Harvey Cushing

Harvey Williams Cushing (1869-1939) was an American author, educator, leader, and neurosurgeon.
One of the greatest American surgeons of all time, Cushing is often regarded as the father of neurosurgery. His relentless work ethic and innovative mind saw him make advances in various fields of medicine beginning from when he was just a medical student.
A prolific author, Cushing published countless works that won countless prizes, even winning the coveted Pulitzer Prize for his biography of William Osler. The prowess and renown Cushing had saw countless students seek his teaching, with the likes of Walter Dandy, Hugh Cairns, and Wilder Penfield being under his tutelage. He was also awarded honorary degrees from nine American and thirteen European universities.
Cushing’s approach to his work saw him receive dichotomous views from his patients and staff. His patients loved him, as he was kind, caring, and ever-present, often tending to patient wounds himself, but his staff felt very much the opposite, being in a constant state of terror due to his intolerance for mistakes and his tendency to work long hours.
Regardless of his methods, Cushing’s achievements speak for themselves. Apart from surgery, he contributed to the fields of anaesthesiology, bacteriology, and medical history. He is eponymous with the Cushing reflex, three different Cushing’s syndromes, Cushing’s disease, Cushing Ulcer, the Bailey-Cushing classification, Neurath-Cushing dyspituitarism, and various surgical instruments.
Biography
- Born April 8, 1869 Cleveland, Ohio descending from a long line of Cushing doctors
- 1887-1891 – Bachelor of Arts, Yale University
- 1891-1895 – Doctor of Medicine, Harvard University
- 1894 – Created the first anesthetic records alongside Ernest Codman
- 1895-1896 – Internship at the Massachusetts General Hospital
- 1896 – Surgical assistant to William Stewart Halsted, Johns Hopkins Hospital
- 1898 – 1900 – Published numerous papers in the field of bacteriology
- 1900 – Studied in Europe with the likes of William Osler, Angelo Mosso, and Thomas McCrae; Coined the term “regional anesthesia”.
- 1901-1911 – Associate professor of surgery at Johns Hopkins Hospital
- 1901 – Described the Cushing reflex
- 1912-1932 – Surgeon-in-chief at the Peter Bent Brigham Hospital, Boston; Professor of Surgery at Harvard Medical School
- 1912 – Described Cushing’s syndrome I and Neurath-Cushing dyspituitarism
- 1915 – Described Cushing’s symphalangism
- 1916 – Published the Bailey-Cushing classification
- 1917 – Commissioned as a major in the US Army Medical Corps, described Cushing’s syndrome II
- 1918 – Promoted to colonel and assigned as a senior consultant in neurosurgery for the American Expedition Forces
- 1925 – Published his Pulitzer Prize-winning biography, “Life of Sir William Osler”
- 1933-1937 – Sterling professor of neurology at Yale Medical School
- 1930 – Described Cushing’s syndrome III
- 1932 – Described Cushing’s disease and the Cushing ulcer
- 1937 – Emeritus professor of neurology at Yale Medical School
- Died October 7, 1939 of coronary thrombosis in New Haven, Connecticut
Medical Eponyms
Cushing Reflex (1901)
The triad of bradycardia, hypertension, and irregular respiration as a physiological response to increased intracranial pressure. Also known as the Cushing effect, the Cushing reaction, the Cushing phenomenon, the Cushing response, Cushing’s triad, and Cushing’s law.
The idea of studying the effects of raised intracranial pressure had been investigated at least 60 years before Cushing, with publications dating back as early as 1835 by Joseph François Malgaigne (1806 – 1865)
1873 – Ernst von Bergmann (1836-1907) and his assistant, Paul Cramer observe the effects of injecting masses of jelly, wax, and sponges into the cranium of dogs. They discover that the increased intracranial pressure resulted in increased arterial pressure and slowing of the pulse. Two individual publications arose from their study, which became the first documented detection of the Cushing reflex.
1901 – Cushing, under the guidance of Emil Kocher (1841-1917), published a study detailing the changes in blood pressure during cerebral compression. The actual primary finding in the study his eponymous reflex is derived from was that the blood pressure will tend to rise until it is at a level that is slightly above the pressure exerted against the medulla. The findings of the effects of raised intracranial pressure on heart rate and respiratory rate (alongside gastrointestinal, urinary, and central nervous system) were a secondary observation, which he noted to be transient in nature.
When, however, the pressure is increased until it exceeds that of the blood pressure and especially if this high intracranial tension has been rapidly produced, we may occasion momentarily the so-called major symptoms of compression with Kussmaul-Tenner spasms, evacuation of bladder and rectum, practical cessation of respiration and pronounced vagus effect upon the heart often with a complete “Stillstand” lasting from ten to twenty seconds. Then follows a release from this extreme vagus inhibition and the vasomotor centre begins to exert its striking influence
Cushing. Concerning a Definite Regulatory Mechanism of the Vaso-Motor Centre which Controls Blood Pressure during Cerebral Compression; 1901: 292
Cushing’s Syndrome I (1912)
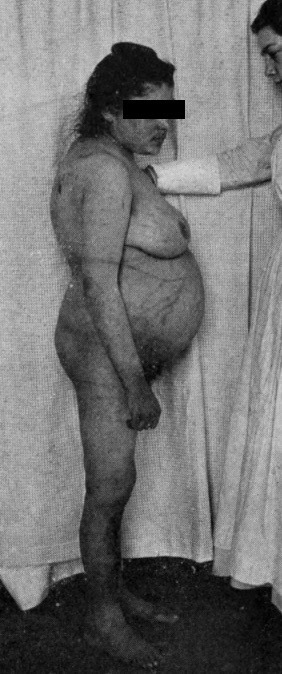
Primarily known as Cushing’s Syndrome. Cushing’s Syndrome is a disorder resulting from excess cortisol exposure. Signs and symptoms include hypertension, abdominal obesity and lipodystrophy, purple striae, osteoporosis, hirsutism and acne. Can be as a result of excess exogenous cortisol exposure, or endogenous production as seen in Cushing’s Disease.
The condition was likely first described by Henry Sampson (circa 1629-1700) in 1695.
1912 – Cushing described a case of a 23-year old woman of Russian origin (named Minnie G.) who had been admitted to the Johns Hopkins Hospital in 1910, identifying characteristic features, and rightly suspected adrenal dysfunction was part of the disease etiology.
Case XLV. (Surgical No. 27140.) A syndrome of painful obesity, hypertrichosis, and amenorrhoea, with over-development of secondary sexual characteristics accompanying a low grade of hydrocephalus and increased cerebral tension…other noteworthy symptoms have been insomnia, tinnitus, extreme dryness of the skin, frequent sore throat, shortness of breath, palpitation, purpuric outbreaks, marked constipation, sudden attacks of dizziness with falling, a definite growth of hair and mustache during the past few years with marked falling out of the hair of the scalp. She feels chilly and cold all of the time and suffers from insomnia rather than from drowsiness. Muscular weakness is extreme and there is much complaint of backache and epigastric pains…other cases with precisely the same syndrome have been recorded in the past…in all of them adenomatous or hyperplastic adrenal tumors have been found and in some instances the constitutional transformation of the afflicted individual into an adipose and hirsute creature has been extraordinary…it will thus be seen that we may perchance be on the way toward the recognition of the consequences of hyperadrenalism.
Cushing. The Pituitary Body and its Disorders; 1912: 216
The eponymous term ‘Cushing’s syndrome’ was introduced to the medical literature by FMP Bishop and RG Close in their 1932 article, A case of basophil adenoma of the anterior lobe of the pituitary: “Cushing’s syndrome”. Fuller Albright, however, would be the one to popularize the eponym when he discussed it during his presentation in the 1943 Harvey Lecture Series; the same lecture series where Albright would be the first to attribute that the syndrome was a result of excess cortisol exposure.
Cushing’s Disease (1932)
A pituitary adenoma that secretes increased amounts of adrenocorticotropic hormone (ACTH) causing excessive cortisol production which results in Cushing’s Syndrome I.
1932 – Alongside possible adrenal dysfunction, Cushing also suspected that the 1912 case of Minnie G. may have also been secondary to pituitary dysfunction as he believed the disease to be a ‘polyglandular syndrome’. It wouldn’t be until 1932, however, where he would associate the symptoms of the syndrome to a pituitary adenoma, observing numerous other cases with the features.
A polyglandular syndrome hither- to supposed to be of cortico-adrenal origin characterized in its full-blown state by acute plethoric adiposity, by genital dystrophy, by osteoporosis, by vascular hypertension, and so on, has been found at autopsy in six out of eight instances to be associated with a pituitary adenoma…the fact that the peculiar polyglandular syndrome, which pains have been taken herein conservatively to describe, may accompany a basophil adenoma in the absence of any apparent alteration in the adrenal cortex other than a possible secondary hyperplasia, will give pathologists reason in the future more carefully to scrutinize the anterior-pituitary for lesions of similar composition
Cushing. The Basophil Adenomas of the Pituitary Body and Their Clinical Manifestations; 1932: 506-507.
Neurath-Cushing Dyspituitarism (1912)
A syndrome characterized by skeletal overgrowth with adiposity and sexual infantilism secondary to hyperpituitarism of the anterior pituitary with hypopituitarism of the posterior pituitary (as seen in a functioning pituitary adenoma for example). Likely a variant of Launois Syndrome.
1911 – Rudolf Neurath (1869-1947) published three cases of tall, obese children with underdeveloped sexual organs in his publication, Über Fettkinder (hypophysäre und eunuchoide Adipositas im Kindesalter).
1912 – Cushing, in his book on pituitary disorders, references Neurath’s cases and presented a similar case of a tall, overweight six-year-old boy with underdeveloped genitalia. He concluded from the clinical features that there is evidence of both hyper- and hypopituitarism.
It is not improbable, therefore, that we have here an instance of anterior lobe activation combined with posterior lobe insufficiency…one of Neurath’s cases is almost the exact counterpart of this case – an overgrown boy of 6 years, with semi-occasional epileptoid attacks, weighing 31.2 kilo. (69 pounds), height 118 cm. (3 feet 11 inches), extremely adipose (abdominal measurements 75 cm.), genital hypoplasia, a large head and a normal sella. Neurath’s two other remarkable cases are somewhat similar, and doubtless the type will come to be a definitely recognizable one.
Cushing. The Pituitary Body and its Disorders; 1912: 178-179
Cushing’s Symphalangism (1915)
Also known as proximal symphalangism. A rare genetic condition characterised by fusion of the mid-phalangeal joints. The elbow, middle ear ossicles, carpal and tarsal bones may also be affected. Clinical features depends on the joints involved, and may include conductive deafness, limited range of motion of the elbow, wrist and ankle joint, brachydactyly and peculiar facies.
1896 – Hector Leboucq (1848-1934) presented a case of a 46-year old with brachydactyly to the Belgian Academy of Medicine.
1900 – Georg Joachimsthal (1863-1914), based on Leboucq’s work, described a case of a 27-year old with brachydactyly, whose siblings also apparently had the deformity.
1915 – Cushing published an abstract detailing his observations over a 10-year period of family members with the condition. He described an autosomal dominant mode of transmission through 7 generations and introduced the term “symphalangism”.
The lesion in the condition under discussion consists of a congenital anchylosis, due apparently to the failure of formation of the joint between MAST the proximal and middle row of phalanges. One or more, often all of the fingers are involved. The resulting deformity is known in the community as ‘stiff fingers,’ in contradistinction to the normal which are called ‘crooked fingers.’ This condition has been transmitted through seven generations, the progenitor of the family having migrated from Scotland to Virginia in 1700. There are connections of the family still in Scotland who carry the trait.
Cushing. Hereditary Anchylosis of the Proximal Phalangeal Joints (Symphalangism); 1915: 621-622
Cushing’s Syndrome II (1917)
A syndrome consisting of multiple tumors of the spinal nerve roots and auditory nerves. Clinical features include hearing loss, tinnitus, vertigo, ipsilateral paralysis of the sixth and seventh cranial nerves, hyperaesthesia of the face, headache, vomiting, and dimness of vision. Associated with von Recklinghausen disease and other nervous system abnormalities.
The condition was first described by John Henry Wishart (1781-1834) in 1822.
1917 – Cushing published a book detailing 33 cases of patients with acoustic nerve and cerebellopontine angle tumors. The book also detailed possible etiology, symptomatology, pathological anatomy, surgical management, and operative technique for the tumors.
Acoustic tumors apparently arise from embryonic tissue rests in the peripheral end of the nerve and their growth may possibly be influenced by such elements as trauma, local infection, or pregnancy. From the present series they appear to be somewhat more common in women and more often on the left side. The average age of onset has been 34 years…the primary diagnosis, which was usually “glioma” because of the demonstration of supposed glia fibrils, had in almost all cases been subsequently shifted to “endothelioma,” doubtless because of my insistence from the clinical side that these were extracerebellar and benign lesions and could therefore have no relation to the gliomas, for they never extended by infiltration.
Cushing. Tumors of the Nervus Acusticus and the Syndrome of the Cerebellopontile Angle. 1917: 151,196
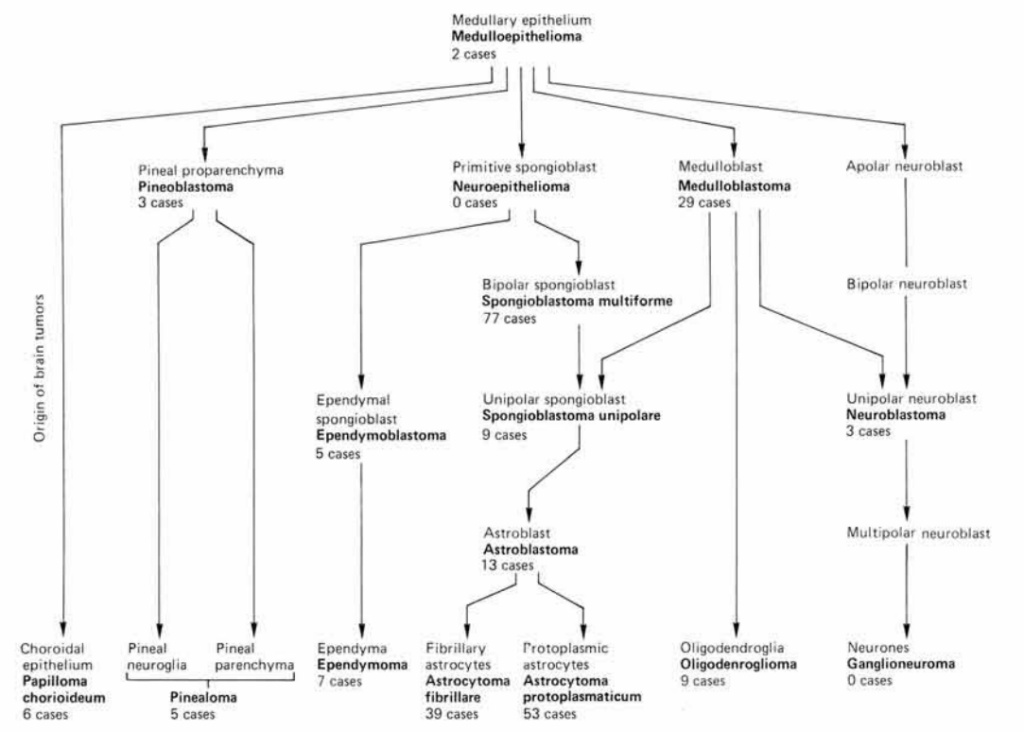
Bailey-Cushing classification (1926)
A classification which stratifies gliomas on a histogenetic basis.
1922 – Percival Bailey, under the instruction of Cushing, created a histological laboratory for the study of Cushing’s collection of brain tumours.
1924 – Bailey presented Cushing with a complete classification of the glioma group. The two disagreed with timing of publishing the classification, with Bailey wishing to publish an individual paper on each group member and Cushing wishing to urgently publish the classification as a whole
1926 – Whilst Bailey was away in Paris, Cushing took his preliminary report, added a chapter on clinical correlation, and sent it to be published. Bailey initially reacted with horror, but over time came to view the events with understated humour.
Cushing’s Syndrome III (1930)
A syndrome of progressive primary optic atrophy with bitemporal hemianopsia secondary to a suprasellar tumor.
1930 – Cushing, building on his 1923 paper on optic gliomas with Paul Martin, notes several cases of an atypical chiasmal syndrome. He performed exploratory surgery to investigate the newfound syndrome and identified the cause to be secondary to a suprasellar tumor.
Certain of these suprasellar tumors, more particularly the meningiomas that arise from the membrane over the sulcus chiasmatis, prove to be most favorable for operative removal. The characteristic syndrome of these tumors of primary atrophy with bitemporal field defects in adult patients with an essentially normal sella may be simulated not only by other tumors (adenomas, chiasmal gliomas, craniopharyngiomas, etc.), but by a variety of conditions which with further study should be capable of clinical differentiation without the necessity of an exploratory operation.
Cushing. The Chiasmal Syndrome of Primary Optic Atrophy and Bitemporal Field Defects in Adults with a Normal Sella Turcica; 1930: 735
Cushing Ulcer
Also known as von Rokitansky-Cushing ulcer. A gastric ulcer believed to be caused by oversecretion of gastric acid, secondary to direct stimulation of the vagal nuclei from raised intracranial pressure. Treatment includes decreasing intracranial pressure, anti-acid medications such as proton-pump inhibitors, and vagotomy.
1842 – Karel Rokitansky described in detail multiple cases of acute perforating ulcers. He also described a “softening” of the stomach lining and attributed this to stimulation of the vagus nerve.
1932 – Cushing detailed case reports of patients presenting with epigastric pain and vomiting coupled with an intracranial brain tumor who unexpectedly died of perforated peptic ulcers. Puzzled by the pathogenesis of these peptic ulcerations and perforations, Cushing proposed several theories, one of which involved advancing Rokitansky’s theory by speculating disturbance of vagal centers in the brainstem.
What has incited my interest in the subject has been the disturbing experience of having lost three patients from acute perforations of the upper alimentary canal soon after what appeared to be successful operations for the removal of intracranial tumors, and that each of these tumors happen to be situated in a cerebellum could not it seems to me be other than some significance…extrapyramidal lesions anywhere from the intracranial course of these fiber tracts from the anterior hypothalamus to vagal center, presumably from parasympathetic stimulation within, or possibly from vagal release due to sympathetic paralysis are prone to cause gastric erosions, perforations, or ulcers. Intracranial injuries and diseases affecting these same basilar regions of the brain are known to be accompanied by ulcerative lesions of the upper alimentary canal. It is reasonable to believe, therefore, that the perforations following the cerebellar operations forming the base of this study were produced in like fashion by an irritative disturbance either of fiber tracts or vagal centers in the brainstem
Cushing. Peptic Ulcers and the Interbrain; 1932: 2,32
Surgical Instruments
Cushing is eponymous with various surgical instruments. These include:
Cushing tissue forceps – a pair of light to medium weight straight thumb forceps with a narrow tip. Used on delicate tissue and in small surgical areas.

Cushing artery forceps – a pair of scissor-like, ratcheted finger ring instruments with a half-serrated jaw grip and blunt tip. Commonly used for control of blood flow during neurological procedures.

Cushing pituitary rongeurs – a pair of angulated rongeurs originally used to remove brain tumors. Now commonly used to remove intervertebral discs and tissue during spinal surgery.

Cushing brain spoon retractors – a spoon-shaped, round-edged retractor that is commonly double-sided. Cushing first used these retractors as an alternative to the flat, sharply edged retractors to cause less damage to the cortical vessels in 1909.

Cushing vein retractors – a retractor with teardrop, fenestrated handle that tapers into a sharply curved blade. Commonly used to retract veins or other small tissues.

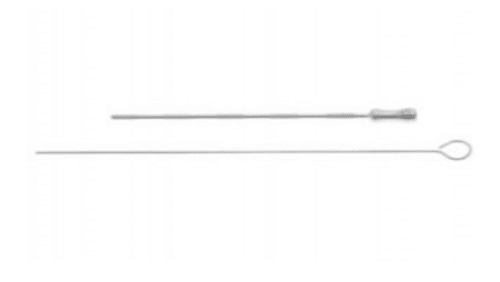
Cushing-Cairns ventricular cannula – developed with his resident at the time, Hugh Cairns. A sharp, thin metal cannula with a stylet. Commonly used for ventricular drainage.
Key Medical Attributions
Developing the first anaesthesic records
When he was a student at the Massachusetts General Hospital in 1894, Cushing, alongside fellow student Ernest Amory Codman (1869-1940), developed the first consistent recording of physiological variables during anaesthesia using observed respiratory rate and palpated pulse rate as initial parameters. He would later add blood pressure as an additional parameter in 1901 after his discovery of the Riva-Rocci sphygmomanometer and be instrumental in its adoption as a vital sign.
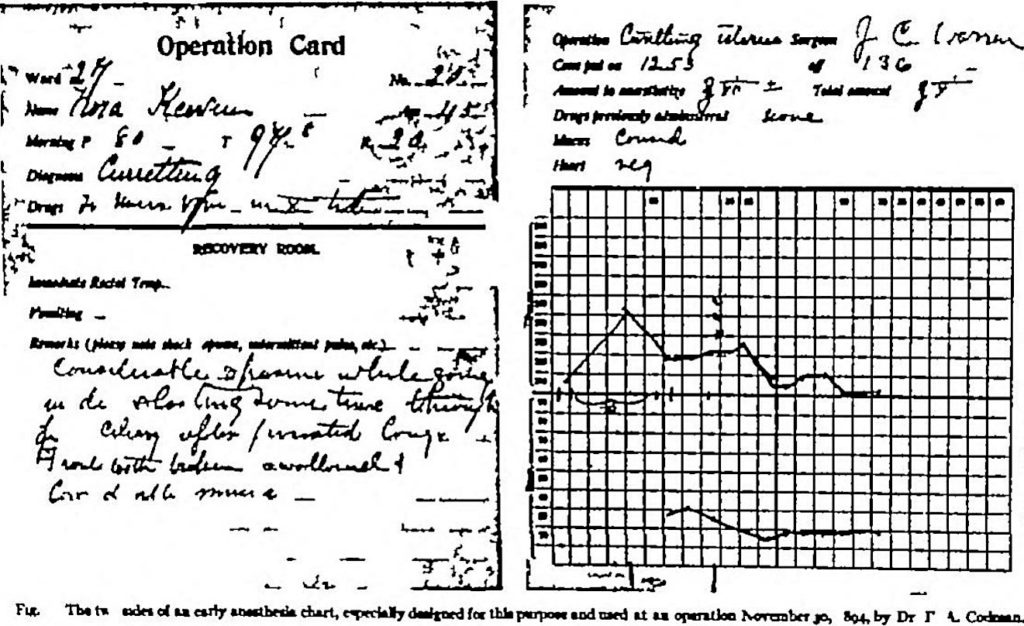
Years later, Cushing explained the reason for developing the records was to minimize fatalities; something he saw first-hand when he would be asked to anaesthetize patients.
I hesitate to recall what an awful business it was and how many fatalities there were. My first giving of an anaesthetic was when, a third-year student, I was called down from the seats and sent in a little side room with a patient and an orderly and told to put the patient to sleep. I proceeded as best I could under the orderly’s directions. The operation was started…there was a sudden great gush of fluid from the patient’s mouth, most of which he inhaled and he died. I stood aside, burning with chagrin and remorse. No one paid the slightest attention to me, although I supposed that I had killed the patient. To my perfect amazement I was told it was nothing at all, that I had nothing to do with the man’s death…and that sort of thing happened frequently and I had better forget about it and go on with the medical school I went on with the medical school but I have never forgotten about it…Codman and I resolved that we would improve our technique of giving ether. We made a wager of a dinner as to who could give the best anesthesia. We both became very much more skillful…than we otherwise would have become but it was particularly due to the detailed attention which we had to put upon the patient by the careful recording of the pulse rate throughout the operation.
Cushing 1895. From Letter to F A Washburn Anaesthesia Charts of 1895.
Coining the term “regional anaesthesia”
In 1896, after starting residency at Johns Hopkins Hospital, Cushing learned the method of infiltrational anaesthesia from William Halstead. Understanding the utility of it, Cushing implemented this novel method of anesthesia to his surgical work where he could. He introduced the term “regional anaesthesia” in 1900 to describe pain relief by nerve blocks using cocaine, however interchanged it readily with the term “local anaesthesia”.
“Since our first cocaine operation…233 herniotomies have been performed, forty-nine of them under regionary anaesthesia… in the majority of them the administration of ether or chloroform seemed inadvisable or positively contraindicated, whereas, in the remainder, the local anaesthetic was employed at the patient’s personal request…the ilio-inguinal nerve emerges from the external ring, and near by, or also through the ring, the genital branch of the genito-cural appears…the early cocainization of which at the deeper part of the canal…is perhaps the most important step of the operation.”
Cushing. The Employment of Local Anæsthesia in the Radical Cure of Certain Cases of Hernia, with a Note upon the Nervous Anatomy of the Inguinal Region; 1900: 1, 25.
Contributions to bacteriology
From the period of 1898-1900, during his residency at Johns Hopkins Hospital, Cushing developed a keen interest in bacteriology and published a number of significant papers in the field. During this time he:
- demonstrated that typhoid fever could result in gallstones (1898)
- pioneered surgical treatment of intestinal perforation in typhoid fever (1898)
- proved that gonococcus could cause peritonitis (1899)
- studied Bacillus enteritidis (Gartner type) and compared it with other pathogenic microorganisms of the gastro-intestinal system (1900)
- alongside Louis Livingood (1868-1895), studied the bacteriology of the alimentary canal which highlighted the importance of fasting before upper gastrointestinal surgery to reduce the risk of peritonitis (1900)
Cushing’s publication on the alimentary canal was particularly highly acclaimed, with William Welch even commenting to Cushing:
Your paper is of very great value and I confess that I had not realized how thorough a study you had made of the bacterial flora of the intestine under varying conditions. Your observations are certainly of great practical importance, as well as of scientific interest
Quote from William Henry Welch to Harvey Cushing, May 14, 1900. Harvey Cushing Papers, Microfilm Reel 127
Addressing the issue of haemorrhage during surgery
One of the issues Cushing faced was the haemorrhage commonly seen when operating on the heavily vascularized skull. To circumvent this, Cushing developed a number of tools. The first would be the ‘silver clip’ in 1911, which was used for the occlusion of blood vessels that could not be ligated.
Cushing then worked with physicist William T. Bovie to develop a more efficient electrocautery system. He performed the first operation utilising this system in 1926.
”…with Dr Bovie’s help I proceeded to take off most satisfactorily the remaining portion of the tumour with practically none of the bleeding which was occasioned in the preceding operation. The loop acted perfectly and blood stilling was almost complete but whether we would venture to use anything of this kind in the brain tissue itself I am at a loss to know because almost certainly it would cause convulsion.”
Segment from Harvey Cushing’s operative notes on October 1st, 1926. From Fulton. Harvey Cushing A Biography: 1946; 538.
Thanks to the efforts of Cushing, mortality rates from intra-operative haemorrhage dropped from nearly 50% to less than 10%.
Pioneering post-operative care
Cushing was one of the first to introduce focused care for his post-operative patients, with each of his patients being cared for by a team of specialized staff. He introduced strict observation systems and record-keeping and was the first to use x-rays and blood pressure monitoring extensively. Some credit these efforts to be the blueprints for post-operative intensive care.
“Not all surgeons would pay that much attention to the patient once they’d completed their operation, Cushing carried over his meticulousness during surgery to the post-operative care of the patients. Cushing’s whole ward was more like an intensive care unit than other surgeon.”
Quote from Dennis Spencer. Hollingham 2020. How intensive care units were born.
Prolific author and biography of William Osler
During his time, Cushing was the author of 14 books; 9 related to neurologic surgery and diseases and 5 pertaining to history and war. From the period of 1898 to 1939 alone, he published 330 articles and held many lectures and addresses. It is estimated by his biographer, John Fulton (1899-1960), that Cushing averaged writing 5,000 to 10,000 words per day.
In 1925, Cushing published two volumes detailing the life of Sir William Osler. Containing forty-seven original illustrations and written in a manner the layman could understand, Cushing’s work would become renown as one of the greatest of medical biographies ever written, winning him the Pulitzer Prize in 1926.
Establishing the medical library of Yale University
Cushing, alongside Arnold Klebs (1870-1943) and John Fulton and under the moniker of “The Trinitarians”, donated their extensive library collections to Yale to form the nucleus of one of the greatest medical historical libraries of the world. The library opened its doors for the first time in 1941, two years after Cushing’s death. It is estimated that Cushing personally left approximately 8,000 items, many of which were of great rarity.
Controversies
Lost eponyms
Although historically, there may have been three different eponymous syndromes of Cushing (I, II, III), the modern medical literature does not seem to retain Cushing Syndrome II and III as eponymous terms. Similarly, whilst Cushing’s Syndrome I may be the same entity as Apert-Gallais syndrome, the latter eponym is sparsely used in the modern medical literature.
Plagiarism claims regarding Cushing’s reflex
Controversy concerning plagiarism surrounds some of Cushing’s research on his eponymous reflex. Bernhard Naunyn (1839-1925), a contemporary of Cushing, made remarks claiming that Cushing neither cited him in Cushing’s research nor expanded on any of the results that Naunyn had found in his original experiments.
Zwischenein ging in Königsberg die grosse experimentelle Hirndruckarbeit vom Stapel, die ich 1881 mit Schreiber publizierte. Ich habe immer viel von ihr gehalten, doch wuchs mein Selbstgefühl gewaltig, als 1902 Cushings Arbeit über den Gleichen Gegenstand erschien. Cushing ist tatsächlich an keener Stelle über uns hinausgekommen. Das ser es dabei fertig gebracht hat, unsere Arbeit mit keinem Worte zu erwähnen, hat mich erstaunt, obgleich sie bei Kocer gemacht war…
Nanyun on Cushing’s study of intracranial pressure. Fulton 1946. Harvey Cushing. A Biography; 192;28
In the meantime, the extensive experimental work on intracranial pressure took place by Stapel in Konigsberg, which I published in 1881 with Schreiber. My self-confidence increased tremendously when in 1902 Cushing’s work about the same subject appeared. Cushing has under no circumstances added anything new to our results. The fact that he does not mention our work with a single word surprised me, even if it was done with Kocher…
Nanyun on Cushing’s study of intracranial pressure. Fulton 1946. Harvey Cushing. A Biography; 192;28
Major Publications
- Cushing H. An improved method for the radical cure of femoral hernia. 1889
- Cushing H. The “right angle” continuous intestinal suture. 1889
- Cushing H. Haematomyelia from gunshot wounds of the spine. 1898
- Cushing H, Livingood LE. Experimental and surgical notes upon the bacteriology of the upper portion of the alimentary canal; with observations on the establishment there of an amicrobic state as a preliminary to operative procedures on the stomach and small intestine. 1899
- Cushing H. The Employment of Local Anaesthesia in the Radical Cure of Certain Cases of Hernia, with a Note upon the Nervous Anatomy of the Inguinal Region. 1900
- Cushing H. Concerning a definite regulatory mechanism of the vaso-motor centre which controls blood pressure during cerebral compression. 1901 [Cushing reflex]
- Cushing H. A method of combining exploration and decompression for cerebral tumors which prove to be inoperable. 1909 [Cushing brain spoon retractors]
- Cushing H. The Control of Bleeding in Operations for Brain Tumors. 1911
- Cushing H. The pituitary body and its disorders. 1912 [Cushing syndrome I, Neurath-Cushing syndrome]
- Cushing H. Hereditary anchylosis of the proximal phalangeal joints (symphalangism). 1915 [Cushing’s symphalangism]
- Cushing H. Tumors of the nervus acusticus and the syndrome of the cerebellopontile angle. 1917 [Cushing syndrome II]
- Cushing H. The life of Sir William Osler. 1925
- Bailey P, Cushing H. A classification of the tumours of the glioma group on a histogenetic basis, with a correlated study of prognosis. 1926 [Bailey-Cushing classification]
- Cushing H. The chiasmal syndrome of primary optic atrophy and bitemporal field defects in adults with a normal sella turcica. 1930
- Cushing H. The basophil adenomas of the pituitary body and their clinical manifestations. 1932 [Cushing disease]
- Cushing H. Peptic ulcers and the interbrain. 1932 [Cushing ulcer]
- Cushing H. From a surgeon’s journal: 1915-1918. Boston, 1936
References
Biography
- Editorial: Harvey Cushing. N Engl J Med. 1939;221:623-625.
- Cannon WC. Harvey (Williams) Cushing 1869-1939. Obit. Not. Fell. R. Soc.1941; 3(9): 277–290.
- Holman E. Sir William Osler, William Stewart Halsted, Harvey Cushing: some personal remembrances. Surgery. 1965;57:589-601.
- Laws ER Jr. Neurosurgery’s man of the century: Harvey Cushing–the man and his legacy. Neurosurgery. 1999 Nov;45(5):977-82.
- Haas LF. Harvey Williams Cushing (1869-1939). J Neurol Neurosurg Psychiatry. 2002 Nov;73(5):596.
- Ellis H. Harvey Cushing: a founding father of neurosurgery. Br J Hosp Med (Lond). 2009 Oct;70(10):600.
- Bruce SS, Bruce JN. Harvey Cushing, neurosurgical pioneer. Curr Surg. 2005 Jan-Feb;62(1):138-40.
- Fresquet JL. Harvey Williams Cushing (1869-1939). Historia de la Medicina
Eponymous terms
- Lisser H. Absence of the prostate associated with endocrine disease, notably hypopituitarism; with histories of eighteen cases. Endocrinology. 1923 Mar;7(2):225–255
- Bailey OT. Genesis of the Percival Bailey-Cushing classification of gliomas. Pediatr Neurosci. 1985-1986;12(4-5):261-5.
- Medvei VC. The history of Cushing’s disease: a controversial tale. J R Soc Med. 1991 Jun;84(6):363-6.
- Loriaux DL. Harvey Williams Cushing (1869–1939). The Endocrinologist 1992;2(1):2–5.
- Lindholm J. Cushing’s syndrome: historical aspects. Pituitary. 2000 Oct;3(2):97-104.
- Voorhees JR, Cohen-Gadol AA, Laws ER, Spencer DD. Battling blood loss in neurosurgery: Harvey Cushing’s embrace of electrosurgery. J Neurosurg. 2005 Apr;102(4):745-52.
- Harvey Cushing: A Journey Through His Life. February 2006. Historical Library, Cushing Whitney/Medical Library
- Kim OJ. Experimental sciences in surgery: Harvey Cushing’s work at the turn of the twentieth century. Uisahak. 2006 Jun;15(1):49-76.
- Fodstad H, Kelly PJ, Buchfelder M. History of the Cushing reflex. Neurosurgery. 2006 Nov;59(5):1132-7.
- Molnár C, Nemes C, Szabó S, Fülesdi B. Harvey Cushing, a pioneer of neuroanesthesia. J Anesth. 2008;22(4):483-6.
- Wijdicks EF. Cushing’s ulcer: the eponym and his own. Neurosurgery. 2011 Jun;68(6):1695-8.
- Assina R, Rubino S, Sarris CE, Gandhi CD, Prestigiacomo CJ. The history of brain retractors throughout the development of neurological surgery. Neurosurg Focus. 2014 Apr;36(4):E8.
- Bliss M. Harvey Cushing: A Life in Surgery. Oxford University Press
Eponym
the person behind the name
Lewis is an RMO at Royal Perth Hospital. He is currently interested in critical care medicine.
