Osgood-Schlatter disease
Description
Osgood–Schlatter disease (OSD) is an osteochondrosis or traction apophysitis of the tibial tubercle. OSD is common during the early adolescent growth spurt between 10 and 15 years of age, particularly in children who participate in sports that involve running and jumping. It is more common in males and may affect both knees.
OSD is a mostly self-limiting apophysitis of the tibial tubercle and the adjacent patella tendon in young active patients with open physis. A chronic fatigue injury due to repeated microtrauma at the patellar tendon insertion onto the tibial tuberosity.
Most cases resolve with supportive treatment including rest, ice and NSAID medications.
Prevention strategies include quadriceps and hamstring stretching and therefore should be implemented in everyday practice routines for children who partake in regular sports activities.
Radiographic features
Plain knee X-ray (lateral): In the early acute phase there is soft tissue swelling with a loss of the sharp margins of the patellar tendon. Later, bone fragmentation at the tibial tuberosity may be evident, usually 3 to 4 weeks after the onset.
Note: Isolated ‘fragmentation’ of the apophysis is not synonymous with OSD, as secondary ossification centres can occur.

Ultrasound: examination of the patellar tendon can demonstrate swelling of overlying soft tissues; thickening of the distal patellar tendon; infrapatellar bursitis; and fragmentation of the ossification centre
MRI: is the most sensitive and specific. MRI can demonstrate soft-tissue swelling anterior to the tibial tuberosity; loss of the sharp inferior angle of the infrapatellar fat pad; thickening and oedema of the distal patellar tendon; infrapatellar bursitis; and bone marrow oedema at the tibial tuberosity
History of Osgood-Schlatter disease
1878 – Odilon Marc Lannelongue (1840-1911) discussed ‘les ostéites apophysaires pendant la croissance‘. This in depth review outlines the condition it’s predominance in adolescence; differentiation from TB; and the long term benign nature of tibial tuberosity apophysitis
Le changement d’état des apophyses, leur transformation lente ou rapide, réclame pour se produire le concours d’une irritation physiologique active, poursuivant son but de substitution jusqu’à son dernier terme: l’ossification complète après croissance achevée.
Sous cette influence, et pendant toute sa durée, se trouve constituée une véritable prédispositon, une sorte d’imminence morbide. Dès ce moment les apophyses peuvent subir primitivement les mêmes atteintes que celles qui frappent ailleurs le tissuosseux.
The change of state of the apophyses, their slow or rapid transformation, calls for the co-operation of an active physiological irritation to occur, pursuing its goal of substitution until its last term: complete ossification after completed growth.
Under this influence, and throughout its duration, a veritable predisposition is constituted, a sort of morbid imminence. From this moment the apophyses can primitively undergo the same attacks as those which strike the osseous tissue elsewhere.
1891 Sir James Paget first described periostitis following strains in his Studies of Old Case-books
Much more common are the enlargements of the tubercle of the tibia which are often seen in young people much given to athletic games. They complain of aching pain at and about the part, especially during and after active exercise, and the tubercle may be felt enlarged and is often too warm. The pain often continues, more or less, for many months, and there may be enlargement of the bursa under the ligamentum patellae, and the tubercle may remain too prominent; but common as are these cases, especially in our public schools, I have never known grave mischief ensue in any of them, and they get well of themselves. They may represent one of the least degrees of periostitis due to strain; the increase of the prominence of the bone is only just beyond that which may be deemed the normal limit for the attachment of vigorous muscles.
Paget 1891
1903 The American orthopedist, Robert Bayley Osgood (1873–1956), wrote about bone changes on the tibial tubercle with a review of 10 patients in his time as a roetgenologist at Boston Children’s Hospital. “Lesions of the tibial tubercle occurring during adolescence” published in the Boston Medical and Surgical Journal
It is possible, however, to have a partial separation of the tubercle and the interference with normal function be so slight that the condition is often unrecognized and the diagnosis made of a bursitis or a periostitis, or even a joint fringe (see fig 5, 6). The x-ray evidence of this is apparently indisputable and the clinical picture absolutely consistent with the true condition.
Osgood advised conservative management and that:
…complete immobilisation for 6-8 weeks uniformally brought about a return to practically normal function…even though the fragment is not completely restored to it’s normal position.
Osgood 1903
1903 Swiss surgeon Carl B. Schlatter (1864-1934) published “Verletzungen des schnabelförmigen Forsatzes der oberen Tibiaepiphyse” [Injuries of the beak-shaped appendage of the upper tibial epiphysis] and the condition was later termed ‘Schlatterschen Krankheit‘. Schaltter observed 7 patients with separation of the anterior rostrate (beak) process from the upper tibia noting that
…these injuries represent a clinically sharply delineated profile of the disease whose symptom complex is in most cases simple and easy to diagnose without the use of radiographs
Schlatter 1903
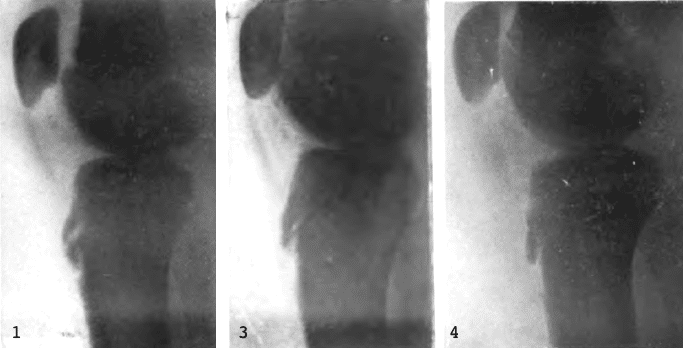
- Fig 1. Hakenförmiger Fortsatz eleviert und seine Spitze abgebrochen.
- Fig 3. Breite Spalte zwischen dem abgebrochenen Epiphysenfortsatz und der Tibiadiaphyse.
- Fig 4. Unteres Ende des Epiphysenfortsatzes abgehoben, vordere Tibiakante unterhalb der Epiphysenspitze nnregelmässig konturiert.
- Fig 1. Hook-shaped extension elevated and its tip broken off.
- Fig 3. Wide gap between the broken epiphyseal process and the tibial diaphysis.
- Fig 4. Lower end of the epiphyseal process lifted off, the anterior tibial edge below the epiphyseal tip irregularly contoured.
1905-1911 Variably termed Schlatter’s sjukdom / Schlatter’s disease and finally Osgood-Schlaltersche Erkrankung (1910) and in American Journals Osgood-Schlatter disease from 1911
Associated Persons
- Odilon Marc Lannelongue (1840 – 1911)
- Sir James Paget (1814 – 1899)
- Carl B. Schlatter (1864 – 1934)
- Robert Bayley Osgood (1873 – 1956)
Alternative names
- Apophysitis of the tibial tubercle
- Osteochondrosis of the tibial tuberosity
- Lannelongue’s disease
- Lannelongue-Osgood-Schlatter disease
- Schlatterschen Krankheit; Schlatter’s sjukdom; Schlatter’s disease.
References
Historical references
- Lannelongue OM. Note sur les ostéites apophysaires pendant la croissance. Bulletins et mémoires de la société de chirurgie de paris. 1878. Tome IV pp162 and pp276
- Paget J. Studies of Old Case-books. Longmans, Green. 1891
- Osgood RB. Lesions of the tibial tubercle occurring during adolescence. Boston Medical and Surgical Journal 1903; 148: 114-117
- Schlatter C. Verletzungen des schnabelförmigen Forsatzes der oberen Tibiaepiphyse. Beitrage zur klinischen Chirurgie, 1903; 38: 874-887
- Haglund P. Concerning some rare but important surgical injuries brought on by violent exercise. [Schlatter’s disease.] Lancet 1908; 172(4427): 12-15
- Kienbttck R. Ueber Osteochondritis an der Tuberositas tibiae und die sogeiiannte Osgood-Schlaltersche Erkrankung. Fortschritte auf dem Gebiete der Röntgenstrahlen und der Nuklearmedizin. 1910; 15: 135-139.
Article reviews
- Tubby AA. Orthopaedic surgery: the Osgood-Schlatter disease. The Practitioner. 1912; 89: 56-60
- Tibia (Anterior apophysis of Thickening of) [Osgood- Schlatter disease, 1903] Index-catalogue of the Library of the Surgeon-General’s Office, United States Army. Authors and subjects 1913; II(18): 252 (Series 2, Volume 18)
- Nowinski RJ, Mehlman CT. Hyphenated history: Osgood-Schlatter disease. Am J Orthop (Belle Mead NJ). 1998; 27(8): 584-5.
- Ladenhauf HN, Seitlinger G, Green DW. Osgood-Schlatter Disease: A 2020 Update of a Common Knee Condition in Children. Curr Opin Pediatr. 2020 Feb;32(1):107-112.
- Knipe H. Osgood-Schlatter disease. Radiopaedia
[cite]
eponymictionary
the names behind the name
Resident medical officer in emergency medicine MB ChB (Uni. Dundee) MRCS Ed. Avid traveller, yoga teacher, polylinguist with a passion for discovering cultures.


