Intra-aortic Balloon Pump Trouble-shooting
aka Cardiovascular Curveball 007
Your ICU patient with the intra-aortic balloon pump (IABP) from Cardiovascular Curveball 005 is having a very bad night. His IABP keeps playing up. You are beginning to wonder if there a gremlin in the unit…
Can you fix the problems?
Warm up questions
Label the IABP waveform…which Arrow goes where?
Answer and interpretation
Which Arrow goes where?
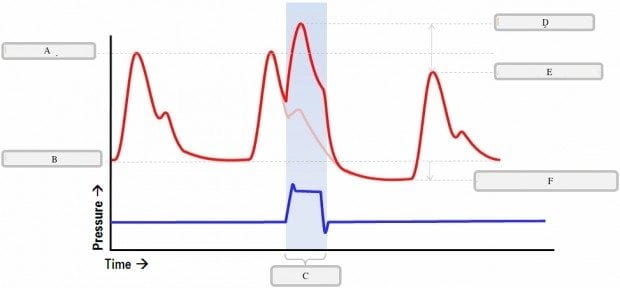
- Unassisted Peak Systolic Pressure?
- Diastolic Augmentation / Augmented Peak Diastolic Pressure?
- Balloon Aortic/ Assisted End Diastole Pressure?
- Assisted Peak Systolic Pressure?
- Unassisted End Diastolic Pressure?
- Balloon inflation?
Answers
A. Unassisted Peak Systolic Pressure
B. Unassisted End Diastolic Pressure
D. Diastolic Augmentation / Augmented Peak Diastolic Pressure
E. Assisted Peak Systolic Pressure
F. Balloon Aortic/ Assisted End Diastole Pressure
Which features indicate optimal timing and function of the IABP?
Answer and interpretation
Optimal timing and function of IABP has the following features:
- inflation of the balloon occurs at the dicrotic notch (forming the sharp ‘V’)
- the slope of rise of augmented diastolic waveform is straight and parallel to the systolic upstroke
- the augmented peak DBP at balloon deflation exceeds or is equal to end-systolic BP
- the balloon aortic end-diastolic BP (DBP at balloon deflation) is lower than the preceding unassisted end-DBP by 15-20 mmHg
- the assisted SBP (following a cycle of balloon inflation) is lower than the previous unassisted SBP by 5 mmHg
The timing of IABP inflation and deflation should be manually adjusted to achieve these optimal waveform characteristics if they are absent.
Scenarios
Too easy? Well, see if you can deal with these scenarios showing a segment of the aortic pressure waveform from your patient with an IABP and a 2:1 assist ratio:
Scenario 1
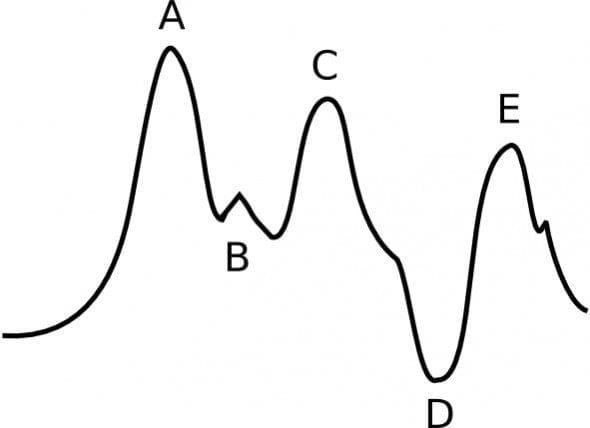
Q 1.1 What is the cause?
Answer and interpretation
Inflation of the IAB is occurring too late – it occurred well after the dicrotic notch (B).
Q 1.2 Describe the waveform and the abnormalities.
Answer and interpretation
Waveform features:
- Inflation of the IAB occurs after the dicrotic notch (B)
- Absence of a sharp V at the point of IAB inflation (should occur at B – the dicrotic notch)
- The augmented DBP (peak C) is less than the unassisted SBP (peak A) – it should be higher
Q 1.3 What are the physiological effects?
Answer and interpretation
Suboptimal augmentation of DBP (peak C) means that coronary perfusion may be inadequate.
Q 1.4 How can you correct this?
Answer and interpretation
Adjust the timing so that the IABP inflates at the dicrotic notch.
Scenario 2
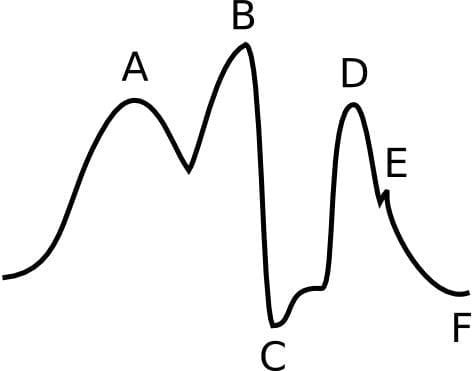
Q 2.1 What is the cause of the waveform abnormalities?
Answer and interpretation
Deflation of the IAB is too early – it occurred well before the onset left ventricular contraction and the start of systole.
Q 2.2 Describe the waveform and the abnormalities.
Answer and interpretation
Waveform features:
- There is a sharp drop in pressure immediately following the peak of diastolic augmentation (peak B).
- Diastolic augmentation may be suboptimal but it is difficult to confirm in the absence of a pressure scale or comparison to an unassisted waveform.
- Assisted aortic end-diastolic BP may be sub-optimally increased (trough C), but it is difficult to say based on the information given. With early deflation a widened U-shaped trough is typically seen. Early deflation can lead to an assisted aortic end-diastolic BP that equals or exceeds the unassisted aortic end-diastolic BP (trough F), although this is not the case in this scenario.
- Assisted SBP (peak D) is the same or higher than the unassisted SBP (peak A) – it should be slightly less.
Q 2.3 What are the physiological effects?
Answer and interpretation
Early IAB deflation may result in:
- inadequate coronary perfusion, with the potential for retrograde coronary blood flow. This may result in angina due to decreased myocardial oxygen supply.
- suboptimal afterload reduction and increased myocardial oxygen demand
Q 2.4 How can you correct this?
Answer and interpretation
Prolong the IAB inflation time, so that it deflates at the end of diastole, just before the onset of isovolumetric systolic contraction.
Scenario 3
Q 3.1 What is the cause of the waveform abnormalities?
Answer and interpretation
Inflation of the IAB is occurring too early – it occurred prior to aortic valve closure (indicated by the absence of a dicrotic notch).
Q 3.2 Describe the waveform and the abnormalities
Answer and interpretation
Waveform features:
- Diastolic augmentation (peak B) encroaches on the peak corresponding to unassisted systole (peak A) – the two peaks have merged and are barely distinguishable.
- There is no ‘sharp V’ or dicrotic notch between peaks A and B.
Q 3.3 What are the physiological effects?
Answer and interpretation
Early IAB inflation may result in:
- Premature closure of the aortic valve and possible aortic regurgitation, thus impairing left ventricular emptying. There may be an increase in LVEDV, LVEDP and PCWP.
- Increased left ventricular wall stress (afterload) and increased myocardial oxygen consumption will occur.
Q 3.4 How can you correct this?
Answer and interpretation
Delay the onset of IAB inflation, so that it inflates at the dicrotic notch resulting in a ‘sharp V’ (see the normal pressure waveform).
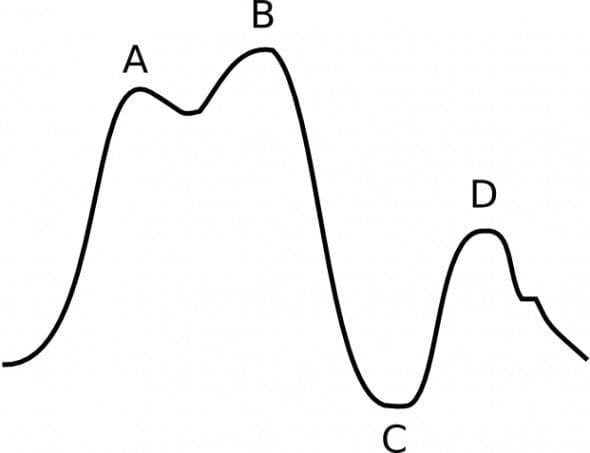
Scenario 4

Q 4.1 What is the cause of the waveform abnormalities?
Answer and interpretation
Deflation of the IAB is occurring too late – deflation is occurring as the aortic valve is opening.
Q 4.2 Describe the waveform and the abnormalities.
Answer and interpretation
Waveform features:
- The peak corresponding to diastolic augmentation (peak C) is widened.
- Assisted aortic end-diastolic BP (trough E) is the same as, not lower than, the unassisted aortic end-diastolic BP (trough G).
- The upstroke of assisted systolic BP (peak F) has a gentle gradient resulting in a prolonged rise.
Q 4.3 What are the physiological effects?
Answer and interpretation
Late deflation of the IAB has these effects:
- There is no afterload reduction. The inflated balloon may actually impede left ventricular ejection and increase the afterload.
- Myocardial oxygen consumption will increase because the left ventricle experiences a longer period of isovolumetric contraction (when most myocardial oxygen consumption occurs) and has to contract against greater resistance (afterload).
Q 4.4 How can you correct this?
Answer and interpretation
Shorten the IAB inflation time, so that the IAB deflates at the end of diastole – just before isovolumetric contraction of the left ventricle.
Scenario 5
After struggling all night optimizing the timing of the balloon pump, the patient develops atrial fibrillation with intermittent ventricular ectopy.
Q 5.1 What problems will this cause for the intra-aortic balloon pump?
Answer and interpretation
- Triggering of the IABP is usually set according to the patient’s ECG tracing.
- When an R wave is detected the balloon is triggered to automatically start inflating in the middle of the T wave.
- Triggering can be impaired if the patient develops an arrhythmia, is paced or has a poor ECG trace.
Q 5.2 What can be done about it?
Answer and interpretation
- If the IABP cannot be successfully triggered using the R waves from the ECG trace, pacing spikes or the arterial blood pressure waveform may used for triggering.
- Alternatively, the pump can be set at an intrinsic rate without any physiological triggering.
- The IABP may automatically use these other modes as default backups if ECG-triggered timing is not possible.
- If the patient remains haemodynamically stable despite the IABP malfunctioning it might be a good time to think about removing the IABP
- …treating any underlying causes of arrhythmia is also a good idea!
References
- Overwalder PJ. Intra Aortic Balloon Pump (IABP) Counterpulsation. The Internet Journal of Perfusionists. 2000;1:(1) (fulltext online) [Scenarios 1-4 are based on a figure from this article]
- Marino’s The Little ICU Book
- Krishna M, Zacharowski K. Principles of Intra-Aortic Balloon Pump Counterpulsation. Cont Edu Anaesth Crit Care & Pain. 2009;9(1):24-28. [Reference]
- Datascope’s IABP elearning modules
- Gomersall C. Intra-aortic balloon pumping. 1999.
- LITFL CCC — Intra-Aortic Balloon Pump
- The IABP waveforms in each of the scenarios were drawn using the open-source vector graphics editor Inkscape.
CLINICAL CASES
Cardiovascular Curveball
Chris is an Intensivist and ECMO specialist at The Alfred ICU, where he is Deputy Director (Education). He is a Clinical Adjunct Associate Professor at Monash University, the Lead for the Clinician Educator Incubator programme, and a CICM First Part Examiner.
He is an internationally recognised Clinician Educator with a passion for helping clinicians learn and for improving the clinical performance of individuals and collectives. He was one of the founders of the FOAM movement (Free Open-Access Medical education) has been recognised for his contributions to education with awards from ANZICS, ANZAHPE, and ACEM.
His one great achievement is being the father of three amazing children.
On Bluesky, he is @precordialthump.bsky.social and on the site that Elon has screwed up, he is @precordialthump.
| INTENSIVE | RAGE | Resuscitology | SMACC

I love reading your page. It’s very simple to understand and educative. It’s very helpful! Thank you very much.
Fantastic indeed
Best show i have ever seen about IABP education!
This was the most informative page and easy to grasp. Thank you so much for the breakdown of what’s happening with the way form, what it means, it’s impact on physiology, and what to do about it.