CT Case 102
A 52 year old man is brought to hospital by ambulance complaining of 2 weeks of abdominal pain and constipation. He denies previous significant medical or surgical background.
On arrival he has a systolic blood pressure of 70mmHg and severe metabolic acidosis with pH 7.06 and lactate 14. Renal function. is impaired with eGFR 26.
Physical examination reveals a grossly distended and tender abdomen.
A CT mesenteric angiogram is urgently arranged.
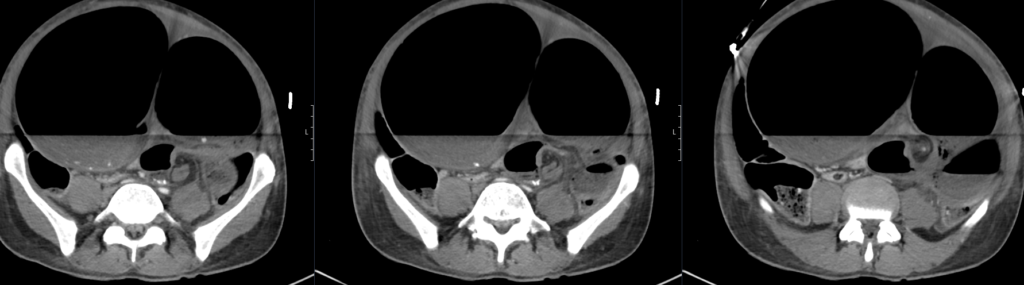
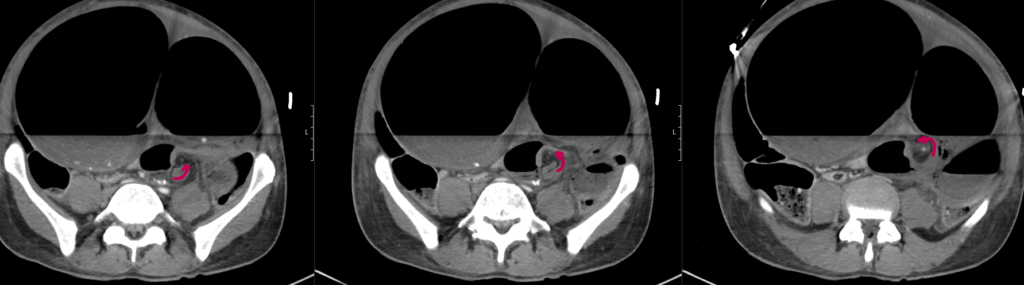
CT mesenteric angiogram

Describe and interpret the CT scan
There is evidence of a sigmoid volvulus.
The proximal large bowel as well as small bowel loops are dilated suggestive of an incompetent ileocaecal valve.
There is no pneumoperitoneum to suggest hollow viscus perforation.
There is a moderate volume of free fluid. No collection.
The distended bowel compresses the liver and displaces the gallbladder and spleen posteriorly.
The abdominal aorta as well as the origins of the common iliac arteries and external iliac arteries are compressed by dilated bowel loops however remain patent and there is satisfactory flow distally to the common femoral and superficial femoral arteries.
There is narrowing of the proximal coeliac trunk likely due to compression by the median arcuate ligament. The coeliac trunk and its major branches are otherwise patent. The SMA and IMA are patent.
The distal oesophagus is distended.
The visualised lung bases are clear. No pleural effusions.
Comment: Acute sigmoid volvulus with severe bowel obstruction. The dilated bowel loops are significantly compressing the abdominal aorta and pelvic arteries as above. Urgent surgical review recommended.

Clinical Pearls
This patient has an acute sigmoid volvulus causing abdominal compartment syndrome.
Sigmoid volvulus occurs when the sigmoid colon twists about its mesentery resulting in mechanical obstruction. Ischaemia from impaired bowel wall perfusion can occur if the bowel continues to twist around the point of attachment of the mesentery. The onset of this condition is often insidious and patients present with slowly progressive abdominal pain and distension, nausea, and constipation (1).
The exact cause for sigmoid volvulus remains uncertain, but it is associated with constipation and frequently occurs in patients with neurological and psychiatric illness. It is theorised that chronic faecal overloading may cause elongation of the sigmoid colon, increasing the risk of torsion of that segment of bowel around its narrow mesenteric attachment (1).
Complications of sigmoid volvulus includes large bowel obstruction, ischaemic bowel, bowel perforation and peritonitis and abdominal compartment syndrome. Definitive treatment involves surgical resection of the affected portion of bowel. Detorsion may be attempted initially in stable patients with sigmoidoscopy and rectal tube insertion, but they require resection shortly after due to the high rate of recurrence of volvulus.
Abdominal compartment syndrome (ACS) is defined as new organ dysfunction associated with elevated intra-abdominal pressures (commonly pressures >20mmHg). Pressures are often measured using an indwelling urinary catheter. Primary ACS is due to injury or disease within the abdominopelvic region (eg. pancreatitis, bowel obstruction, abdominal trauma etc). Secondary ACS is caused by conditions that don’t involve the abdomen or pelvis (eg burns, sepsis, excessive fluid administration). (3)
The major organ systems affected in ACS are: cardiac (reduced venous return from IVC compression and reduced cardiac contractility and compliance from diaphragmatic compression); pulmonary (reduced lung compliance from diaphragmatic compression); renal (acute kidney injury from renal vein compression); and gastrointestinal (bowel wall ischaemic due to impaired mesenteric blood flow and impaired venous flow from intestinal walls).
Supportive care is the mainstay therapy for ACS, surgical abdominal decompression may be required in select patients. Supportive care aims to improve abdominal wall compliance and reduce intraabdominal volume. The former is achieved through pain control, sedation and paralysis; the latter through bladder and stomach decompression, and ascitic drainage where applicable. Clinicians should avoid a positive fluid balance after initial resuscitation. (2).
This patient was resuscitated with careful intravenous fluid administration and early initiation of vasopressors and IV Tazocin was given empirically. He was intubated and had an emergency laparotomy shortly after arrival. The laparotomy found a torted sigmoid with a long length of devitalised bowel, and soiling of all abdominal quadrants due to bowel wall perforation. He underwent a Hartmann’s procedure (sigmoidectomy with stoma formation). He was extubated the following day and did not require further vasopressors. His renal function returned to normal on discharge. He had reversal of his Hartmann’s procedure approximately one year later
References
- Le CK, Anand S, Cooper W. Volvulus. 2022 Sep 12. In: StatPearls [Internet]
- Meldrum DR, Moore FA, Moore EE, Franciose RJ, Sauaia A, Burch JM. Prospective characterization and selective management of the abdominal compartment syndrome. Am J Surg. 1997 Dec;174(6):667-72; discussion 672-3
- Malbrain ML et al. Results from the International Conference of Experts on Intra-abdominal Hypertension and Abdominal Compartment Syndrome. I. Definitions. Intensive Care Med. 2006 Nov;32(11):1722-32.
- Hartung MP. Abdominal CT: abdominal arteries. LITFL
- Davidson J. CT Case 044. LITFL
- Cunningham K. Abdominal Imaging Cases 009. CMC
TOP 100 CT SERIES
FACEM, MBBS (Hon), B. Pharm. Emergency Medicine Education Fellow at Liverpool Hospital, Australia. Special interests in clinical education, ECG interpretation and diagnostic ultrasound. Proud father and husband, sadly a golf tragic
Sydney-based Emergency Physician (MBBS, FACEM) working at Liverpool Hospital. Passionate about education, trainees and travel. Special interests include radiology, orthopaedics and trauma. Creator of the Sydney Emergency XRay interpretation day (SEXI).
Dr Leon Lam FRANZCR MBBS BSci(Med). Clinical Radiologist and Senior Staff Specialist at Liverpool Hospital, Sydney



