Pyroglutamic Acidosis
OVERVIEW
- Pyroglutamic acidosis is a rare cause of high anion gap metabolic acidosis (HAGMA)
- pyroglutamic acid is also known as 5-oxoprolinemia
- produced from γ-glutamyl cysteine by the enzyme γ-glutamyl cyclotransferase
- catabolised by 5-oxoprolinase
- when glutathione levels are low, the activity of γ-glutamyl cyclotransferase is increased, resulting in pyroglutamic acid accumulation in glutathione-depleted states
CAUSE
Risk factors
- elderly
- paracetamol use (glutathione depletion by its metabolite NAPQI)
- sepsis (depletion of glutathione)
- flucloxacillin (inhibits 5-oxoprolinase)
- hepatic and renal impairment
- malnutrition
- pregnancy
- vigabatrin
- congenital enzyme deficiencies (glutathione synthase deficiency)
Pyroglutamic acidosis results from disruption of the γ-glutamyl cycle
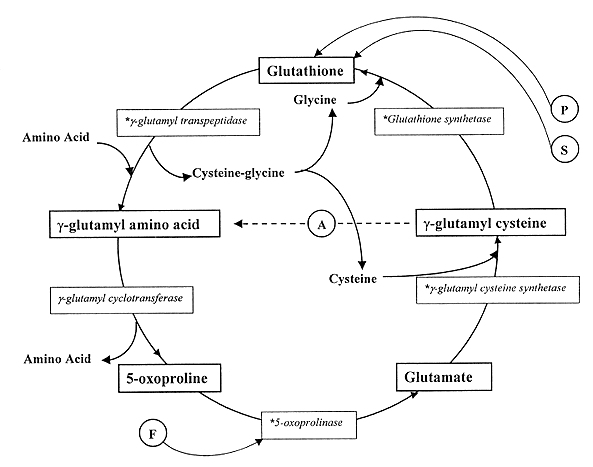
- 5-oxoproline (aka pyroglutamic acid) is produced from γ-glutamyl cysteine by the enzyme γ-glutamyl cyclotransferase
- γ-glutamyl cyclotransferase activity increases when glutathione levels are low, due to a loss of feedback inhibition from glutathione
- accumulation of pyroglutamic acid is thought to be due to depletion of the glutathione, particularly when glutathione synthetase is inhibited
- Decreased activity of 5-oxoprolinase, which breaks down pyroglutamic acid, may also play a role
CLINICAL FEATURES
- manifestations of acidaemia
- e.g. tachycardia, tachypnoea, altered level of consciousness
- presence of risk factors
- features of underlying cause
INVESTIGATIONS
- high anion gap metabolic acidosis (HAGMA) on blood gas
- normal osmolar gap
- normal lactate
- normal beta-hydroxybutyrate
- high pyroglutamic acid (urine or blood)
MANAGEMENT
- stop exacerbating factors
- treat sepsis, including:
- early and appropriate antibiotics
- source control
- supportive care and monitoring
- intubation, ventilation, renal replacement therapy (RRT) as indicated
- N-acetylcysteine
- help replenish glutathione stores
References and Links
LITFL
- Metabolic Muddle 004 — Staph sepsis and an unusual metabolic acidosis
Journal articles
- Dempsey GA, Lyall HJ, Corke CF, & Scheinkestel CD (2000). Pyroglutamic acidemia: a cause of high anion gap metabolic acidosis. Critical care medicine, 28 (6), 1803-7 [pubmed]
- Mizock BA, & Mecher C (2000). Pyroglutamic acid and high anion gap: looking through the keyhole? Critical care medicine, 28 (6), 2140-1 [pubmed]
- Peter JV, Rogers N, Murty S, Gerace R, Mackay R, & Peake SL (2006). An unusual cause of severe metabolic acidosis. The Medical journal of Australia, 185 (4), 223-5 [pubmed]

Critical Care
Compendium
Chris is an Intensivist and ECMO specialist at The Alfred ICU, where he is Deputy Director (Education). He is a Clinical Adjunct Associate Professor at Monash University, the Lead for the Clinician Educator Incubator programme, and a CICM First Part Examiner.
He is an internationally recognised Clinician Educator with a passion for helping clinicians learn and for improving the clinical performance of individuals and collectives. He was one of the founders of the FOAM movement (Free Open-Access Medical education) has been recognised for his contributions to education with awards from ANZICS, ANZAHPE, and ACEM.
His one great achievement is being the father of three amazing children.
On Bluesky, he is @precordialthump.bsky.social and on the site that Elon has screwed up, he is @precordialthump.
| INTENSIVE | RAGE | Resuscitology | SMACC
