Sciatic nerve lesions
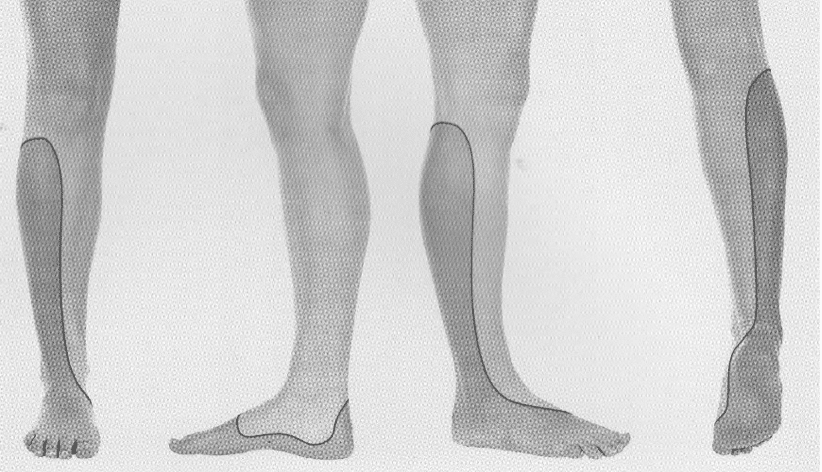
Sciatic nerve lesions cause motor loss below the knee and sensory loss in the foot and leg. Most commonly injured in the buttock, often from trauma or injection.
The sciatic nerve is the largest nerve in the body.
It provides motor innervation to:
- The muscles of the posterior compartment of the thigh (via its main trunk)
- The muscles in the posterior compartment of the leg and sole of the foot (via the tibial nerve)
- The muscles in the anterior and lateral compartments of the leg (via the common peroneal nerve)
It also provides sensory innervation to:
- The lateral leg
- Foot
Injury to the sciatic nerve is a catastrophic injury and typically produces loss of sensation to the lateral leg and the foot and loss of motor function to the hamstrings and the leg below the knee.
It is particularly vulnerable to injury in the region of the mid-buttock.
Anatomy
Course of the sciatic nerve
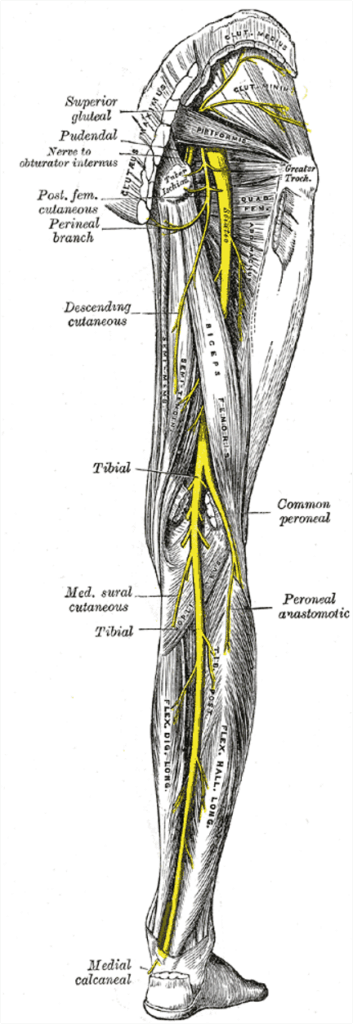
The sciatic nerve arises from the sacral plexus.
It is derived from the anterior divisions of the lumbosacral plexus (L4,5 S1,2,3).
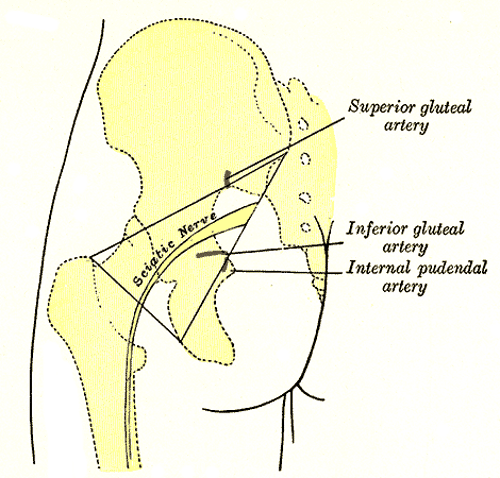
The nerve exits the pelvis via the greater sciatic foramen below the piriformis muscle.
It emerges midway between the posterior superior iliac spine (PSIS) and the ischial tuberosity—an important surface landmark. Intramuscular injections must be given in the upper outer quadrant of the buttock to avoid nerve injury.
The nerve continues down the thigh between the ischial tuberosity and greater trochanter, running deep to gluteus maximus and superficial to various deep muscles before dividing into the tibial and common peroneal nerves in the distal third of the thigh.
(Gray’s Anatomy, 1918).
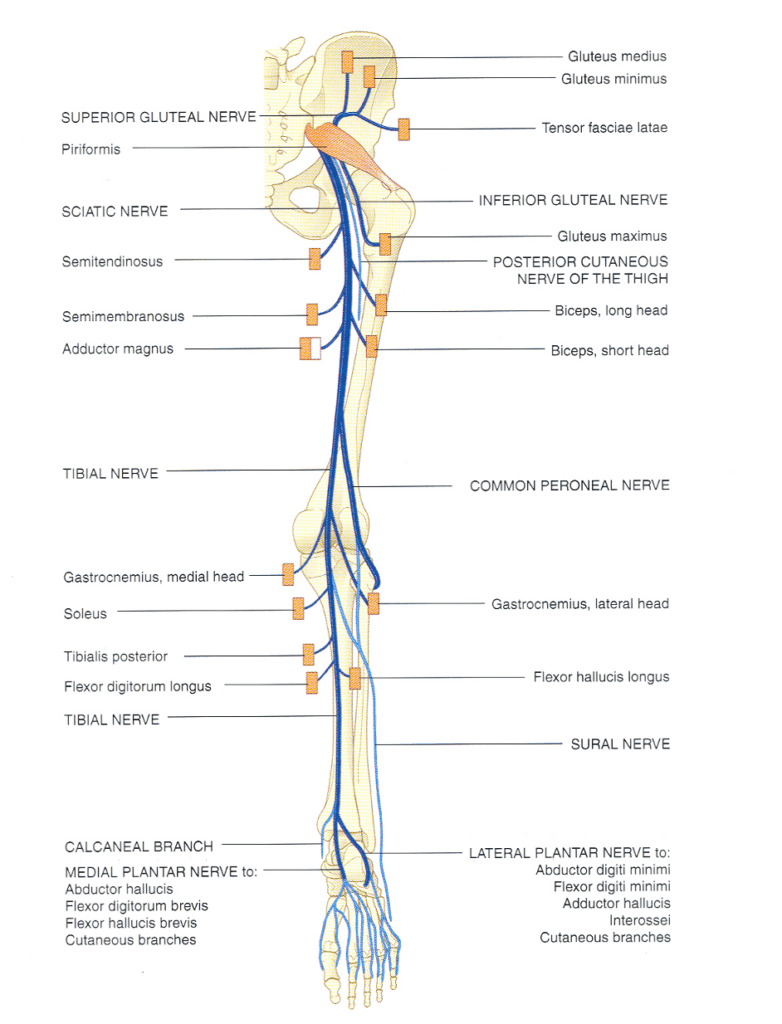
Sciatic nerve innervations
Main trunk (prior to division):
Motor: Muscular branches are distributed to the hamstring muscles
- Biceps femoris
- Semitendinosus
- Semimembranosus
- Hamstring portion of adductor magnus
Sensory:
- Articular branches to the hip joint
Tibial nerve (branches and distributions):
Popliteal fossa:
- Motor
- Soleus
- Gastrocnemius
- Popliteus
- Plantaris
- Sensory:
- Knee joint
- Medial sural cutaneous nerve → Sural nerve (just behind the knee) → Lateral border of foot to the lateral border of the little to
Below popliteal fossa:
- Motor
- Flexor digitorum longus
- Flexor hallucis longus
- Tibialis posterior
- Sensory:
- Ankle joint
- Medial calcaneal nerve → Medial heel and as well as its medial plantar surface
Beneath the flexor retinaculum of the medial ankle, the tibial nerve divides into two terminal branches. Terminal branches at ankle:
- Medial plantar nerve
- Motor: abductor hallucis, flexor digitorum brevis, flexor hallucis brevis, 1st lumbrical
- Sensory: medial sole and medial 3½ toes (including nail beds)
- Lateral plantar nerve
- Motor: quadratus plantae, abductor digiti minimi
- Superficial branch: flexor digiti minimi brevis, 4th interosseous
- Deep branch: adductor hallucis, 2nd–4th lumbricals, 1st–3rd interossei
- Sensory: lateral sole and lateral 1½ toes
- Motor: quadratus plantae, abductor digiti minimi
Common peroneal nerve (before and after division)
Pre-division branches:
- Peroneal communicating nerve → joins medial sural cutaneous to form sural nerve
- Lateral sural cutaneous nerve → lateral leg
- Short head of biceps femoris
- Knee joint
Superficial peroneal nerve
- Motor: peroneus longus, peroneus brevis
- Sensory: dorsum/lateral foot, lateral 3½ toes
Deep peroneal nerve
- Motor: tibialis anterior, extensor digitorum longus, extensor hallucis longus, extensor digitorum brevis, peroneus tertius
- Sensory: 1st webspace
Pathology
Causes of sciatic nerve lesions
- Trauma
- Posterior hip dislocation, pelvic fractures, intramuscular injections
- Neuropraxias
- Compartment syndromes (incomplete in original)
- Mass lesions
- Tumours
- Abscesses
- Neuropathies
- Diabetes mellitus (microvascular ischaemia)
- Malignancy (compression, paraneoplastic)
- Infections: leprosy, HIV
- Connective tissue diseases: RA, SLE, PAN, scleroderma, sarcoidosis
- Others: amyloidosis, Lyme disease, heavy metal poisoning
Clinical assessment
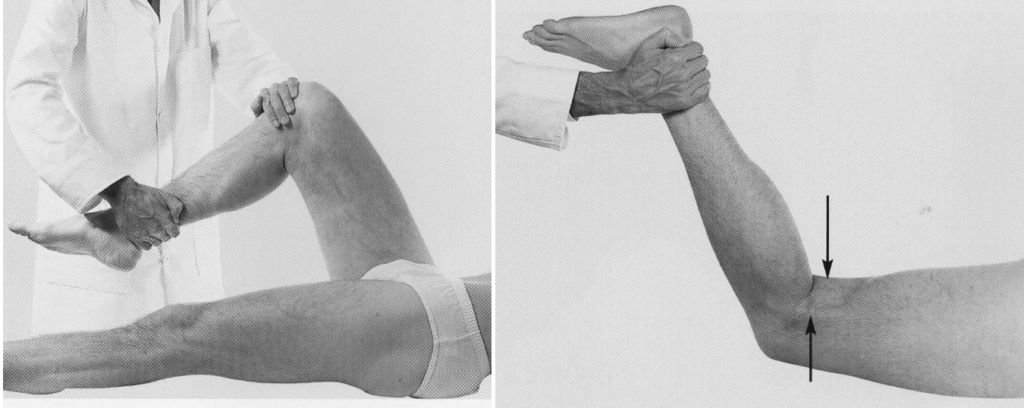
Right: Alternatively: The patient lies prone and flexes the leg at the knee against resistance. Arrows show the tendons of biceps femoris (laterally) and semitendinosus (medially), which can be felt and usually seen.
Investigations
Blood tests
- FBC
- U&Es / glucose
- CRP
- ESR
- Others as indicated (e.g. lead levels)
Nerve conduction studies
- Confirm diagnosis
- Rule out generalised disease
- Assess severity and prognosis
CT/MRI
- To evaluate mass lesions or nerve integrity
Management
General principles
- Treat underlying cause
- Fasciotomy for compartment syndrome
- Remove iatrogenic causes
- Occupational therapy for support devices
- Physiotherapy for function and complication prevention
Disposition
Depends on:
- Cause of lesion
- Severity of symptoms
- Acuteness of onset
Appendix 1
Appendix 2
References
Publications
- Brazis PW, Masdeu JC, Biller J. Localization in Clinical Neurology. 8e 2021
- Fuller G. Neurological Examination Made Easy. 6e 2019
- O’Brien M. Aids to the Examination of the Peripheral Nervous System. 6e 2023
FOAMed
- Coni R. Neuro 101: Peripheral Nervous System. LITFL
- Nickson C. Myotomes and Differentiating Nerve Lesions. LITFL
Fellowship Notes
MBBS DDU (Emergency) CCPU. Adult/Paediatric Emergency Medicine Advanced Trainee in Melbourne, Australia. Special interests in diagnostic and procedural ultrasound, medical education, and ECG interpretation. Co-creator of the LITFL ECG Library. Twitter: @rob_buttner
Educator, magister, munus exemplar, dicata in agro subitis medicina et discrimine cura | FFS |


