Paraquat toxicity
Paraquat is a widely used herbicide and is unique in toxicology for a couple of reasons. Firstly supplemental oxygen should be avoided due to the risk of developing oxygen free radicals. Secondly treatment does not follow the usual RRSIDEAD approach, patients require immediate decontamination to prevent a lethal outcome.
Toxic Mechanism:
It is a caustic agent that is specifically transported into pneumocytes, where oxygen free radicals are produced resulting in lipid peroxidation and damage to the cell membranes.
Toxicokinetics:
- Rapid but incomplete absorption
- Peak blood levels occur within 2 – 4 hours.
- Absorption is reduced by the presence of food in the stomach.
- Inhalation or dermal exposures cause minimal absorption (you would need a prolonged time with high concentrations or broken skin to risk any systemic toxicity).
- Paraquat redistributes to highly vascular tissues (kidney, liver, heart, muscle and lungs). It is not metabolised.
- Excreted in the urine
Resuscitation:
- This is the only poisoning where decontamination takes priority over resuscitation or transport to hospital. If possible this should be done on scene.
- Do not administer supplemental oxygen unless oxygen saturations are <90%, only titrate to achieve saturations of 91% (no greater).
- Airway compromise: Stridor, dysphagia and dysphonia indicate airway injury and should be intubated early.
Risk Assessment
- Patients who are unstable after an deliberate self-poisnong with a large ingestion should be palliated once the diagnosis is established
- The aim of management is to reduce the risk of morbidity and mortality in those with moderate or accidental exposures via early decontamination and haemodialysis.
- Survival after an acute paraquat poisoning is related to dose and circumstances (intentional versus accidental). A mouthful may cause toxicity but a splash or a taste is unlikely. Dermal exposures require high concentrations or damaged/broken skin to be of concern. Inhalation does not cause toxicity.
- The risk assessment can be further refined using urinary and serum paraquat assays.
- In children a teaspoonful of 5ml may be fatal.
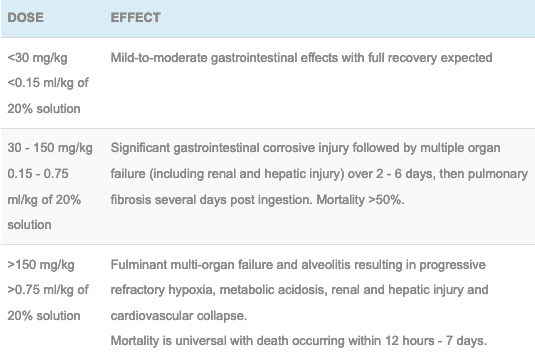
- Dose-related risk assessment table:
- Clinical features range from the following:
- Clinically well with oral burns
- Central tongue ulceration “Paraquat tongue” and gastrointestinal symptoms are universal (patients can develop perforations and mediastinitis).
- Moderate ingestions may not develop systemic features in the first 48 hours. Typically they will have increasing dyspnoea and hypoxia as alveolitis and then pulmonary fibrosis occurs. This will progress over days to weeks and may result in death. If the patient survives they will also develop renal injury during this course that typically resolves.
- Large ingestions will result in multi-organ failure, initial signs include; tachycardia, tachypnoea, metabolic acidosis and rising lactate. Followed by cardiovascular collapse and death within 24 hours in severe cases.
Supportive Care
- Agitation: titrated doses of benzodiazepines are effective e.g. diazepam 2.5 – 5 mg every 5 minutes IV until gentle sedation is achieved
- If intubated consider FASTHUGSINBED Please
Investigations
- Screening: 12 lead ECG, BSL, Paracetamol level
- Specific:
- Regular oxygen saturations.
- Serial pulmonary function testing for signs of alveolitis or pulmonary fibrosis
- Acid-base status, FBC, EUC, LFTs, lipase, lactate (lactate >4.4 mol/L without another cause is often fatal)
- CXR to detect fibrosis and aspiration
- CT chest/abdo
- Endoscopy
- Urinary paraquat test – if positive (turns blue) confirms ingestion but not plasma level. Urine, dialyse and gastric fluids can be used. It is reliable if performed within 12 hours of ingestion (although can remain positive for days in large ingestions).
Decontamination:
- Fullers earth (non-plastic clay): 30%, 250mL Q 4 hourly -> until comes out in stools but is rarely available
- Alternatively Activated Charcoal is just as effective 50 gram PO (1 g/kg in children).
- First aid on the scene can involve any food to reduce absorption.
Enhanced Elimination
- Haemodialysis or haemoperfusion should be started immediately for those who have ingested more than a splash or lick and less than a lethal dose. It is only beneficial before the paraquat has redistributed to the tissues therefore within 4 hours post ingestion.
Antidotes
- None available
- Semi-experimental therapies to reduce inflammation involve:
- N-acetylcystine
- Dexamethasone 8 mg TDS IV
- Salicyclic acid 100 mg/kg/day in divided doses
Disposition
- Patients who are clinically well 6 – 12 hours post exposure without oral burns and a negative urinary test have not absorbed paraquat systemically and can be discharged.
- Patients with a moderate or accidental ingestion should be observed in ICU and the above investigations and treatments selected as appropriate.
- Patients who have had a massive ingestion (i.e. >100ml of 20% solution) and early clinical features of toxicity should be palliated from the outset.
References and Additional Resources:
Additional Resources:
- CCC – Paraquat
References:
- Dinis-Oliveira PJ et al. Paraquat poisonings: mechanisms of lung toxicity, clinical features and treatment. Critical Reviews in Toxicology 2008; 38:13-71.
- Eddleston M, Wilks MF, Buckley NA. Prospects for treatment of paraquat–induced lung fibrosis with immunosuppressive drugs and the need for better prediction of outcome: a systematic review. Quarterly Journal of Medicine. 2003; 96(11):809-824.
- Gawarammana IB, Buckley NA. Medical management of paraquat ingestion. British Journal of Pharmacology 2011; 5:745-757
- Senarathna L, Eddleston M, Wilks MF. Prediction of outcome after paraquat poisoning by measurement of the plasma paraquat concentration. Quartery Journal of Medicine 2009; 102:251-259.

Toxicology Library
DRUGS and TOXICANTS
Dr Neil Long BMBS FACEM FRCEM FRCPC. Emergency Physician at Kelowna hospital, British Columbia. Loves the misery of alpine climbing and working in austere environments (namely tertiary trauma centres). Supporter of FOAMed, lifelong education and trying to find that elusive peak performance.