Reports of therapeutic hypothermia’s death are greatly exaggerated
I expect you’re completely #FOAMed out by the post-publication frenzy stirred up by the TTM Trial.
If not, you’ve come to the right place!
Mike collated the explosion of initial FOAM responses in All in a lather over TTM and there have since been notable additions such as Scott Aberegg’s Chill Out: Homeopathic Hypothermia after Cardiac Arrest… and ICN’s interview with TTM investigators Niklas Nielsen and Anders Aneman one week after TTM. Soon after, Charles Bruen came with his fascinating blogpost/podcast putting the latest studies in historical perspective: Therapeutic hypothermia: The history of general refrigeration.
Meanwhile I’ve been involved in discussions via Google Hangouts, reading what the big brains on the CCM-L listserv have written, been asking questions of one of the authors, and generally trying to get to grips with the strengths, weakness and implications of this study.
So, have we entered the age of ‘homeopathic hypothermia’ as Scott Aberegg suggests tongue-in-cheekily? Or is there still life in therapeutic hypothermia post-arrest?
I’ll start with the bottom line:
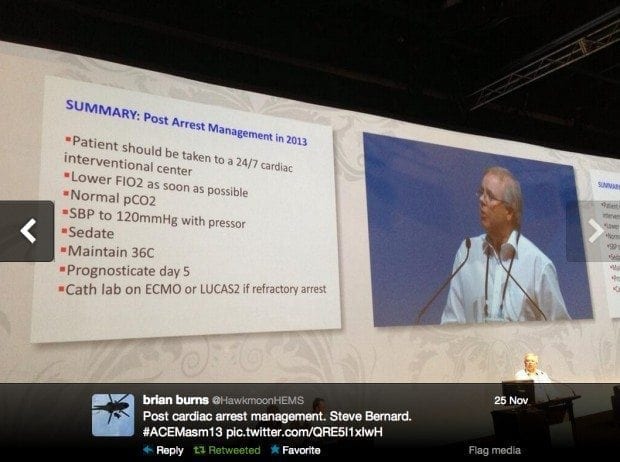
If T36C is good enough for Stephen Bernard, it’s good enough for me too (plus he’s my boss)
Here is the summary of the TTM trial from the newly updated LITFL CCC page on this topic:
- MCRCT, stratified according to site, no allocation concealment
- 36 ICUs in Europe and Australia
- modified intention-to-treat analysis
- n= 939 (T33C: 473 vs T36C: 466 patients in the primary analysis)
- Population:
— inclusion criteria: Age ≥18y, OOHCA of presumed cardiac cause, sustained ROSC for 20 minutes, GCS <8 after sustained ROSC
— exclusion criteria: . pregnancy, known bleeding diathesis (other than medically induced coagulopathy, e.g. warfarin), suspected or confirmed acute intracranial bleeding or acute stroke, unwitnessed cardiac arrest with initial rhythm asystole, known limitations in therapy and Do Not Resuscitate-order, known disease making 180 days survival unlikely, known pre-arrest Cerebral Performance Category 3 or 4, >4 hours from ROSC to screening, SBP <80 mm Hg in spite of fluid loading/vasopressor and/or inotropic medication/intra aortic balloon pump, temperature on admission <30°C - Intervention: TTM at T33C (cooled my various means to target <6hours, maintained T33C for 36h, then rewarmed at 0.25C per hour; fever actively managed until at least 72 hours after cardiac arrest)
- Comparison: TTM at T36C (otherwise similar treatment to the intervention group)
- Outcomes:
— Primary: mortality at 180 days
— Secondary: composite of poor neurologic function or death, defined as a Cerebral Performance Category (CPC) of 3 to 5 and a score of 4 to 6 on the modified Rankin scale, at or around 180 days (there were also others such as duration of mechanical ventilation, see below) - Results:
— no difference in mortality: 50% of the T33C (235 of 473 patients) had died, as compared with 48% of the patients in the 36°C group (225 of 466 patients) (hazard ratio with a T33°C, 1.06; 95%CI 0.89-1.28; P=0.51)
— no difference in neurological outcomes: 54% of the T33C group versus 52% of the 36C group died or had poor neurologic function according to the CPC (RR, 1.02; 95% CI 0.88 to 1.16; P=0.78). Using the modified Rankin scale, the comparable rate was 52% in both groups (RR 1.01; 95% CI 0.89 to 1.14; P=0.87).
— shorter duration of mechanical ventilation in the T36C group: T33C = 0.83 versus T33C = 0.76 median days receiving mechanical ventilation/days in ICU (P=0.006)
— serious adverse effects were common and marginally higher (with borderline significance) in the T33C group (93%) compared with the T36C (90%) (RR 1.03; 95% CI 1.00 to 1.08; P=0.09)
— higher rates of hypokalemia in T33C group (19%) than the T36C group (13%) P=0.02)
— no differences found in subgroup analyses: age > 65 years, presence of initial shockable rhythm, time from cardiac arrest to ROSC >25 min, and presence of shock at admission
— no differences in shivering
— during the first 7 days of hospitalization, life-sustaining therapy was withdrawn in 247 patients (132 in the 33°C group and 115 in the 36°C group) - Commentary and criticisms
— this study is a methodological masterpiece!
— unlike Bernard 2002 and HACA 2002, not just VT/VF OOHCA were included (~80% were VF/VT)
— a useful standardised protocol for neurological prognostication and treatment withdrawal was used
— survival rates of about 50% may seem high, but remember that this applies to patients who have achieved ROSC for a minimum of 20 minutes}
— the study was powered to detect a RRR of 20% or an ARR of ~11%, thus the study was not powered to detect a smaller treatment effect (this may be more realistic due to the lower ‘separation effect’ between T33C and T36C compared to the earlier Bernard and HACA studies)
— less than 50% of T33C patients had reached target at 6 hours, but there was good separation between T33C and T36C groups
— Baseline balance: higher rates of previous MI and IHD in the T33C group, but no difference in the rates of interventions for these conditions
— the true patient-orientated outcome that matters is neurologically intact survival, the authors didn’t use this as the primary outcome because mortality is a ‘harder endpoint’ and less subject to bias
— staff caring for the patients could not be blinded; however the doctors who perform neurological prognostication and data interpretation for the study were
— TTM differs to the Bernard 2002 and HACA 2002 trials: larger MCRCT with excellent methodology, not limited to VT/VF, control group still received TTM (but at T36C) - Bottom line: No difference found between targeted temperature management with a target of T36C compared to T33C
Putting this study in perspective
I’ll say it again, this study is a methodological masterpiece. It differs from the two famous practice-changing but flawed papers published in the NEJM in 2002 (Bernard et al, 2002 and the HACA trial) in that it is much bigger, was not restricted to VT/VF only and had targeted temperature management in both the intervention and comparison group. Of note, the previous studies had no specific protocols for management of patients in the control arm, and included significant numbers of patients that became febrile. Finally, TTM was powered to determine an absolute difference in mortality of 11% between the two groups (a big difference) — there might be a smaller difference that has gone undetected (but there aren’t even any trends or weak signals supporting this) — and it was not powered for the more important patient-centered outcome of neurologically intact survival.
What are the possible explanations for the result of this trial?
TTM might work, at either T33C or T36C, because of avoidance of hyperthermia (leading to decreased metabolic demand and fever-related tissue injury) or simply through a reduction in metabolic demand (e.g. prevention of fever, seizure control, cooling, sedation and neuromuscular blockade).
T33C might conceivably be slightly more effective, but less than this study was powered to detect. Various physiological plausible mechanisms have been proposed for therapeutic hypothermia, including effects on excitotoxicity, neuroinflammation, apoptosis, free radical production, seizure activity, blood-brain barrier disruption, blood vessel leakage and cerebral thermopooling… As I’m prone to say, the problem with physiological plausibility is that everything is plausible when our understanding of physiology is incomplete.
TTM at any temperature may not confer any benefit, it might simply be associated with the improved overall care resulting from focusing the coordinated efforts of an expert team, with close monitoring and prioritisation of therapies, on a critically ill patient.
So, what do we do now?
As clinicians we need to get together with your colleagues and review our post-arrest protocols. I expect most centers will shift to a target of T36C based on the findings of TTM and the possible benefits of simplifying post-arrest care. One concern I have is that the patients managed at T36C may be at risk if there is a lapse in temperature control. In other words, these patients may be more likely to develop a fever. Strict adherence to the assigned temperature target should remain a strictly targeted goal of post-arrest care protocols.
Despite this pragmatic solution to the dilemma of what to do now, many uncertainties remain. Even if there truly is no difference as found in this study, there are still numerous unanswered questions:
- What is the optimum target temperature? (If T33C and T36C are equivalent, what is the shape of the curve on which they lie? T34C might be better, for instance)
- Does it matter when cooling is started? (prehospital, during CPR, post-ROSC?)
- What is the optimum duration of targeted temperature management? How long should we actively avoid fever for?
- What is the optimum rate of rewarming? (less of an issue with TTM at T36C!)
- Is TTM at any temperature really beneficial over not worrying about the temperature? (previous studies would suggest yes, but how definitive are these?)
- Should VT/VF be treated differently to non-VT/VF? What about in-hospital cardiac arrests? What about different underlying causes?
- Should some patients have different target temperatures?
- What does all this mean in the ECMO era?
The list of questions is daunting to read. Additional RCTs are already underway investigating various aspects of TTM, but I wonder whether traditional RCTs are going to be able to answer many of these questions. Perhaps new trial designs, such as adaptive trials, may provide some of the answers. A researchers work, it would seem, is never done.
Therapeutic hypothermia may look dead at first glance, but what seems like rigor mortis is just a radical facelift. We still have targeted temperature management, but the target has changed to a temperature of 36C.
References and Links
LITFL
- All in a lather over TTM (2013)
- CCC — Prognosis after cardiac arrest
- CCC — Post-cardiac arrest syndrome
- CCC — Post Cardiac Arrest Care
- CCC — Targeted temperature management after cardiac arrest
Journal articles
- Bernard SA et al. Treatment of comatose survivors of out-of-hospital cardiac arrest with induced hypothermia. N Engl J Med 2002;346:557-63. doi: 10.1056/NEJMoa003289
- The Hypothermia after Cardiac Arrest Study Group. Mild therapeutic hypothermia to improve the neurologic outcome after cardiac arrest. N Engl J Med 2002;346:549-56. doi: 10.1056/NEJMoa012689
- Nielsen N et al. Targeted temperature management at 33°C versus 36°C after cardiac arrest. N Engl J Med Nov 17 2013 doi: 10.1056/NEJMoa1310519
- Rittenberger JC, Callaway CW. Temperature Management and Modern Post–Cardiac Arrest Care. N Engl J Med Nov 17 2013 doi: 10.1056/NEJMe1312700

Critical Care
Compendium
Chris is an Intensivist and ECMO specialist at The Alfred ICU, where he is Deputy Director (Education). He is a Clinical Adjunct Associate Professor at Monash University, the Lead for the Clinician Educator Incubator programme, and a CICM First Part Examiner.
He is an internationally recognised Clinician Educator with a passion for helping clinicians learn and for improving the clinical performance of individuals and collectives. He was one of the founders of the FOAM movement (Free Open-Access Medical education) has been recognised for his contributions to education with awards from ANZICS, ANZAHPE, and ACEM.
His one great achievement is being the father of three amazing children.
On Bluesky, he is @precordialthump.bsky.social and on the site that Elon has screwed up, he is @precordialthump.
| INTENSIVE | RAGE | Resuscitology | SMACC
