Eye movements, coma and pseudocoma
aka Neurological Mind-boggler 007
You are reviewing an unconscious patient in the emergency department. Meanwhile, the resus team is preparing to intubate the patient for airway protection prior to facilitate transfer to CT.
See Neurological Mind-boggler 005 for an approach to the differential diagnosis of coma (Q1) and abnormally sized pupils (Q2)
Questions
Q1. What are the 5 key components of the neurological examination of the comatose patient?
Answer and interpretation
According to Posner et al (2008), the key components of the neurological examination of the comatose patient are:
- level of consciousness (Glasgow Coma Score — list the components; e.g. E4V5M6 = GCS 15)
- the pattern of breathing
- size and reactivity of the pupils
- eye movements and oculovestibular responses
- motor responses (tone, reflexes and posturing)
These can be rapidly assessed in a few minutes. I would also add to check for evidence of meningism, and emphasize the search for focal neurological deficits.
General examination is also important — consider the neurological findings in light of the vital signs, evidence of trauma, acute or chronic illness, and/or drug ingestion.
The patient is GCS3, has a slow but otherwise unremarkable pattern of breathing and the pupils are midsized, equal and reactive. Tone and reflexes are normal and there is no abnormal posturing.
Next you assess the patient’s corneal reflexes and spontaneous eye movements.
Q2. What is the significance of the eyes rolling up on corneal stimulation?
Answer and interpretation
Upward rolling of the eyes (with reflexive eyelid closure) on corneal stimulation implies that the pons and midbrain are intact (the reflex pathway involves the trigeminal nerve, the spinal CN5 nucleus, the lateral brainstem tegmentum, and the CN3 and CN7 nuclei — if necessary revise the Brainstem Rules of 4).
If the eye turns upwards but the eyelid does not close there is a CN7 lesion (Bell’s phenomenon).
If the eye does not turn upwards and the eyelid does not close there is a CN5 lesion.
Loss of the corneal reflex is usually a late sign in coma.
To avoid corneal trauma in the unconscious patient, corneal stimulation can be performed by dropping a few drops of sterile saline onto the cornea from a height of 10 cm.
Patients that chronically wear contact lenses may have diminished corneal reflexes.
Q3. What lesion should be suspected if the eyes are tonically deviated to the left?
Answer and interpretation
This is suggestive of either:
- A frontal lobe lesion on the same side as the eye deviation, commonly a stroke.
This can also be a result of a Todd’s paralysis following a seizure (whereas during the seizure the eyes deviate in the opposite direction — away from the origin of the ‘irritative’ focus).
or
- A pontine lesion on the opposite side to the eye deviation.
‘Wrong way eyes’ may also be seen in thalamic hemorrhage.
Lateral gaze deviation from a pontine lesion cannot be overcome by stimulating oculocephalic or ocularvestibular reflexes (see below), whereas supranuclear (e.g. frontal lesions) can. Hence they can be distinguished clinically.
Q4. What lesion should be suspected if there is vertical separation of the ocular axes?
Answer and interpretation
Vertical separation of the ocular axes is called skew deviation. This is suggestive of a pontine or vestibulo-cerebellar lesion on the side of the inferior eye, or a medial longitudinal fasciculus lesion on the side of the superior eye.
On examining the patient’s eyes, he appears to resist eye opening. When opened he has saccadic eye movements. The eyelids once opened stayed open, they did not close smoothly and gradually.
Q5. What are the different types of spontaneous eye movement seen in comatose patients and what do they indicate?
Answer and interpretation
Eye movements seen in the comatose patient include:
- roving eye movements —
Description: slow random predominantly horizontal conjugate eye movements (though there may be a degree of exophoria) similar to those seen in deep sleep.
Likely cause: metabolic encephalopathy (may be absent in deep coma), bilateral supranuclear lesions - ocular bobbing —
Description: Rapid, conjugate, downward movement; slow return to primary position
Likely cause: Pontine strokes; other structural, metabolic, or toxic disorders - ocular dipping —
Description: Slow downward movement; rapid return to primary position
Likely cause: Unreliable for localization; follows hypoxic-ischemic insult or metabolic disorder - reverse ocular bobbing —
Description: Rapid upward movement; slow return to primary position
Likely cause: Unreliable for localization; may occur with metabolic disorders - reverse ocular dipping —
Description: Slow upward movement; rapid return to primary position
Likely cause: Unreliable for localization; pontine infarction and with AIDS - ping-pong gaze —
Description: Horizontal conjugate deviation of the eyes, alternating every few seconds
Likely cause: metabolic encephalopathy, bilateral cerebral hemispheric dysfunction; toxic ingestion - periodic alternating gaze deviation —
Description: Horizontal conjugate deviation of the eyes, alternating every 2 minutes
Likely cause: Hepatic encephalopathy; disorders causing periodic alternating nystagmus and unconsciousness or vegetative state - vertical myoclonus —
Description: vertical pendular oscillations (2–3 Hz)
Likely cause: Pontine strokes - horizontal myoclonus —
Description: rapid horizontal pendular oscillations; the eyes appear to be shaking.
Likely cause: Serotonin toxicity - monocular eye movements —
Description: Small, intermittent, rapid monocular horizontal, vertical, or torsional movements
Likely cause: Pontine or midbrain destructive lesions, perhaps with coexistent seizures
Most individuals have a degree of exophoria when drowsy for any reason and any underlying strabismus tends to worsen — thus dysconjugate gaze is difficult to interpret in the stuporose or comatose patient.
A simplified approach to spontaneous eye movements in coma is:
- roving eye movements — metabolic/ toxic encephalopathy most likely, or although they can also occur with bilateral lesions above the brainstem.
- other ‘weird and wonderful’ eye movements — structural, metabolic or toxicological cause of comas.
- saccadic eye movements or fixing and following — pseudocoma (feigned coma).
Q6. How can pseudocoma (a patient feigning coma) be differentiated from true coma?
Answer and interpretation
Pseudocoma is a diagnosis of exclusion. The following features are consistent with ‘pseudocoma’:
- The pattern of clinical findings are not consistent with a specific neurological syndrome or anatomical lesion.
- Pupils:
- pupils are equal and reactive to light.
- passive eyelid opening results in pupillary constriction, whereas if the patient is sleeping or comatose (with intact pupillary reflexes) the pupils dilate on passive eyelid opening.
- Eye movements and oculovestibular reflexes:
- fluttering of the eyelids when the eyelashes are gently stroked
- the patient may resist passive eye opening. Occasionally patients with metabolic or structural lesions may resist eye opening.
- any spontaneous eye movements are saccadic (rapid and jerking) rather than slowly roving
- the patient actually makes eye contact with the examiner when the eyelids are opened; or the eyes always look to the side away from the examiner, or the eyes always look towards the ground
- the awake patient’s eyes move concomitantly with head rotation when assessing the oculocephalic reflex. It is nearly impossible for an awake patient to mimic the brainstem oculocephalic responses of a truly comatose patient.
- on cold caloric testing the patient may wake up or exhibit preservation of the fast component of nystagmus.
- Motor
- active resistance or varying resistance to passive motor tone testing, or cog-wheeling resistance with sudden “giving-away” phenomena
- no abnormal reflex posturing in response to painful stimuli
- the patient may occasionally make voluntary movements or change body position in bed
- the patient will show avoidance of ‘self injury’ — do not allow the patient to be injured!
Q7. How are oculcephalic and oculovestibular reflexes tested?
Answer and interpretation
Oculocephalic reflex:
- ensure the C-spine is cleared.
- the patient’s eyes are held open.
- the head is briskly turned from side to side with the head held briefly at the end of each turn.
- a positive response occurs when the eyes rotate to the opposite side to the direction of head rotation, thus indicating that the brainstem (CN3,6,8) is intact.
- a similar result is seen when the head is flexed and extended — a positive result is downward deviation of the eyes during extension, and upward deviation during flexion (the eyelids, if closed, may also open as part of the ‘doll’s head phenomenon’). These vertical responses indicates that the brainstem (CN3,4,8) is intact.
- The eyes should gradually return to the mid-position in a smooth, conjugate movement if the brainstem is intact.
Patients with metabolic coma (e.g. hepatic failure) may have exaggerated, brisk oculocephalic reflexes.
Oculovestibular reflex (caloric stimulation):
- the head is elevated to 30 degrees above horizontal so that the lateral semicircular canal is vertical, and so that stimulation with generate a maximal response.
- check that the tympanum is intact and that the external ear canal is clear — C-spine clearance is not necessary.
- introduce iced water into the external ear canal through a small cather until one of the following occurs:
- nystagmus (in the intact brainstem the slow phase is towards the irrigated ear)
- ocular deviation
- 200mL of iced water has been instilled.
- allow 5 minutes between testing ears to allow re-equilibration of the oculovestibular system.
- as consciousness is lost, the fast component (towards the non-irrigated ear) is lost and the slow component tonically deviates the eye in the direction of the irrigated ear.
Vertical oculo-vestibular eye responses can be assessed by irrigated both ears simultaneously. If the brainstem is intact, cold water causes the eyes to deviate downwards and warm water causes the eyes to deviate upwards.
The positive brainstem responses described above are those seen in a comatose patient with an intact brainstem. As described in Q4, results in an awake patient with an intact brainstem may differ…
Brainstem encephalitis, deep metabolic coma and certain drugs may mimic brainstem death. such drugs include recently administered antiepileptics such as phenytoin and barbiturates. Like phenytoin, tricyclic overdose may cause bilateral vestibular failure, as might aminoglycoside vestibulotoxicity. Baclofen overdose can also mimic brain death.
Another caveat pertains to the trauma patient — ocular movements may be impaired if a blowout fracture has trapped the extraocular muscles.
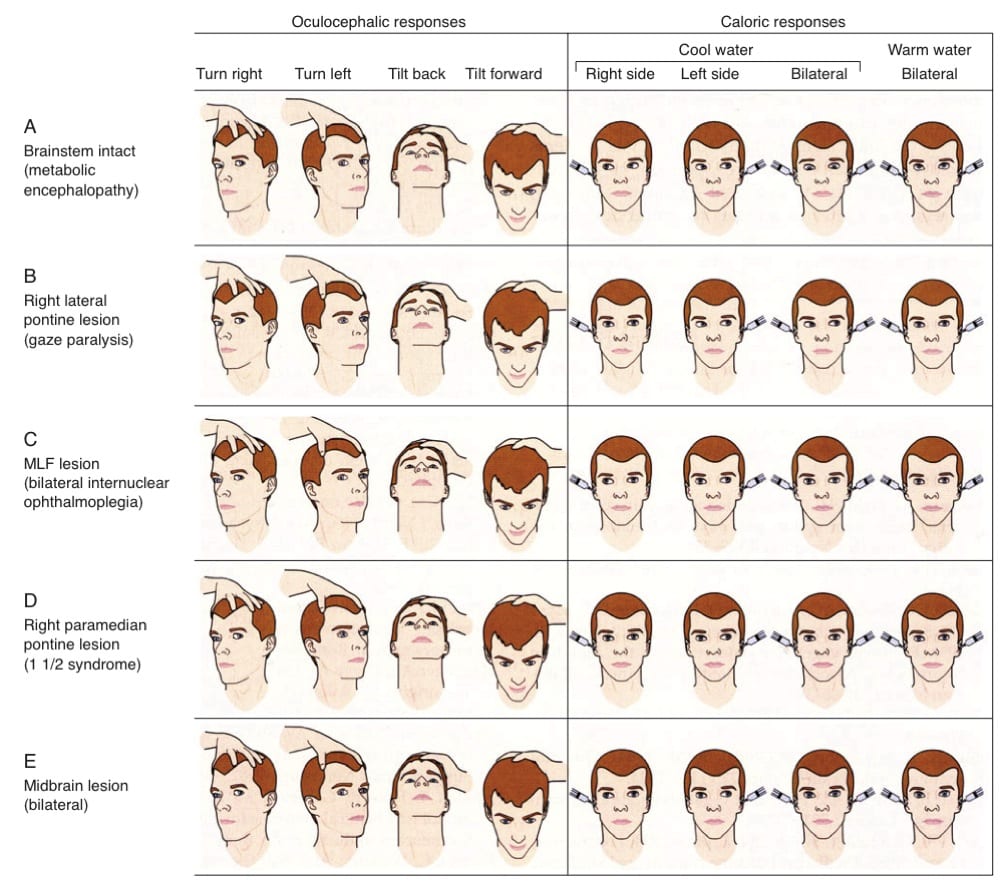
Typical findings for various lesions are shown in this graphic from Posner et al (2008):
Q8. What is Collier’s sign?
Answer and interpretation
Tonically retracted eyelids occasionally seen in patients with dorsal midbrain or pontine lesions.
Now that you know, you can forget about it…
Q9. What are the two most important findings to look for on fundoscopy of the undifferentiated coma patient?
Answer and interpretation
I’d put these two at the top of the list:
- papilloedema —
optic disc swelling due to raised intracranial pressure. However, the absence of papilloedema does not rule out intracranial hypertension… - evidence of Terson syndrome —
vitreous, subhyaloid, or retinal bleeding in association with subarachnoid hemorrhage.
References
- Posner JB, Saper CB, Schiff N, Plum F. Plum and Posner’s Diagnosis of Stupor and Coma 4e Oxford university Press, 2009.
Neurological Mind-boggler
Chris is an Intensivist and ECMO specialist at The Alfred ICU, where he is Deputy Director (Education). He is a Clinical Adjunct Associate Professor at Monash University, the Lead for the Clinician Educator Incubator programme, and a CICM First Part Examiner.
He is an internationally recognised Clinician Educator with a passion for helping clinicians learn and for improving the clinical performance of individuals and collectives. He was one of the founders of the FOAM movement (Free Open-Access Medical education) has been recognised for his contributions to education with awards from ANZICS, ANZAHPE, and ACEM.
His one great achievement is being the father of three amazing children.
On Bluesky, he is @precordialthump.bsky.social and on the site that Elon has screwed up, he is @precordialthump.
| INTENSIVE | RAGE | Resuscitology | SMACC
