Intra-Aortic Balloon Pump Overview
OVERVIEW
Intra-Aortic Balloon Pump (IABP) or intra-aortic counterpulsation device
- the balloon is inflated during diastole to increase coronary perfusion and then deflated during systole to decrease afterload
- This aims to improve myocardial oxygenation, increase cardiac output and organ perfusion with a reduction in left ventricular workload
INDICATIONS
IABP is used as a supportive treatment tool in a clinical context that will improve (bridging therapy) due to recovery or treatment
- cardiogenic shock
- post bypass
- post MI
- cardiomyopathy
- severe IHD awaiting surgery or stenting
- severe acute MR awaiting surgery
- prophylactically in high risk patient pre-stenting/ cardiac surgery
- miscellaneous (i.e. post myocardial contusion which is expected to recover with time)
Intra-Aortic Balloon Pumps have also been inserted as a last-ditch measure to stop haemorrhage from the aorta or its branches (e.g. massive GI haemorrhage)
CONTRAINDICATIONS
- aortic regurgitation
- aortic dissection
- severe aortoiliac or peripheral vascular disease
- aneurysm or other anatomical disease of aorta
- prosthetic aortic tree grafts
- local sepsis
- lack of experience with management
- severe coagulopathy
- not effective in a setting of a CI of < 1.2 and tachyarrhythmias
DESCRIPTION
The IABP has two parts:
- a large bore catheter with a long sausage-shaped balloon at the distal tip, and
- a console containing a pump that inflates the balloon
Features
- balloon is made of a polyurethane membrane mounted on a vascular catheter
- various catheter sizes — usually 7.5 F with the balloon size chosen according to height (25–50 cc)
- may be sheathed or sheathless
- some newer catheters have fibre optics that assist pressure waveform detection and timing
- helium is used to inflate the balloon as its low density means there is little turbulent flow so the balloon can inflate fast and deflate slowly. It is also relatively benign and eliminated quickly if there is a leak or the balloon ruptures
- when inflated the balloon occludes 80-90% of the aorta
INSERTION
Preparation
- patient positioned supine
- sterile technique (gowns, gloves, mask, drapes, sterile prep solution)
- check for bleeding diathesis and other complications
Method
- fully collapse balloon applying vacuum with 60 ml syringe; some kits require that the plunger is completely pulled out to achieve this
- percutaneous Seldinger technique or surgical
- with or without sheath
- access femoral artery at 45 degrees with needle
- pass guidewire through needle and advance until tip is is in thoracic aorta. Wire should pass very easily
- pass sheath over wire in similar manner to insertion of PA catheter sheath (sheath is not always used)
- Pass balloon through sheath over guidewire and insert estimated distance – measure from sternal angle to umbilicus then to femoral artery. Must be inserted to at least the level of the manufacturer’s mark (usually double line) to ensure that entire balloon has emerged from sheath
- Balloon should be positioned so that the tip is about 1 cm distal to the origin of the left subclavian artery
- watch for loss of left radial pulse (too high)
- Remove wire — return of blood via central lumen confirms that the tip is not subintimal and has not caused a dissection
- Flush central lumen and connect to transducer to monitor intra-aortic pressure (the outer lumen transmits helium gas to the balloon)
Confirmation of position
- Arterial balloon waveform and pressures are shown on the console
- check for normal morphology and appropriate timing of inflation and deflation in 1:2 augmentation ratio
- Chest x-ray or fluoroscopy
- confirms radiopaque tip lies in the 2nd intercostal spaces just above the left main bronchus; the lower end of the balloon should lie cephalad to the renal arteries
- or transoesophageal echo (TOE)
- direct visualisation 1cm distal to the left subclavian artery
USE
Triggering and timing
- The balloon is timed to inflate and deflate in time with the cardiac cycle
- Trigger options include:
- ECG (using the R wave to identify the onset of systole); if sinus rhythm (SR) then deflation can be for a set time period, in atrial fibrillation (AF) the balloon deflates when R waves are sensed
- If paced then pacing spikes can be used to detect cardiac cycle events
- Arterial waveform (using the arterial upslope to designate systole)
- An internal trigger mode is available for asystolic arrested patients
Optimising performance
- correct position (balloon just distal to left subclavian artery, 2 cm above left main bronchus)
- optimal balloon volume
- balloon timing
- inflation at onset of diastole and deflation prior to the beginning of systole (check this in 1:2 augmentation ratio)
- regular rhythm
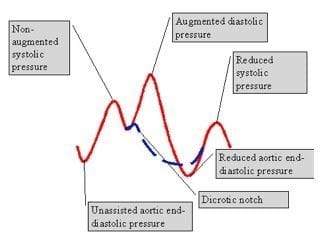
- timing: 1:1 – inflation takes place at the dicrotic notch
- slope of augmented diastolic wave form is straight and parallel to the systolic upstroke
- the augmented diastolic pressure should exceed non-augmented systolic pressure
- the end-diastolic pressure at balloon deflation is lower than preceding unassisted end-diastolic pressure by 15 mmHg
- the systolic pressure following a cycle of balloon inflation should be lower than the previous unassisted systolic pressure by about 5 mmHg
Efficiency is affected by
- the timing of inflation and deflation
- assist ratio
- heart rate (tachycardia > 130/min reduces the benefit of IABP)
- gas loss from the balloon
- CI of 1.2-1.4 required for IABP to be effective
COMPLICATIONS
During insertion
- failure to advance catheter beyond iliofemoral system because of atherosclerotic disease (common)
- aortic dissection and arterial perforation – may cause retroperitoneal haemorrhage
- malposition
- accidental femoral vein cannulation and damage to local structures
During use
- thrombosis at the insertion site causing limb ischemia
- peripheral embolisation and end-organ ischaemia (e.g. limb ischaemia with compartment syndrome, gut, kidneys and spine)
- incorrect positioning with vascular occlusion (e.g. SCA, renal arteries and other aortic branches)
- infection
- perforation
- balloon rupture (look for the presence of blood in the connecting tubing)
- gas embolisation
- haemolysis and thrombocytopenia
- peripheral neuropathy
- timing errors
During or after removal
- haemorrhage – particularly with the sheathed sets, consider surgical repair of insertion sites in sheathed balloons
- pseudoaneurysm
- AV fistula
- entrapment leading to inability to remove (maybe due to small perforation allowing blood to enter balloon, may require aortotomy)
OTHER INFORMATION
Catheter types
- balloon size based on height (25-50cc)
- sheathed or sheathless kits
- new fibreoptic catheters that improve arterial pressure waveform detection and timing
Anticoagulation
- controversial if routinely required during first the 24 hours
- low dose heparin infusion often prescribed; some units infuse heparinised saline through the transducer set
Causes of decreased augmentation
- balloon not needed any longer (myocardial recovery)
- balloon rupture
- distributive shock (sepsis)
Management of helium embolus
- immediate cessation of counterpulsation
- placement of the patient head down
- IAB removal
- Consider giving broad spectrum antibiotics as the gas chamber of the balloon is not sterile
Weaning
- should be considered when inotropic requirements are minimal
- achieved gradually (over 6–12 h) reducing the ratio of augmented to non-augmented beats from 1:1 to 1:2 or less (1:3 ratio is the same as no support) and/or decreasing the balloon volume
- balloon should never be turned off in situ except when the patient is anticoagulated because of the risk of thrombus formation on the balloon
Extracorporeal membrane oxygenation (ECMO)
- in centers that use VA ECMO the role of IABP is controversial
- IABP may offer some additional support to a patient on VA ECMO by assisting LV function or by providing more pulsatile flow to improve coronary perfusion
- there concerns that IABP will interfere with VA ECMO function due to its position in the aorta, and further contribute to the risk of lower limb ischaemia
EVIDENCE
IABP for myocardial infarction, cardiogenic shock and coronary revascularisation
- IABP-SHOCK II trial (2012) showed no 30-day mortality benefit from IABP insertion for cardiogenic shock following MI when early revascularisation was planned. See Cardiogenic Shock Literature Summaries for more details on this article. A subsequent paper showed that there was no mortality benefit at 12 months either.
- Ranucci et al (2013) found that in patients undergoing nonemergent coronary operations, with a stable hemodynamic profile and a left ventricular ejection fraction <35%, the pre-incision insertion of intra-aortic balloon pump does not result in a better outcome.
- Sjauw et al (2009) systematic review found that only low-quality observational studies support IABP use post-STEMI for thrombolysis, not for PCI. There was no support from randomised studies.
- TACTICS trial (2005) was a small trial that showed no mortality benefit for IABP in addition to thrombolysis for STEMI, but there was a trend to improved Killip class in patients with severe heart failure/ cardiogenic shock
- The Randomised IABP study group trial (1994) found that patients randomized to aortic counterpulsation following revascularisation for MI had significantly less reocclusion of the infarct-related artery during follow-up (median 5 days) compared with control patients (8% versus 21%, P < .03).
- Despite the paucity of evidence for cardiogenic shock complicating MI, up until 2012, use of IABP for mechanical assistance had a class IC recommendation in the current European Society of Cardiology guidelines and a class IB recommendation in the American College of Cardiology/American Heart Association Guidelines.
VIDEO
Introduction to the IABP by CritIQ:
Timing and triggering of the IABP by CritIQ:
References and Links
LITFL
- CCC — Cardiogenic Shock Literature Summaries
- Cardiovascular Curveball 005 — Intra-aortic balloon pump
- Cardiovascular Curveball 007 — Intra-aortic balloon pump troubleshooting
Journal articles and textbooks
- Kantrowitz A, Tjonneland S, Freed PS, Phillips SJ, Butner AN, Sherman JL Jr. Initial clinical experience with intraaortic balloon pumping in cardiogenic shock. JAMA. 1968 Jan 8;203(2):113-8. PMID: 5694059.
- Krishna B, Zacharowski K. Principles of intra-aortic balloon pump counterpulsation. Contin Educ Anaesth Crit Care Pain (2009) 9 (1): 24-28. doi: 10.1093/bjaceaccp/mkn051 [Free Fulltext]
- Ohman EM, et al; TACTICS Trial. Thrombolysis and counterpulsation to improve survival in myocardial infarction complicated by hypotension and suspected cardiogenic shock or heart failure: results of the TACTICS Trial. J Thromb Thrombolysis. 2005 Feb;19(1):33-9. PMID: 15976965.
- Ohman EM, et al. Use of aortic counterpulsation to improve sustained coronary artery patency during acute myocardial infarction. Results of a randomized trial. The Randomized IABP Study Group. Circulation. 1994 Aug;90(2):792-9. PMID: 8044950
- Parissis H. Haemodynamic effects of the use of the intraaortic balloon pump. Hellenic J Cardiol. 2007 Nov-Dec;48(6):346-51. PMID: 18196657.
- Ranucci M, Castelvecchio S, Biondi A, de Vincentiis C, Ballotta A, Varrica A, Frigiola A, Menicanti L; Surgical and Clinical Outcome Research (SCORE) Group. A randomized controlled trial of preoperative intra-aortic balloon pump in coronary patients with poor left ventricular function undergoing coronary artery bypass surgery*. Crit Care Med. 2013 Nov;41(11):2476-83. PMID: 23921278.
- Sjauw KD, Engström AE, Vis MM, van der Schaaf RJ, Baan J Jr, Koch KT, de Winter RJ, Piek JJ, Tijssen JG, Henriques JP. A systematic review and meta-analysis of intra-aortic balloon pump therapy in ST-elevation myocardial infarction: should we change the guidelines? Eur Heart J. 2009 Feb;30(4):459-68. PMID: 19168529.
- Thiele H, et al; IABP-SHOCK II Trial Investigators. Intraaortic balloon support for myocardial infarction with cardiogenic shock. N Engl J Med. 2012 Oct 4;367(14):1287-96. PMID: 22920912.
- Thiele H, et al; Intraaortic Balloon Pump in cardiogenic shock II (IABP-SHOCK II) trial investigators. Intra-aortic balloon counterpulsation in acute myocardial infarction complicated by cardiogenic shock (IABP-SHOCK II): final 12 month results of a randomised, open-label trial. Lancet. 2013 Nov 16;382(9905):1638-45. PMID: 24011548.
- Unverzagt S, et al. Intra-aortic balloon pump counterpulsation (IABP) for myocardial infarction complicated by cardiogenic shock. Cochrane Database Syst Rev. 2011 Jul 6;(7):CD007398. PMID: 21735410.
FOAM and web resources
- Arrow — Intra-Aortic balloon Pump: Trouble-shooting Beyond the Basics (pdf)
- ATOTW — Intra-Aortic Balloon Counterpulsation (pdf)
- ICN — SMACC: Litton – Prevention over Cure: Can High Risk Cardiac Surgery Save the Balloon Pump? (2013)
- ICUFAQs — Intra-Aortic Balloon Pump Review (word doc)
- Radiopaedia — IABP (entry search)
- Resus.ME — Double balloon pump fail (2013)
- UMEM Pearls — To pump or not to pump

Critical Care
Compendium
Chris is an Intensivist and ECMO specialist at The Alfred ICU, where he is Deputy Director (Education). He is a Clinical Adjunct Associate Professor at Monash University, the Lead for the Clinician Educator Incubator programme, and a CICM First Part Examiner.
He is an internationally recognised Clinician Educator with a passion for helping clinicians learn and for improving the clinical performance of individuals and collectives. He was one of the founders of the FOAM movement (Free Open-Access Medical education) has been recognised for his contributions to education with awards from ANZICS, ANZAHPE, and ACEM.
His one great achievement is being the father of three amazing children.
On Bluesky, he is @precordialthump.bsky.social and on the site that Elon has screwed up, he is @precordialthump.
| INTENSIVE | RAGE | Resuscitology | SMACC

Just a potential correction in case any part 1 nerds are reading…
You mentioned that helium is used as it causes less turbulence in the IABP due to low viscosity. I think you meant to say that helium has low density, therefore less risk of turbulence as per Reynolds eqn Re = 2rvd / n.
Thanks for a very helpful and informative summary!
Thanks Dan – I think you’re right – have fixed!
Cheers
Chris