Neuro 101: Cerebellum and Basal Ganglia
The Cerebellum and Basal Ganglia
The primary role of the cerebellum is to modulate the descending fibres of the corticospinal tract. It regulates muscle tone and coordination and controls posture and gait.
Cerebellar Lobes
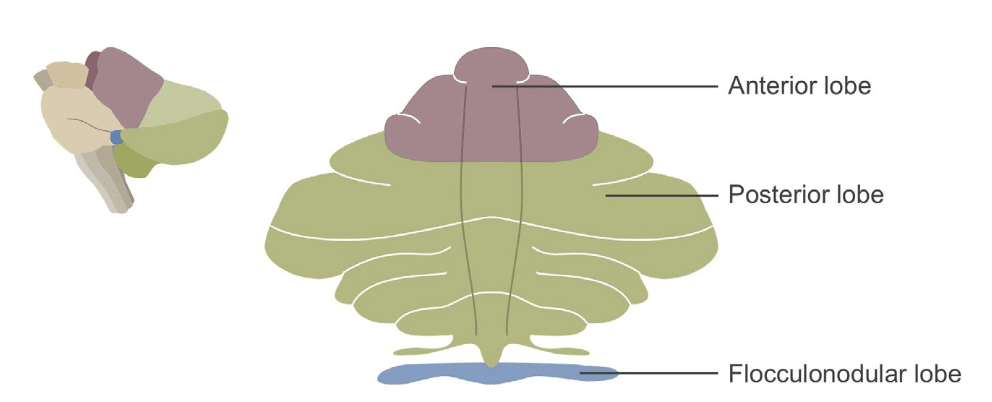
The cerebellum is divided into three lobes:
Anterior lobe
- Controls posture and muscle tone
- Receives input from the spinal cerebellar tracts
- Damage might produce ataxia of the limbs
Posterior lobe
- Controls coordination in skilled activities
- Receives input from the cortex
- Damage produces hypotonia and truncal ataxia
Flocculonodular lobe
- Concerned with equilibrium
- Receives input from the vestibular nuclei
- Damage produces nystagmus, vertigo, and difficulty with equilibrium
Functional Regions
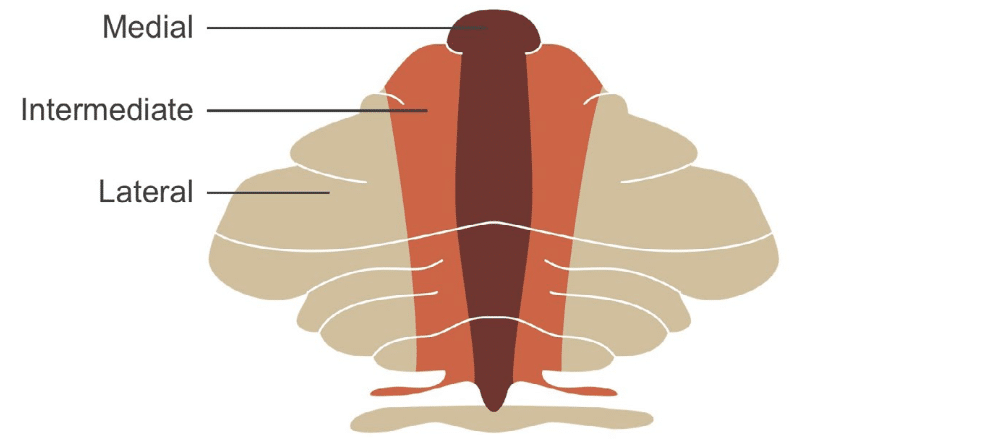
The cerebellum is also divided into three functional zones:
Medial
- Controls proximal and trunk muscles
- Controls vestibulo-ocular reflexes
- Damage causes gait unsteadiness and nystagmus with vertigo
Intermediate
- Controls distal muscles of appendages
- Damage causes appendicular ataxia
Lateral
- Controls motor planning for extremities
- Damage may affect fine motor skills
Cerebellar Connections
Three pairs of peduncles (inferior, middle, superior) connect the cerebellum to other parts of the nervous system.
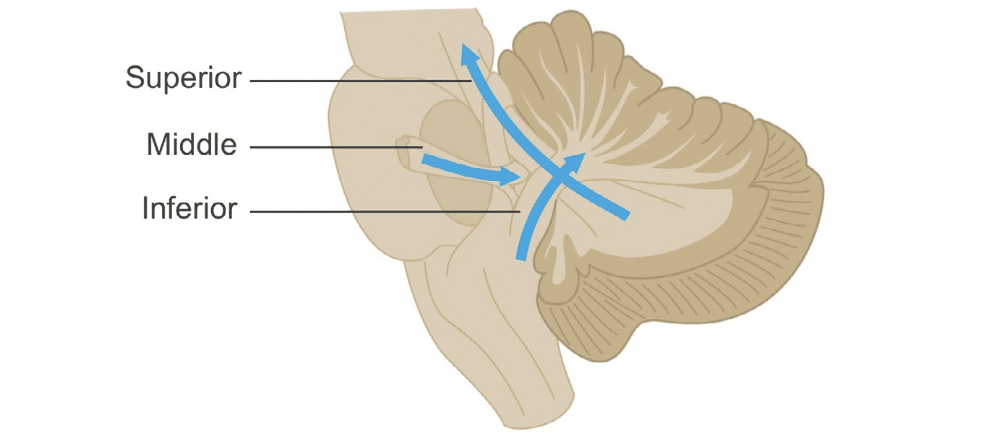
Input
- Mostly through inferior and middle peduncles
- Sensory input from brainstem, midbrain, and spinal cord
- Modulates cerebellar output
Output
- All arises from deep cerebellar nuclei
- All output is inhibitory
- Travels via superior cerebellar peduncle to cortex
Cerebellar Dysfunction
Signs include:
- Ipsilateral ataxia
- Decreased muscle tone
- Decreased reflexes
- Horizontal nystagmus
- Cerebellar dysarthria
- Intention tremor
Common Cerebellar Afflictions
Tonsillar Herniation
Increased intracranial pressure causes cerebellar tonsil herniation through foramen magnum → brainstem compression → coma and death.
Chiari Malformation (Type I)
Cerebellar tonsils displaced below foramen magnum. May develop syringomyelia. Symptoms: headache, high ICP, spinal cord signs, ataxia, vertigo, downbeat nystagmus.
Toxins (Ethanol)
- Acute: postural instability
- Chronic: vermis damage → truncal ataxia
- May be worsened by thiamine deficiency
Neoplasms
- Medulloblastoma (children)
- Astrocytoma
- Metastases
- Meningiomas
Signs: headache, vomiting, vision changes, ataxia, personality and cognitive changes, increased head size in children
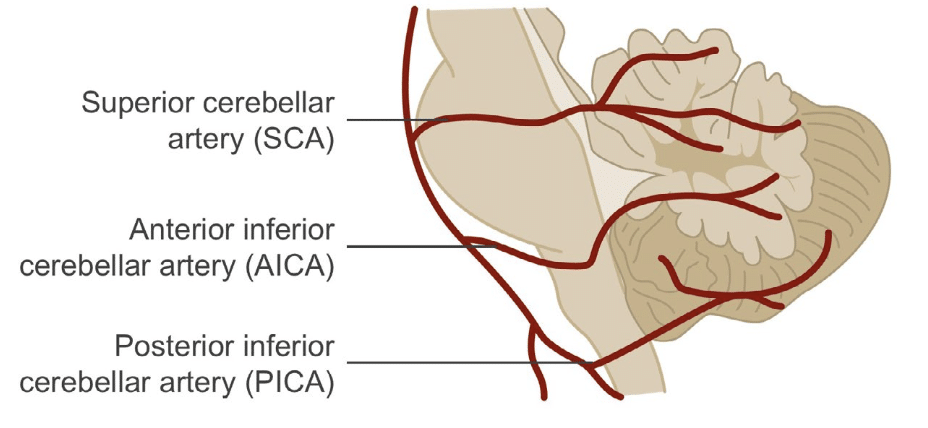
Cerebellar Stroke
- AICA/SCA: appendicular ataxia, nystagmus, nausea
- PICA (Wallenberg): vertigo, nystagmus, facial (ipsi) and body (contra) sensory loss
Other Pathologies
- Hypertensive haemorrhage: rapid ICP increase → herniation
- Degenerative: Friedreich’s ataxia, OPCA/MSA
The Extrapyramidal System
Not a true separate system, but refers to indirect control of movement via cerebellum and basal ganglia. Modulates corticospinal tract activity.
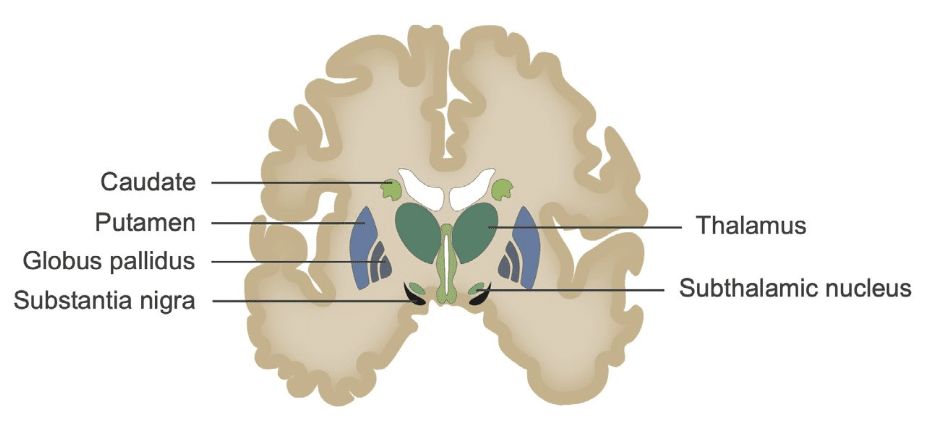
Basal Ganglia Structures
- Caudate + putamen = corpus striatum
- Thalamus is adjacent but not part of basal ganglia
Motor Pathways
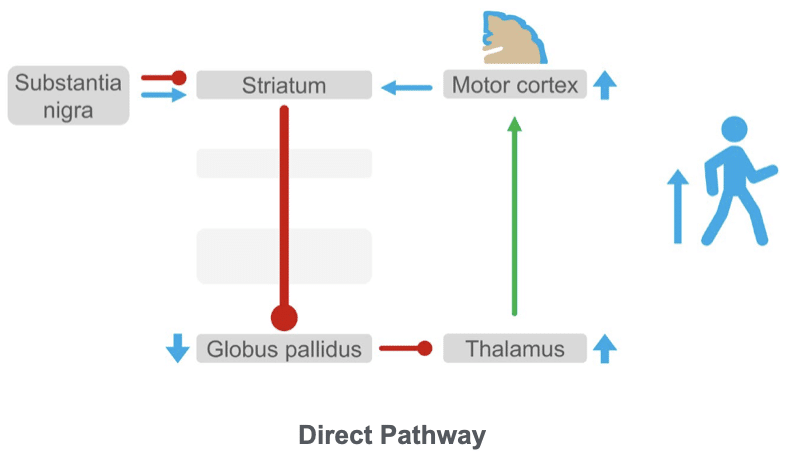
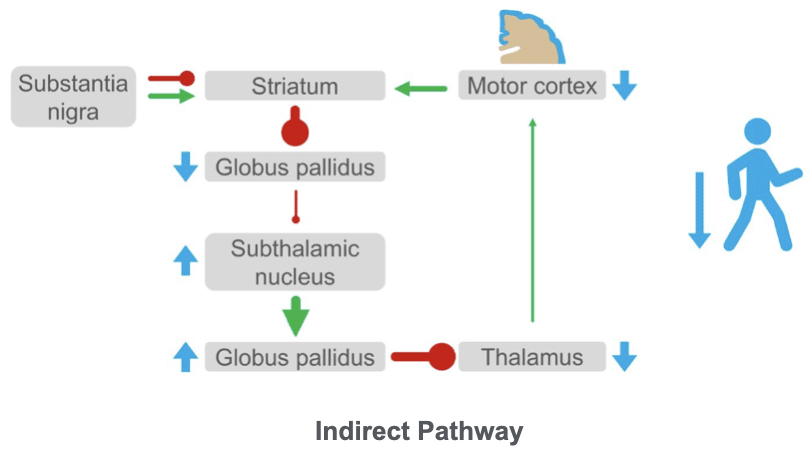
There are two pathways in the basal ganglia made up of interconnections, which form a series of feedback loops, all of which modulate motor activity.
Direct Pathway
- Globus pallidus internus inhibits thalamus
- Striatum suppresses this inhibition → increases motor activity
Indirect Pathway
- Striatum inhibits globus pallidus externus
- → less inhibition of subthalamic nucleus → more GPI activity → decreased movement
Dopaminergic System
- Substantia nigra → striatum (dopamine) → disinhibition of movement
- Acetylcholine has opposite effect (inhibits movement)
- Normally balanced with dopamine
Extrapyramidal Disorders
Hypokinetic Movement Disorders (Parkinsonism/Parkinson’s disease)
- Caused by loss of dopamine neurons in substantia nigra
- Indirect pathway becomes dominant → suppressed movement
Classic Signs
- Rigidity (cogwheeling)
- Rest tremor (pill-rolling)
- Postural tremor
- Bradykinesia
- Postural instability
- Festination
Examination
- Gait and facial expression
- Resting tremor (4–8 Hz)
- Cogwheeling on passive movement
- Retropulsion (pull test)
Hyperkinetic Movement Disorders
- Excessive movement: chorea, ballism, tics, dystonia
Huntington’s Disease
- Genetic, progressive
- Chorea, cognitive decline, psychiatric changes
- Loss of striatal neurons → favours direct pathway → increased movement
- Loss of GPI inhibition → thalamocortical hyperactivity
This is an edited excerpt from the Medmastery course Clinical Neurology Essentials by Robert Coni, DO, EdS, FAAN. Acknowledgement and attribution to Medmastery for providing course transcripts.
- Coni R. Headache Masterclass. Medmastery
- Simmonds GR. Neurology Masterclass: Managing Common Diseases. Medmastery
- Simmonds GR. Neurology Masterclass: Managing Emergencies. Medmastery
Clinical Neurology Essentials
- Coni R. Neuro 101: Neurological Examination. LITFL
- Coni R. Neuro 101: Cerebral Hemispheres. LITFL
- Coni R. Neuro 101: Cerebellum and Basal Ganglia. LITFL
- Coni R. Neuro 101: Brainstem. LITFL
- Coni R. Neuro 101: Cranial Nerves. LITFL
- Coni R. Neuro 101: Spinal Cord. LITFL
- Coni R. Neuro 101: Peripheral Nervous System. LITFL
References
Further reading
- Brazis PW, Masdeu JC, Biller J. Localization in Clinical Neurology. 8e 2021
- Campbell WW. DeJong’s The Neurologic Examination. 8e 2019
- Fuller G. Neurological Examination Made Easy. 6e 2019
- Kiernan J. Barr’s The Human Nervous System: An Anatomical Viewpoint. 10e 2015
- O’Brien M. Aids to the Examination of the Peripheral Nervous System. 6e 2023
- Patten JP. Neurological Differential Diagnosis. 2e 1996
- Waxman SG. Correlative Neuroanatomy. 23e 1996
Publications
- Boller F. Strokes and behavior: disorders of higher cortical functions following cerebral disease. Disorders of language and related function. Stroke. 1981 Jul-Aug;12(4):532-4.
- Brust JC, Shafer SQ, Richter RW, Bruun B. Aphasia in acute stroke. Stroke. 1976 Mar-Apr;7(2):167-74
- Carrera E, Michel P, Bogousslavsky J. Anteromedian, central, and posterolateral infarcts of the thalamus: three variant types. Stroke. 2004 Dec;35(12):2826-31.
- Datar S, Rabinstein AA. Cerebellar infarction. Neurol Clin. 2014 Nov;32(4):979-91
- Fama ME, Turkeltaub PE. Treatment of poststroke aphasia: current practice and new directions. Semin Neurol. 2014 Nov;34(5):504-13
- Fanciulli A, Wenning GK. Multiple-system atrophy. N Engl J Med. 2015 Jan 15;372(3):249-63.
- Kelly PJ, Stein J, Shafqat S, Eskey C, Doherty D, Chang Y, Kurina A, Furie KL. Functional recovery after rehabilitation for cerebellar stroke. Stroke. 2001 Feb;32(2):530-4.
- Kwong Yew K, Abdul Halim S, Liza-Sharmini AT, Tharakan J. Recurrent bilateral occipital infarct with cortical blindness and anton syndrome. Case Rep Ophthalmol Med. 2014;2014:795837
Neurology Library
Robert Coni, DO, EdS, FAAN. Vascular neurologist and neurohospitalist and Neurology Subspecialty Coordinator at the Grand Strand Medical Center in South Carolina. Former neuroscience curriculum coordinator at St. Luke’s / Temple Medical School and fellow of the American Academy of Neurology. In my spare time, I like to play guitar and go fly fishing. | Medmastery | Linkedin |

