Medically cleared?
aka Neurological Mind-boggler 011
A 27 year-old previously well female, presented with a two week history of increasingly bizarre behavior. Her family reported that she had become more withdrawn over this time, stopped attending work and described her as walking around “talking to voices”. On the day of admission she walked into her parents room and urinated on the floor. Prior to this she had no psychiatric or medical history, and was performing well in her job as a lawyer. Her family reports that prior alcohol use as ‘minimal’ and no history of recreational drug use.
She was admitted to the psychiatric unit for presumed acute psychosis after normal initial investigations including a CT brain.
Within one week she deteriorated to a near catatonic state, and began to have periods of akinesis alternating with agitation. Seven days after admission she began to develop orofacial dyskinesia, and at day 10 had a single general tonic-clonic seizure.
The patient was reviewed by the neurology team. An EEG, Lumbar Puncture, MRI-Brain and Pelvic USS were ordered with the following results:
CSF: Lymphocytic pleocytosis
MRI-Brain: Normal
EEG: Generalised slowing, no epileptic features
Pelvic USS: 6cm right-sided ovarian cyst with complex features
Questions
Q1. What is the likely diagnosis and what are the important differentials?
Answer and interpretation
Anti-NMDA Receptor Encephalitis is the most likely diagnosis (see Q2).
Important differentials include:
- Infectious encephalidites (particularly HSV and HHV-6)
- Other autoimmune etiologies (e.g. limbic encephalitis due to autoantibodies against Hu, Ma2, CV2 and amphiphysin)
- Neuroleptic malignant syndrome
- Lethal catatonia
- Cerebral space-occupying lesions
- Metabolic disorders – hyper/hypothyroidism, Cushings syndrome, Addison’s disease
- Psychiatric disorders – schizophrenia, psychotic depression, pseudo-seizures
- Drugs, toxins or withdrawal (unlikely given the history)
Q2. How is the diagnosis confirmed?
Answer and interpretation
Definitive diagnosis is achieved with positive NR1 and NR2 antibodies in CSF combined with a characteristic clinical picture (the antibodies have 100% sensitivity and specificity according to Wandinger et al 2011).
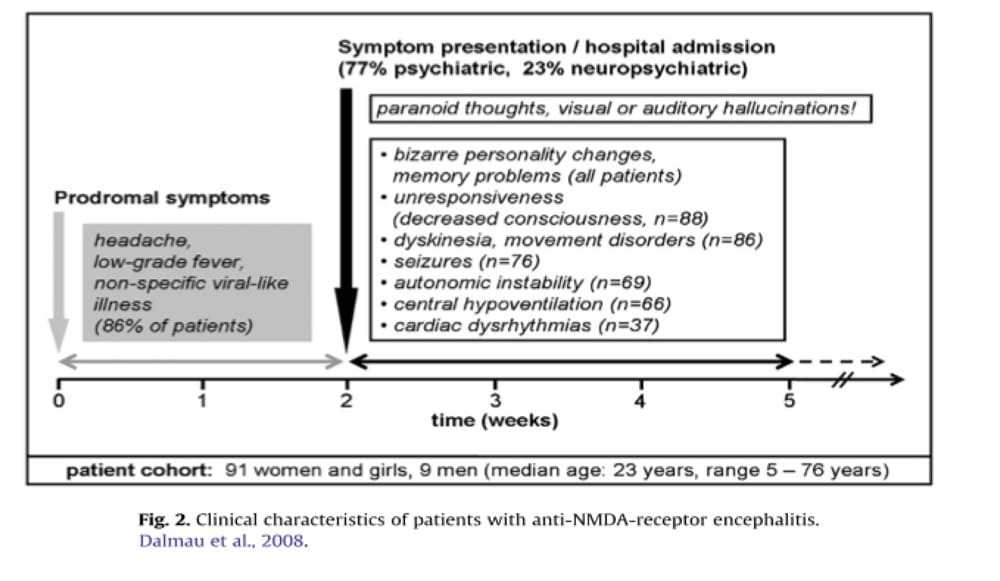
Relatively little is know about this disease, which was first described in 2007, with a subsequent case series published in 2008 in Lancet Neurology. Wandinger et al (2011) describe a typical clinical course:
“A non-specific flu-like prodrome (sub-febrile temperature, headache, fatigue) is always followed by a psychotic stage with bizarre behaviour, disorientation, confusion, paranoid thoughts, visual or auditory hallucinations and memory deficits. Because of these features a large proportion of patients end up in psychiatric therapy, and in many cases a drug-induced psychosis is initially diagnosed. In the following phase, decreased consciousness, hypoventilation, lethargy, seizures, autonomous instability and dyskinesias develop.”
Q3. Why was a pelvic USS ordered?
Answer and interpretation
To look for a pelvic tumour.
60% of patients with anti-NMDA receptor encephalitis have the presence of a tumour (most commonly teratoma). Early identification and removal of tumour is associated with better outcomes.
Q4. What is the likely pathogenesis of this condition?
Answer and interpretation
Antibodies against NR1-NR2 NMDA receptors are central to the pathogenesis of this condition.
These antibodies cause a reversible reduction in post-synaptic NMDA receptor clusters without complement activation. These receptors, which are highly expressed in the forebrain, limbic system, and hypothalamus, are made up of two sub-units: the NR1 subunit, which binds glycine, and the NR2 sub-unit, which binds glutamate.
Owing to the fact that patients frequently improve with immunotherapeutic treatment and tumour removal, an immune mediated mechanism is highly likely.
Q5. How is it treated?
Answer and interpretation
Current evidence suggests early removal of tumour (if present) and immunotherapy are the mainstays of treatment.
Immunotherapy includes consideration of corticosteroids, intravenous immunoglobulin and plasma exchange therapy in severe cases.
Q6. What is the prognosis of this condition?
Answer and interpretation
Of the 100 cases in the article by Dalmau et al, the following outcomes were observed over a mean follow up period of 17 months:
- 47% Full Recovery
- 28% Mild stable deficits
- 18% Severe deficits
- 7% Death
There was a trend for better outcomes in patients who had tumour identified and removed within 4 months of symptom onset.
References
- Hayes J. Anti-NMDA Receptor Encephalitis. LITFL
- Punja M, Pomerleau AC, Devlin JJ, Morgan BW, Schier JG, Schwartz MD. Anti-N-methyl-D-aspartate receptor (anti-NMDAR) encephalitis: an etiology worth considering in the differential diagnosis of delirium. Clin Toxicol (Phila). 2013 Sep-Oct;51(8):794-7.
- Dalmau J, Tüzün E, Wu HY, Masjuan J, Rossi JE, Voloschin A, Baehring JM, Shimazaki H, Koide R, King D, Mason W, Sansing LH, Dichter MA, Rosenfeld MR, Lynch DR. Paraneoplastic anti-N-methyl-D-aspartate receptor encephalitis associated with ovarian teratoma. Ann Neurol. 2007 Jan;61(1):25-36.
- Dalmau J, Gleichman AJ, Hughes EG, Rossi JE, Peng X, Lai M, Dessain SK, Rosenfeld MR, Balice-Gordon R, Lynch DR. Anti-NMDA-receptor encephalitis: case series and analysis of the effects of antibodies. Lancet Neurol. 2008 Dec;7(12):1091-8.
- Graus F, Saiz A, Dalmau J. Antibodies and neuronal autoimmune disorders of the CNS. J Neurol. 2010 Apr;257(4):509-17
- Wandinger KP, Saschenbrecker S, Stoecker W, Dalmau J. Anti-NMDA-receptor encephalitis: a severe, multistage, treatable disorder presenting with psychosis. J Neuroimmunol. 2011 Feb;231(1-2):86-91
- Young PJ, Baker S, Cavazzoni E, Erickson SJ, Krishnan A, Kruger PS, Rashid AH, Wibrow BA. A case series of critically ill patients with anti- N-methyl-D-aspartate receptor encephalitis. Crit Care Resusc. 2013 Mar;15(1):8-14.
- Rege S. Anti-N-methyl-D-aspartate (Anti-NMDA) Receptor Encephalitis – A Synopsis. Psyche Scene Hub 2018.
Neurological Mind-boggler
Chris is an Intensivist and ECMO specialist at The Alfred ICU, where he is Deputy Director (Education). He is a Clinical Adjunct Associate Professor at Monash University, the Lead for the Clinician Educator Incubator programme, and a CICM First Part Examiner.
He is an internationally recognised Clinician Educator with a passion for helping clinicians learn and for improving the clinical performance of individuals and collectives. He was one of the founders of the FOAM movement (Free Open-Access Medical education) has been recognised for his contributions to education with awards from ANZICS, ANZAHPE, and ACEM.
His one great achievement is being the father of three amazing children.
On Bluesky, he is @precordialthump.bsky.social and on the site that Elon has screwed up, he is @precordialthump.
| INTENSIVE | RAGE | Resuscitology | SMACC
