Headache secondary to medical conditions
Analyzing underlying medical conditions
Secondary headaches are, by definition, due to associated medical conditions. Three severe conditions, often associated with headache are:
- Giant cell arteritis
- Tumours
- Idiopathic intracranial hypertension or pseudotumour cerebri
Giant cell arteritis
Giant cell arteritis is an example of one such condition. It is a serious inflammatory disorder affecting the extracranial carotid artery. It is most often seen in individuals over the age of 60, although it can be seen in individuals as early as age 50.
The headache of giant cell arteritis is often located over the temples. It is dull and achy and can be bilateral or unilateral. Fatigue or discomfort in jaw muscles (i.e., jaw claudication) with chewing hard or chewy items is a classic finding, along with weight loss and myalgia.
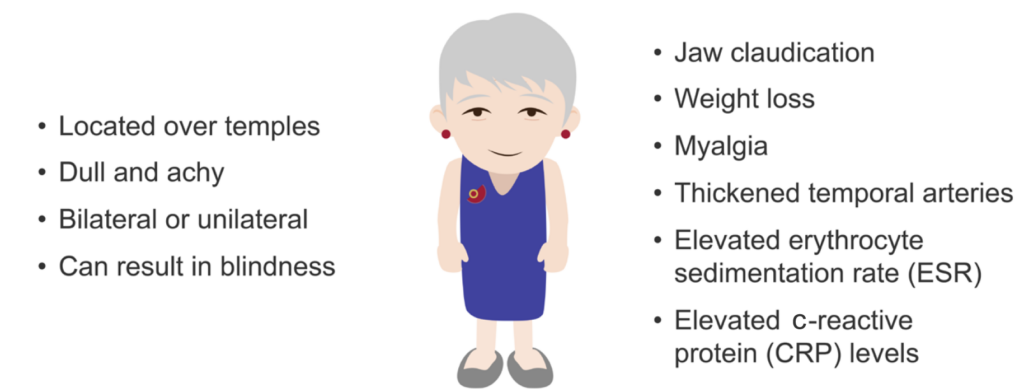
On examination, you’ll find temporal arteries that are often thickened and have either a reduced pulse or are pulseless. Labs will reveal elevated erythrocyte sedimentation rate (ESR) and c-reactive protein (CRP) levels. Temporal artery biopsy is diagnostic.
When the disease affects the ophthalmic artery, blindness can result if not treated. This is the region involved in about 50% of those affected.
Giant cell arteritis is treated with high dose steroids. Prompt treatment can prevent blindness.
Tumours
Patients with headaches often worry that they may have a tumour, but tumours are actually a rare cause of severe headaches. Usually a tumour will present with other focal neurological complaints or signs.
There are three major clues that a headache may actually be related to a tumour:
- Worsening of the headache with exertion or a change in position
- Increased pain at night which awakens a patient from sleep
- A drastic change in an established headache pattern
The headache pain from a tumour is generally nondescript holocranial pain, and is often described as dull, achy, and intermittent.
In a patient with a known cancer, a new headache warrants imaging with magnetic resonance imaging (MRI), both with and without contrast.
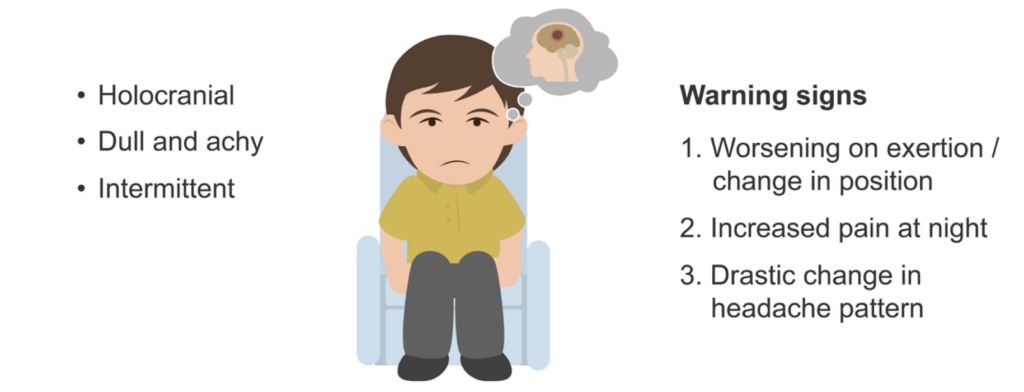
Steroids can decrease the swelling of surrounding brain tissues, which can help to ameliorate headache and other neurologic dysfunction until the tumour can be treated with more specific measures such as surgery or radiation.
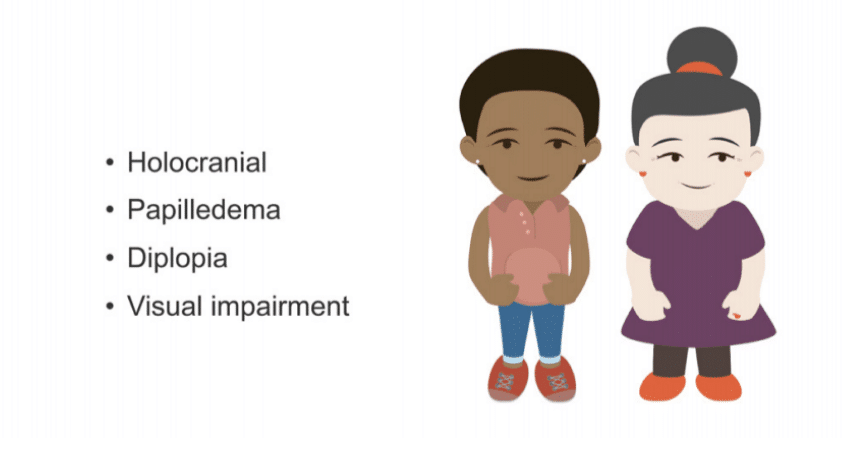
Idiopathic Intracranial Hypertension
Idiopathic intracranial hypertension or pseudotumor cerebri
Idiopathic intracranial hypertension is also called pseudotumour cerebri. It involves diffusely increased intracranial pressure from generalised oedema with headache characteristics similar to those seen with tumours. Papilloedema is typical on fundoscopic examination, and many patients have diplopia. Untreated, it can lead to visual impairment.
Women of childbearing age are affected more frequently, and most are obese.
Treatment is multifaceted, and includes acetazolamide (an oral carbonic anhydrase inhibitor), loop diuretics, weight reduction, serial lumbar punctures, surgical correction with optic nerve fenestration surgery, and lumbar-peritoneal or ventriculoperitoneal shunts.
This is an edited excerpt from the Medmastery course Headache Masterclass by Robert Coni, DO, EdS, FAAN. Acknowledgement and attribution to Medmastery for providing course transcripts.
- Coni R. Headache Masterclass. Medmastery
- Coni R. Clinical Neurology Essentials. Medmastery
- Simmonds GR. Neurology Masterclass: Managing Common Diseases. Medmastery
- Simmonds GR. Neurology Masterclass: Managing Emergencies. Medmastery
References
- The International Classification of Headache Disorders 3rd edition
- Chou DE. Secondary Headache Syndromes. Continuum (Minneap Minn). 2018 Aug;24(4, Headache):1179-1191
- Green MW. Secondary headaches. Continuum (Minneap Minn). 2012 Aug;18(4):783-95.
- Tsakadze, N, Antonovich N, Rossi F. Medication-overuse headache. Practical Neurology. 2018; 17: 50–52.
Neurology Library: Secondary headaches
- Coni R. Secondary headaches. LITFL
- Coni R. Sinus headaches. LITFL
- Coni R. Muskuloskeletal pain and headache. LITFL
- Coni R. Temporomandibular joint and headache. LITFL
- Coni R. Medication overuse headache. LITFL
- Coni R. Thunderclap headache. LITFL
Neurology Library
Robert Coni, DO, EdS, FAAN. Vascular neurologist and neurohospitalist and Neurology Subspecialty Coordinator at the Grand Strand Medical Center in South Carolina. Former neuroscience curriculum coordinator at St. Luke’s / Temple Medical School and fellow of the American Academy of Neurology. In my spare time, I like to play guitar and go fly fishing. | Medmastery | Linkedin |
BMBS (The University of Nottingham) BMedSci (The University of Nottingham). Emergency Medicine RMO at Sir Charles Gairdner Hospital Perth, WA. Interested in Medical Education and Emergency Medicine. Swimmer and frequent concert attendee.


