Necrotising fasciitis
Reviewed and revised 12 July 2015
OVERVIEW
- Necrotising fasciitis is a severe bacterial soft tissue infection marked by edema and necrosis of subcutaneous tissues with involvement of adjacent fascia and by painful red swollen skin over affected areas
- may resemble cellulitis initially but is often rapidly progressive
- commonly known as ‘flesh-eating disease’
- Fournier gangrene is a polymicrobial necrotizing fasciitis of the perineal, perianal, or genital areas
CLASSIFICATION
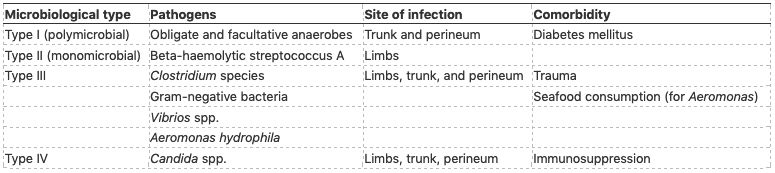
From Misiakos et al, 2014:
Classification of responsible pathogens according to type of infection.
Fournier gangrene is typically polymicrobial infection with aerobes and anaerobes, such as coliforms, klebsiella, streptococci, staphylococci, clostridia, bacteroids, and corynbacteria
CAUSTIVE ORGANISMS
Monomicrobial pathogens:
- Streptococci (especially Streptococcus pyogenes – Group A)
- Clostridium perfringens (gas gangrene) and other Clostridial species
- Staph aureus
- Vibrio vulnificans
- Aeronomonas hydrophila
Polymicrobial pathogens
- mixed aerobe-anaerobe bacterial flora (E.coli, Bacteroides fragillis, Strep and Staph)
RISK FACTORS
- DM
- ETOH abuse
- PVD
- renal failure
- odontogenic infection
- malignancy
- chicken pox
- local penetrating trauma or animal bite
- recent surgery (e.g. abdominal or peritoneal surgery)
- HOWEVER, Group A Strep -> has particularly affinity for young healthy patients ? no previous exposure makes it highly virulent
CLINICAL ASSESSMENT
History
- spreading erythema
- sepsis (fever, chills, myalgia)
- severe constant pain that is out of proportion to clinical findings
- cutaneous anaesthesia
- evidence of developing organ failures
- underlying risk factors (See above)
- commonly an extremity -> but can affect anywhere (e.g. perineum = Fournier gangrene)
Examination
- Local:
- erythematous, tender, swollen
- skin becomes smooth, shiny and tensely swollen -> darkens, patchy, blisters and bullae -> gangrene
- a wooden-hard feel of the subcutaneous tissue
- oedema beyond the margin of erythema
- crepitus (gas gangrene)
- Systemic
- fever, tachycardia
- haemodynamic instability
- rapid spread on re-examination
INVESTIGATIONS
Investigations should not be performed if they delay definite surgical intervention in a suspected case of necrotizing fasciitis
Laboratory
- blood cultures
- FMC (leucocytosis/leukopaenia)
- elevated CRP
- Coagulation profile (DIC)
- UEC (renal failure)
- elevated CK
Imaging
- XR: gas in subcutaneous tissues
- CT: subcutaneous air
- MRI: extent of fascial necrosis seen and can guide limits of debridement
Other
- biopsy: can help differentiate between fasciitis and cellulitis
- surgery reveals the absence of normally adherent fascia to blunt dissection + watery, thin foul smelling pus in subcutaneous space
MANAGEMENT
Resuscitation
- aggressive management of septic shock if present
Specific therapy
- Extensive urgent surgical debridement (the mainstay!)
- Antimicrobial therapy
- clindamycin and lincomycin -> theoretically suppress toxin production by streptococci (no clinical evidence)
- penicillin is often added but is not necessary for empiric treatment
- nosocomial infections -> vancomycin to cover MRSA (plus clindamycin or lincamycin)
Empiric
- Meropenem 1g or 25mg/kg Q8 hrly + Clindamycin 600mg or 15mg/kg Q8h
Streptococcus pyogenes
- Penicillin 1.8g or 45mg/kg Q4 hrly or Cephazolin 2g or 50mg/kg Q6 hrly + Clindamycin 600mg or 15mg/kg Q8 hrly
Clostridial infection
- Benzylpenicillin 2.4g or 60mg/kg Q4 hourly or Metronidazole 500mg or 12.5mg/kg Q8 hrly
Polymicrobial (e.g. Fournier gangrene)
- Meropenem 1g or 25mg/kg Q8 hrly
- Other therapies
- can use lincomycin 600mg or 15mg/kg IV Q8hrly instead of clindamycin
- hyperbaric oxygen – maybe beneficial in anaerobic gram –ve necrotising fasciitis (Concrane: “no evidence to support or refute“)
- intravenous immunoglobulin (IVIG) 0.4 to 2 g/kg IV, for 1 or 2 doses during the first 72 hours – consider in Group A Strep necrotising fasciitis based on expert advice
Seek and treat underlying cause and complications (e.g. diabetes mellitus)
Supportive care and monitoring
Consults
- General surgeon
- ENT (if needs grommets for hyperbaric chamber)
- Infectious diseases
Disposition
- urgent transfer to operating theatre
- often need ICU admission post-operatively, may need further surgeries and often treated with hyperbaric oxyen
PROGNOSIS
- mortality 30-40% with appropriate therapy
- increased mortality in co-morbid patients
- mortality directly proportional to delay in diagnosis and treatment
References and Links
LITFL
- Eponymictionary – Fournier gangrene
- Eponymictionary – Alfred Jean Fournier (1832-1914)
Journal articles
- Levett D, Bennett MH, Millar I. Adjunctive hyperbaric oxygen for necrotizing fasciitis. Cochrane Database Syst Rev. 2015;1:CD007937. [pubmed]
- Misiakos EP, Bagias G, Patapis P, Sotiropoulos D, Kanavidis P, Machairas A. Current concepts in the management of necrotizing fasciitis. Front Surg. 2014;1:36. [pubmed]
- Puvanendran R, Huey JC, Pasupathy S. Necrotizing fasciitis. Can Fam Physician. 2009;55:(10)981-7. [pubmed]
- Thwaini A, Khan A, Malik A, et al. Fournier’s gangrene and its emergency management. Postgrad Med J. 2006;82:(970)516-9. [pubmed] [Free Full Text]

Critical Care
Compendium
Chris is an Intensivist and ECMO specialist at the Alfred ICU in Melbourne. He is also a Clinical Adjunct Associate Professor at Monash University. He is a co-founder of the Australia and New Zealand Clinician Educator Network (ANZCEN) and is the Lead for the ANZCEN Clinician Educator Incubator programme. He is on the Board of Directors for the Intensive Care Foundation and is a First Part Examiner for the College of Intensive Care Medicine. He is an internationally recognised Clinician Educator with a passion for helping clinicians learn and for improving the clinical performance of individuals and collectives.
After finishing his medical degree at the University of Auckland, he continued post-graduate training in New Zealand as well as Australia’s Northern Territory, Perth and Melbourne. He has completed fellowship training in both intensive care medicine and emergency medicine, as well as post-graduate training in biochemistry, clinical toxicology, clinical epidemiology, and health professional education.
He is actively involved in in using translational simulation to improve patient care and the design of processes and systems at Alfred Health. He coordinates the Alfred ICU’s education and simulation programmes and runs the unit’s education website, INTENSIVE. He created the ‘Critically Ill Airway’ course and teaches on numerous courses around the world. He is one of the founders of the FOAM movement (Free Open-Access Medical education) and is co-creator of litfl.com, the RAGE podcast, the Resuscitology course, and the SMACC conference.
His one great achievement is being the father of three amazing children.
On Twitter, he is @precordialthump.
| INTENSIVE | RAGE | Resuscitology | SMACC

