HIV and AIDS
OVERVIEW
- HIV = retrovirus infection -> infection of T-helper lymphocytes (CD4+) and progressively destroys them -> immunosuppression
- 40 million patients in the world
- 2 types: HIV 1 and HIV 2 (West Africa)
- modes of transmission: sexual intercourse, mother to child (pregnancy, labour and breast feeding), contaminated blood and needles
- AIDS = HIV with an AIDS defining illness
- can be thought of as a multi-system disorder
- respiratory failure is the commonest reason for admission to ICU
- with the new era of HAART (highly active antiretroviral therapy) -> ICU admissions for PCP are declining
- common procedures requiring anaesthesia = lymph node biopsy, splenectomy, partial colectomy, CVL’s, gastrostomy tubes and diagnostic procedures.
CLINICAL FEATURES
Risk Factors
- promiscuity
- other STI’s
- IVDU
- hemophiliacs
- Haitian and central/west African people
CDC Classification of HIV
- I – acute seroconversion illness
- II – asymptomatic infection
- III – persistent generalised lymphadenopathy
- IV – symptomatic HIV infection
Manifestations by system:
- RESP – PCP, aspergillosis, herpetic infections, candidiasis, CMV, Tb, normal bacterial pneumonia’s, nocardia, lymphoma, Kaposi sarcoma
- CVS – endocarditis, CCF, brainstem involvement -> arrhythmias, myocarditis -> DCM from cryptococcus, coxsackievirus B, CMV, aspergillus
- GI – diarrhoea, vomiting, LOA, dysphagia -> fluid assess and check electrolytes
- CNS – toxoplasmosis, cryptococcus, candida, mycobacterium, treponema, aspergillus, encephalitis, aseptic meningitis, HSV, multifocal leukoencephalopathy, lymphoma, polyneuropathy, HIV dementia
- HAEM – anaemia, thrombocytopaenia, leucopenia
- ENDO – CMV adrenalitis, exogenous corticosteroid administration -> adrenal suppression
- OBSTETRICS – with no intervention there is a transmission rate of 30% during pregnancy and 20% through breast milk -> with antiretroviral and C/S the transmission rate can be decreased to 2%
- PAIN – numerous aetiologies, HSV, arthralgia, peripheral neuropathy, drug-related pain
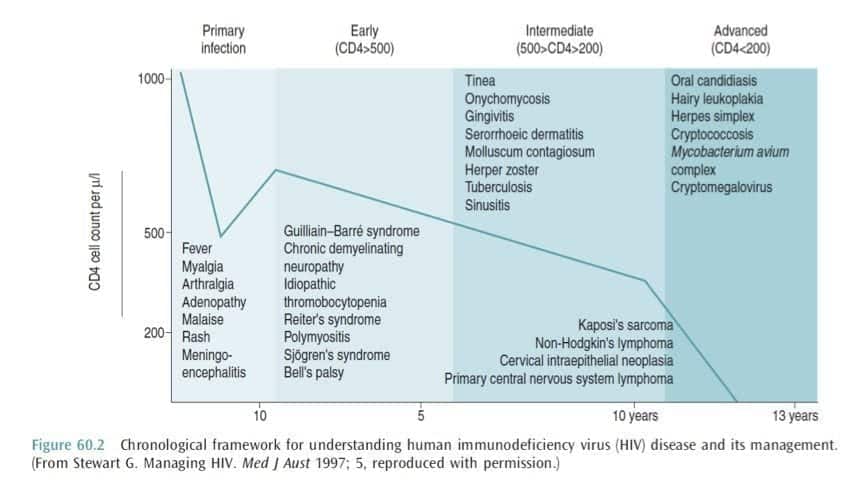
PROGRESSION OF ILLNESS
INVESTIGATIONS
- HIV RNA Reverse Transcription and amplification by PCR (primary HIV infection diagnosis)
- CD4 count
- anti-HIV IgG antibodies
- enzyme linked immunosorbent assay
- as indicated on clinical grounds
MANAGEMENT
Outpatient Management
- in the last 10 years our perceptions of HIV and AIDS has changed from fatal disease -> manageable chronic illness with the introduction of HAART (highly active antiretroviral therapy)
Antiretrovirals
- usually use 3 agents
1. nucleoside reverse transcriptase inhibitors (NRTI’s – zidovudine)
2. nucleotide reverse transcriptase inhibitors (RTI’s – tenofovir)
2. non-nucleoside reverse transcriptase inhibitors (NNRTI’s – nevirapine)
3. protease inhibitors (PI’s – saquinavir)
4. others: enfuvirtide
- aims = achieve an undetectable viral load -> improve duration and QOL
ICU Management
- HIV patients can present to ICU because of many reasons
- mortality rates from ICU admission is dramatically improving
Immune Reconstitution Syndromes
- HAART inhibits viral replication
-> increase in population of memory and naïve T cells
-> enhancement of lymphoproliferative responses
-> increased IL-2
-> reduction of some plasma proteins
- immune reconstitution syndrome = SIRS like illness with no organism found (granuloma in lung or fever, lymphadenopathy) that develops 2-8 weeks after starting HAART
- treatment: stop HAART -> reintroduction +/- steroids
Toxic effects of HAART
- PI’s -> pancreatitis, insulin resistance, hyperlipidaemia
- NRTI’s -> lactic acidosis by disruption of mitochondrial DNA replication
- abacavir -> hypersensitivity and subsequent anaphylaxis if re-challenged
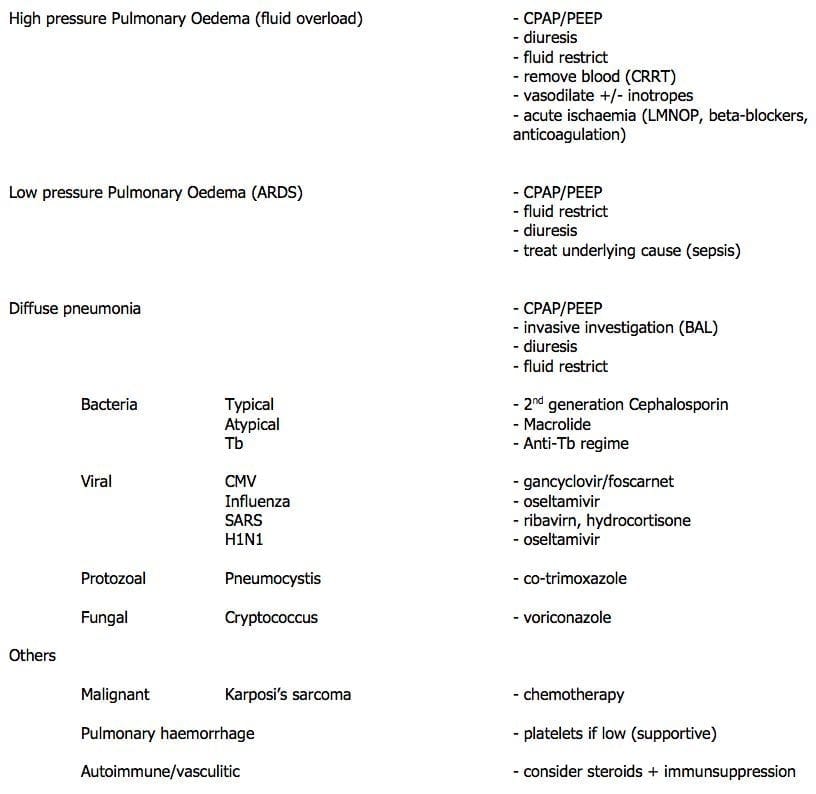
Respiratory Failure
- can be caused by anything!
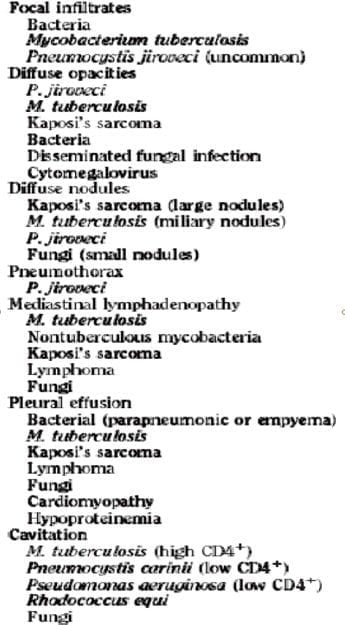
Diffuse Pulmonary Infiltrates:
Pneumocystis jiroveci (PCP):
- normally pneumocystis carinii (protozoa)
- now is classified as a fungus that only infects humans
- PCP with respiratory failure is a common reason with high mortality, however latest data shows that this decreasing with HAART
- CXR: ALI, pneumatoceles -> pneumothorax
- diagnosis: sputum PCR induced by inhalation of hypertonic saline or BAL
- treatment:
-> trimethoprim-sulfamethoxazole or pentamidine
-> steroids are typically given to attenuate lung injury caused by inflammatory response to killed organisms - prognosis: with HAART long term survival is considerably longer
Hepatitis C
- + HIV is associated with higher mortality
- with the introduction of HAART the prevalence of HCV associated cirrhosis increased by 4
- cellular immunity from HIV infections leads to accelerated HCV reproduction
- HCV also accelerates the progression of HIV disease
- consult widely if dealing with these disorders!
Central Nervous System Pathology
Meningitis/Encephalitis
- cryptococcal meningitis -> amphotericin B then PO fluconazole
- toxoplasma encephalitis -> sulfadiazine or clindamycin or pyrimethamine
Lesions that cause mass effect
- toxoplasmosis
- primary CNS lymphoma
- tuberculoma
- brain abscess (strep, staph, salmonella, aspergillus, norcardia, cryptococcus, listeria)
Perioperative Management
PREVENTION OF TRANSMISSION
- prevention of needle stick injuries (0.3% risk of transmission)
- prevention of mucocutaneous transmission (0.03% risk)
- vigilance
- universal precautions
- gloves
- HME’s
- appropriate decontamination
MANAGEMENT OF INJURY
- first aid
- post-exposure prophylaxis within 2 hours
- documentation (AIMS and Events Form)
- ID and occupational health follow up
AIDS defining illnesses that present to ICU
- pneumocystis jiroveci pneumonitis
- oesophageal candidiasis
- cryptococcal meningitis
- toxoplasma encephalitis
- CMV disease (retinal, oesophagus, bile ducts or colon)
- cryptosporidiosis
- mycobacterium avium complex
- Kaposi sarcoma (angioproliferative tumour)
- Lymphoma
- Cervical and anal neoplasms
- HIV related neurological disease (encephalopathy, myelopathy, peripheral neuropathy)
References and Links
LITFL
- CCC — Pneumocystis pneumonia (PJP or PCP)
- Clinical Cases – Humongous HIV Extravaganza
Journal articles
- Akgün KM, Huang L, Morris A, Justice AC, Pisani M, Crothers K. Critical illness in HIV-infected patients in the era of combination antiretroviral therapy. Proc Am Thorac Soc. 2011 Jun;8(3):301-7. doi: 10.1513/pats.201009-060WR. Review. PubMed PMID: 21653532; PubMed Central PMCID: PMC3132789.
- Akgün KM, Miller RF. Critical Care in Human Immunodeficiency Virus-Infected Patients. Seminars in respiratory and critical care medicine. 37(2):303-17. 2016. [pubmed]
- Huang L, Quartin A, Jones D, Havlir DV. Intensive care of patients with HIV infection. N Engl J Med. 2006 Jul 13;355(2):173-81. Review. PubMed PMID: 16837681. [Free Fulltext]
- Sarkar P, Rasheed HF. Clinical review: Respiratory failure in HIV-infected patients–a changing picture. Critical care (London, England). 17(3):228. 2013. [pubmed]

Critical Care
Compendium
Chris is an Intensivist and ECMO specialist at The Alfred ICU, where he is Deputy Director (Education). He is a Clinical Adjunct Associate Professor at Monash University, the Lead for the Clinician Educator Incubator programme, and a CICM First Part Examiner.
He is an internationally recognised Clinician Educator with a passion for helping clinicians learn and for improving the clinical performance of individuals and collectives. He was one of the founders of the FOAM movement (Free Open-Access Medical education) has been recognised for his contributions to education with awards from ANZICS, ANZAHPE, and ACEM.
His one great achievement is being the father of three amazing children.
On Bluesky, he is @precordialthump.bsky.social and on the site that Elon has screwed up, he is @precordialthump.
| INTENSIVE | RAGE | Resuscitology | SMACC