Temporary Epicardial Cardiac Pacing
OVERVIEW
- the usual means of cardiac pacing following cardiac surgery
USES/INDICATIONS
Post cardiac surgery
- conduction abnormality (bradyarrhythmia)
- tachycardia (AV junctional tachycardia, SVT, VT, atrial flutter)
- other: restoration of AV synchrony, HOCM to prevent SAM
Indications are controversial – some centers have at least ventricular leads in almost all cardiac surgery patients, others only in those who have rhythm disturbance intraoperatively
DESCRIPTION
- produce electrical current with subsequent depolarisation + sensing function
Unipolar
- negative wire attached to the epicardium
- positive wire attached to subcutaneous tissues
Bipolar
- a single wire with two conductors insulated from one another which both run to the epicardial surface
- smaller distance for current to run -> threshold less
- more suitable for dual chamber applications
- require less energy to begin with and may have greater longevity compared to unipolar system
METHOD OF INSERTION AND/OR USE
Typical settings
- atrial and ventricular output 10mA
- lower rate 80/min
- atria and ventricular sensitivity 2-5mV
- PR interval 150ms or ‘auto’ (determined by rate)
- PVARP 250ms or ‘auto’ (determined by rate) = post ventricular (pacing spike) atrial refractory period
Daily Checks
- assess underlying rhythm
-> turn pacemaker rate down and assess native rhythm
(do not turn down the output energy – there may be no underlying rhythm!) - determine sensitivity (minimum current that the pacemaker is able to sense)
-> place in VVI, AAI or DDD, increase sensitivity until the sense indicator stops flashing
-> asynchronous pacing should take place, then turn sensitivity down until sense indicator flashes which each endogenous depolarisation
-> this equals the pacing threshold
-> set pacing generator at half the pacing threshold - determine capture threshold (minimum output required to stimulate an action potential in the myocardium)
-> set rate above native rate
-> then reduce output until QRS no longer follows pacing spike = capture threshold
-> leave output at twice the threshold
Removal of wire
- gentle traction allowing cardiac motion to help dislodgement
- if they get cut, cut close to skin so they will retract
OTHER INFORMATION
Duration of use
- Epicardial wires usually fail to sense and capture after a few days
- Increases in stimulation threshold typically occur after 4 days in both atrial and ventricular wires
- failure to pace is observed in > 60% right and > 80% left atrial wires after 5 days
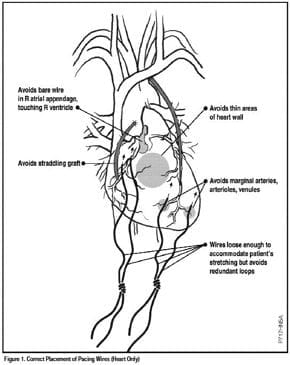
How to extend longevity of pacing wires
- minimise output energy
- optimise wire position (may be at odds with what is optimal for hemodynamics)
- consider steroids (reuces inflammatory reaction to wire)
MRI
- not compatible with MRI due to the amount of ferrous material in pacing box
- controversial regarding in situ epicardial wires
IABP
- if IABP is timed according to ECG with high frequency filter disabled (allowing pacing spikes to become visible) -> pacing spikes can be misinterpreted by the IABP as QRS complexes
- IABP should be timed according the arterial pulse or the high frequency filter applied
- less problematic with bipolar leads
Atrial ECG
- can be performed using atrial wires
- useful for differentiating atrial and junctional arrhythmias, and in defining the nature of an AV block
Safety
- Patients must be nursed in a cardiac-protected electrical environment
- wires should only be handled with non-conductive gloves
- a large metal object (e.g. the bed) should be touched first to discharge static potential prior to touching the wires
- wires should be protected in a non-conductive container e.g. a plastic syringe barrel) when not in use
- continuous ECG monitoring
- immediate access to a cardiac defibrillator with transcutaneous pacing capacity
COMPLICATIONS
Cardiac complications
- infection
- myocardial damage
- perforation
- tamponade
- disruption of coronary anastomoses
- microshock induced arrhythmia (electric shock conducted down epicardial wire)
Pacing complications
- undersensing
- oversensing
- failure to capture
- output failure
- unstable lead position
- pacemaker-mediated tachycardia
References and Links
LITFL
- ECG Library — Pacemaker Rhythms — Normal Patterns
- ECG Library — Pacemaker malfunction
- Medmastery — Pacemaker Essentials: The basics
Journal articles
- Reade MC. Temporary epicardial pacing after cardiac surgery: a practical review: part 1: general considerations in the management of epicardial pacing. Anaesthesia. 2007 Mar;62(3):264-71. PMID: 17300304.
- Reade MC. Temporary epicardial pacing after cardiac surgery: a practical review. Part 2: Selection of epicardial pacing modes and troubleshooting. Anaesthesia. 2007 Apr;62(4):364-73. PMID: 17381573.

Critical Care
Compendium
Chris is an Intensivist and ECMO specialist at The Alfred ICU, where he is Deputy Director (Education). He is a Clinical Adjunct Associate Professor at Monash University, the Lead for the Clinician Educator Incubator programme, and a CICM First Part Examiner.
He is an internationally recognised Clinician Educator with a passion for helping clinicians learn and for improving the clinical performance of individuals and collectives. He was one of the founders of the FOAM movement (Free Open-Access Medical education) has been recognised for his contributions to education with awards from ANZICS, ANZAHPE, and ACEM.
His one great achievement is being the father of three amazing children.
On Bluesky, he is @precordialthump.bsky.social and on the site that Elon has screwed up, he is @precordialthump.
| INTENSIVE | RAGE | Resuscitology | SMACC