High Altitude illness
OVERVIEW
High altitude illness includes:
- acute mountain sickness
- high altitude cerebral edema (HACE)
- high altitude pulmonary edema (HAPE)
- high altitude retinal haemorrhage
PATHOPHYSIOLOGY
The cause of AMS and HACE is not entirely understood
- A vasogenic mechanism is thought to be responsible for the cerebral oedema. Hypoxia-induced cerebral vasodilation and alteration of the permeability of cerebral capillaries are likely causes.
- Cytotoxic oedema may also play a role, with failure of the Na+-K+ ATPase due to oxygen radicals.
HAPE is caused by heterogenous hypoxia-induced pulmonary vasoconstriction
- HAPE prone individuals exhibit greater rises in their pulmonary artery pressure at altitude.
- The heterogeneity of the the response causes diversion of flow to the less constricted areas with subsequent capillary leakage.
- Diminished reabsorption of alveolar fluid is also likely to be important, with hypoxia inhibiting Na+ transport across the alveolar membrane.
PREVENTION
Slow ascent is the best prevention.
- “Above an altitude of 3000 m, individuals should not increase the sleeping elevation by more than 500 m per day and should include a rest day (ie, no ascent to higher sleeping elevation) every 3 to 4 days.” — Luks et al (2010)
- ‘Sleep low, climb high’ — ideally, sleep at less than 2500m altitude on the first night, and sleep at a lower altitude than the altitude reached during the day.
AMS/ HACE prevention
- Acetazolamide is the most effective prophylaxis. It is a carbonic anhydrase inhibitor that causes a bicarbonate diuresis and metabolic acidosis. It increases the hypoxic ventilatory response, decreases CSF production and may also have effects on the perripheral chemoreceptors. It is usually well tolerated. Side effects include paraesthesia and metallic taste.
- Dexamethasone has been shown to be effective in the prevention of AMS, although it is usually reserved for short exposures (<4 days) to altitude due to its side effects.
- Ginkgo biloba has shown conflicting results, although recent studies suggest it is no better than placebo.
- Other simple measuresthat may be beneficial include:
- avoiding over-exertion
- avoidance of alcohol and smoking
- eating a high carbohydrate diet
- ensuring adequate hydration.
- Acetazolamide showed be used in those of moderate risk of AMS — individuals who have had AMS before or need to ascend more rapidly than the suggested safe rate. Dexamethasone may be used in those intolerant of acetazolamide. Both drugs may be used in high risk individuals (e.g. previous HAPE or HACE, very rapid and high ascents). drug prophylaxis should be continued until descent or until 3 days have been spent at peak altitude.
Consult Luks et al (2010) to assess an individual’s risk of developing AMS, HACE and HAPE.
HAPE prevention
- Pulmonary artery pressure can be reduced by nifedipine or the phosphodiesterase inhibitorssildenafil and tadalafil. Both have been shown to decrease the incidence of HAPE when taken as prophylaxis.
- Salmeterol decreases the risk of HAPE by increasing alveolar fluid clearance through its action on Na+ transport.
- According to Luks et al (2010): “Drug prophylaxis should only be considered for individuals with a prior history of HAPE and nifedipine is the preferred option in such situations. It should be started on the day prior to ascent and continued either until descent is initiated or the individual has spent 5 days at the target elevation.”
Early recognition of AMS, so that ascent is stopped, may prevent the development of HAPE and HACE.
ACUTE MOUNTAIN SICKNESS
- Acute mountain sickness (AMS) is rare below altitudes of 2500m.
- It is similar to a bad hangover and is characterised by headache plus one or more of these other symptoms: nausea and/or vomiting, fatigue, lassitude, dizziness, and difficulty sleeping.
- Risk factors include:
- previous AMS
- rapid ascent
- higher altitudes
- strenuous physical exertion
- Recent altitude exposure can be protective. There is no simple way to identify who will suffer from AMS prior to arriving at altitude. Those over 50 years of age may be less prone to AMS than younger people.
HACE
- High-altitude cerebral oedema (HACE) is a potentially fatal condition and represents the severe end of the AMS spectrum.
- It usually occurs over 3000m, with an estimated prevalence between 0.5% – 1.5% at altitudes between 4000-5000m.
- Symptoms include severe headache, confusion, ataxia, drowsiness, stupor and coma.
- Ataxia is the most sensitive sign, and should be considered an indication for descent.
HAPE
High-altitude pulmonary oedema (HAPE) is the leading cause of death related to high altitude.
- HAPE usually occurs within the first 2-4 days of ascent to high altitudes.
- It is characterised by decreased exercise capacity, dry cough, cyanosis, dyspnoea at rest and pink, frothy sputum.
- HAPE and HACE can occur together.
MANAGEMENT The best treatment for AMS, HACE and HAPE is descent.
- Mild AMS can be treated with stopping ascent for 24 hours, acetazolamide and simple analgesia. Once symptoms resolve ascent may continue, but at the risk of recurrence.
- Severe AMS or HACE should be treated with descent, supplemental oxygen, portable hyperbaric chamber if available, acetazolamide and dexamethasone.
- HAPE should be treated with, again, descent, supplemental oxygen and portable hyperbaric chamber. Nifedipine is the drug of choice — sildenafil/tadalafil may be used if nifedipine is unavailable, but concurrent use vasodilators is not recommended. Use CPAP as an adjunct if available. There is no established role for acetazolamide, beta-agonists, or diuretics in the treatment of HAPE.
A patient with HAPE and HACE can be given the respective treatments for each condition simultaneously. However, the following should be considered:
- altered mental state in a patient with HAPE may be due to hypoxia. Commence treatement for HACE with dexamethasone if the patietn’s neurological status doesn’t promptly improve with the administration of supplemental oxygen.
- treatment of HAPE with nifedipine will decrease the patients mean artial pressure. This will decrease cerebral perfusion pressure and may lead to cerebral ischemia in the patient with HACE. Tread carefully!
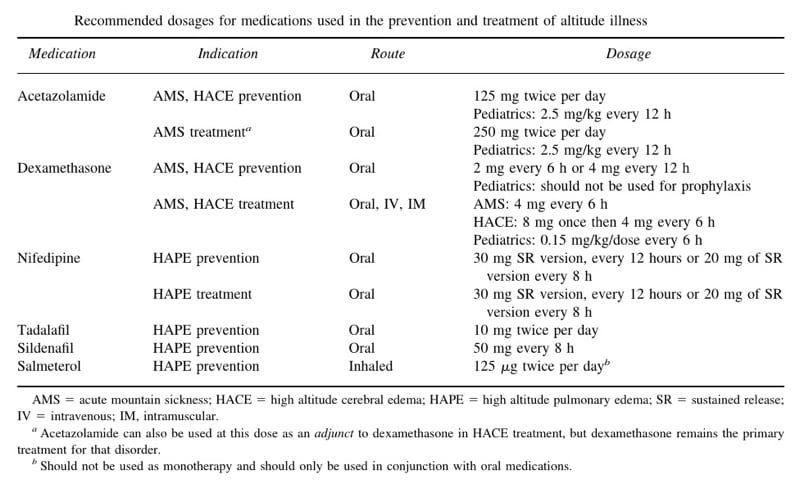
DRUG DOSES The Wilderness Medical Society Consensus Guidelines for the Prevention and Treatment of Acute Altitude Illness by Luks et al (2010) contains this handy table:
HIGH ALTITUDE RETINAL HAEMORRHAGES
- High altitude retinal hemorrhages are more common at altitudes above 5000m.
- They are usually asymptomatic and typically resolve over a few weeks.
- They may be found in HAPE and HACE, as well as the otherwise well person.
- Central scotomata can occur if the macula is involved.
References and Links
LITFL
- Pulmonary Puzzler 017 — Above the clouds
- EBM Gone Wild – Acute mountain sickness is more than one syndrome
- EBM Gone Wild – Predicting altitude sickness?
- EBM Gone Wild – A novel prevention for acute mountain sickness
- EBM Gone Wild – Deep breathing to prevent acute mountain sickness
Journal articles
- Imray C, et al (2010) Acute Mountain Sickness: Pathophysiology, Prevention and Treatment. Progress in Cardiovascular Diseases, 52, 467-484. PMID: 20417340
- Luks AM, et al. Wilderness Medical Society Consensus Guidelines for the Prevention and Treatment of Acute Altitude Illness. Wilderness Environ Med. 2010 Jun;21(2):146-155. Epub 2010 Mar 10. PMID: 20591379. [fulltext]
- Maggiorini M (2010) Prevention and Treatment of High-Altitude Pulmonary Edema. Progress in Cardiovascular Diseases, 52, 500-506 PMID: 20417343
- Palmer BF (2010) Physiology and Pathophysiology with Ascent to Altitude. The American Journal of the Medical Sciences [Epub ahead of print] PMID: 20442684
- Scherrer U, et al (2010) New Insights into the Pathogenesis of High-Altitude Pulmonary Edema. Progress in Cardiovascular Diseases, 52, 485-492. PMID:20417341

Critical Care
Compendium
Chris is an Intensivist and ECMO specialist at The Alfred ICU, where he is Deputy Director (Education). He is a Clinical Adjunct Associate Professor at Monash University, the Lead for the Clinician Educator Incubator programme, and a CICM First Part Examiner.
He is an internationally recognised Clinician Educator with a passion for helping clinicians learn and for improving the clinical performance of individuals and collectives. He was one of the founders of the FOAM movement (Free Open-Access Medical education) has been recognised for his contributions to education with awards from ANZICS, ANZAHPE, and ACEM.
His one great achievement is being the father of three amazing children.
On Bluesky, he is @precordialthump.bsky.social and on the site that Elon has screwed up, he is @precordialthump.
| INTENSIVE | RAGE | Resuscitology | SMACC