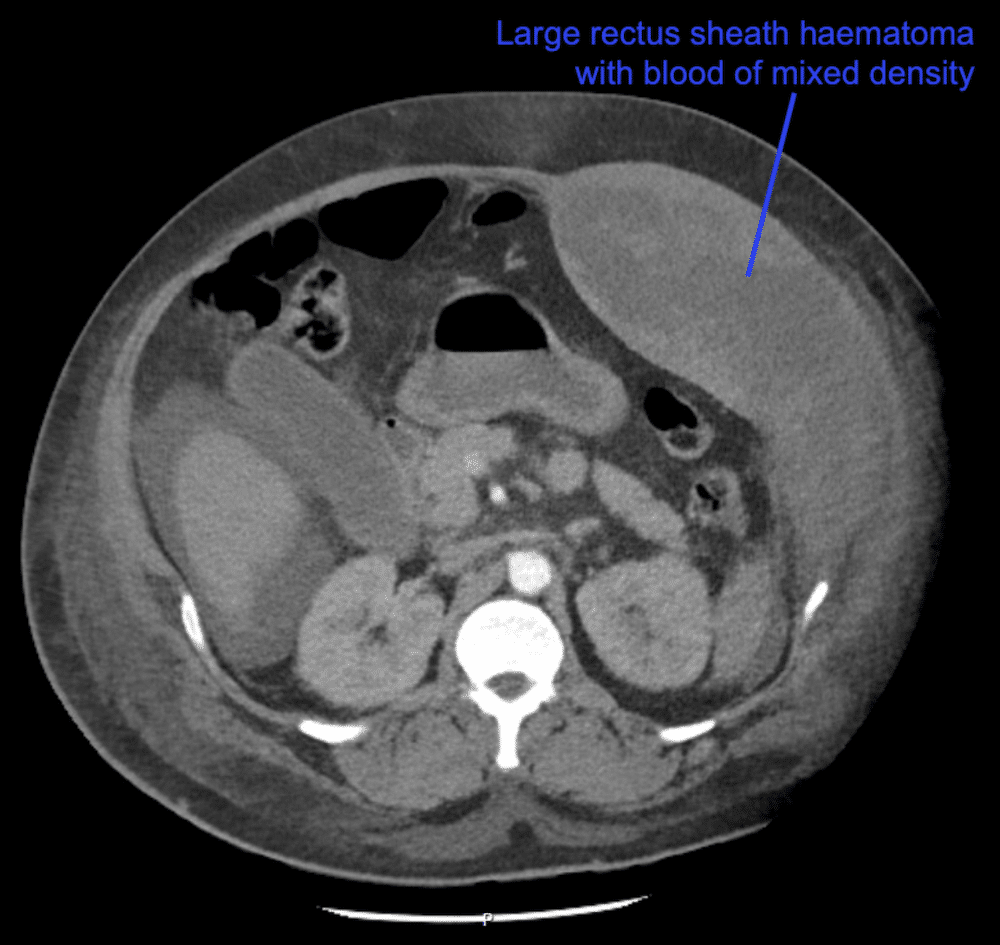
CT INTERPRETATION (non-contrast)
Rectus sheath haematoma
There is a large left sided rectus sheath haematoma, with some intra-peritoneal free fluid.
In the era of IV contrast media limitations (May-June 2022) his initial CT was non-contrast.
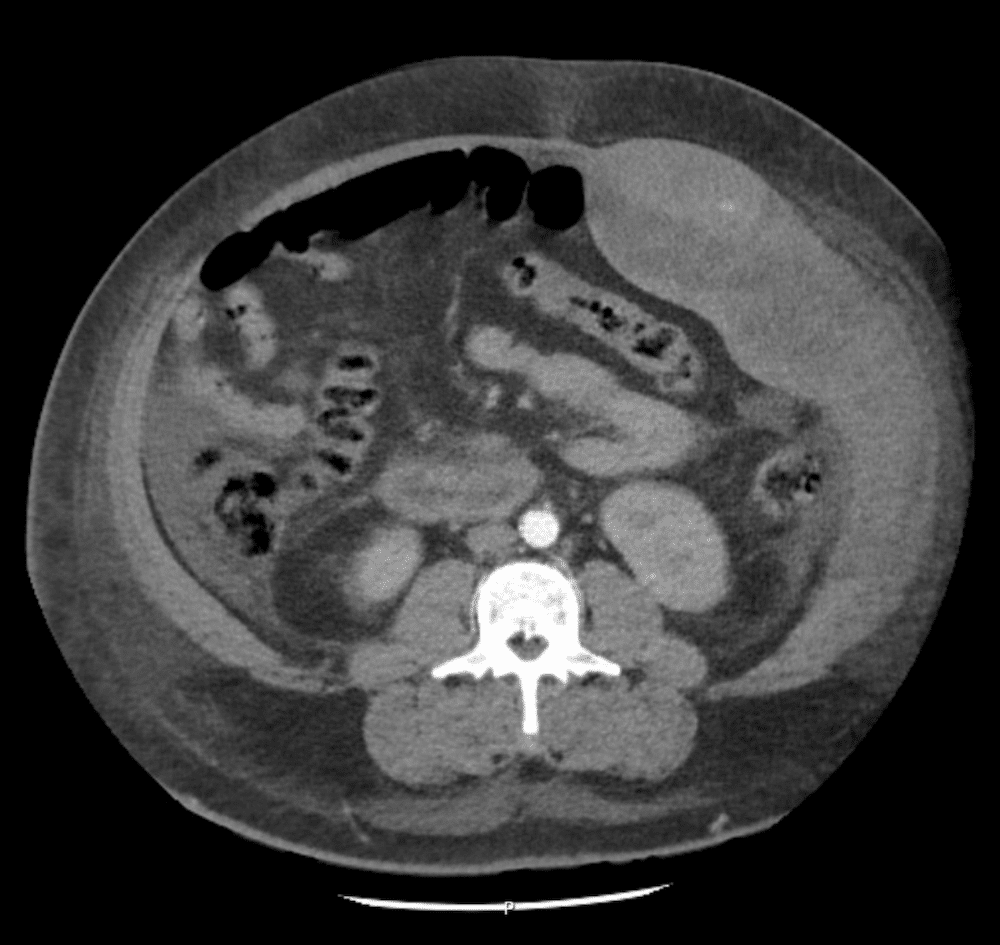
The images were reviewed and the patient was transferred back to CT for an arterial phase contrast scan.
Describe and interpret the images
CLINICAL PEARLS
Strangely this patient had NO abdominal pain despite the massive haematoma! (normally patients with this pathology present with abdominal pain)
The rectus abdominis muscle receives its blood supply from the superior and inferior epigastric arteries.
Rectus sheath haematoma is a rare condition that typically arises from rupture of superior or inferior epigastric arteries. It can occur in the setting of trauma or in anticoagulated patients.
This patient was auto-anticoagulated secondary to his liver disease.
Management of rectus sheath haematoma depends on the site and the extent of bleeding.
Superior epigastric artery haematoma normally will tamponade and no specific management is required.
On the other hand, inferior epigastric artery bleed is less likely to tamponade as it can extend into the pelvis and abdomen. In these cases, interventional radiology (for embolisation) or surgical ligation are necessary.
Our patient was sent for interventional radiology that evening and haemostasis was achieved.
REFERENCES
- Hartung MP. Abdominal CT interpretation. LITFL
[cite]
TOP 100 CT SERIES
Emergency Medicine Education Fellow at Liverpool Hospital NSW. MBBS (Hons) Monash University. Interests in indigenous health and medical education. When not in the emergency department, can most likely be found running up some mountain training for the next ultramarathon.
Sydney-based Emergency Physician (MBBS, FACEM) working at Liverpool Hospital. Passionate about education, trainees and travel. Special interests include radiology, orthopaedics and trauma. Creator of the Sydney Emergency XRay interpretation day (SEXI).
Dr Leon Lam FRANZCR MBBS BSci(Med). Clinical Radiologist and Senior Staff Specialist at Liverpool Hospital, Sydney




