Pacemaker Malfunction
Pacemaker Malfunction Overview
- Pacemaker malfunction can occur for a wide variety of reasons, ranging from equipment failure to changes in underlying native rhythm
- Diagnosis of pacemaker malfunction is challenging and often associated with non-specific clinical symptoms while ECG changes can be subtle or absent
Note: Normal pacemaker function is discussed extensively in a seperate post.
Problems with Sensing
Undersensing
- Undersensing occurs when the pacemaker fails to sense native cardiac activity
- Results in asynchronous pacing
- Causes include increased stimulation threshold at electrode site (exit block), poor lead contact, new bundle branch block, or programming problems
- ECG findings may be minimal, although presence of pacing spikes within QRS complexes is suggestive of undersensing
Oversensing
- Oversensing occurs when electrical signal are inappropriately recognised as native cardiac activity and pacing is inhibited
- These inappropriate signals may be large P or T waves, skeletal muscle activity or lead contact problems
- Abnormal signals may not be evident on ECG
- Reduced pacemaker output / output failure may be seen on ECG monitoring if the patient stimulates their rectus or pectoral muscles (due to oversensing of muscle activity)
Problems with Pacing
Output failure
- Output failure occurs when a paced stimulus is not generated in a situation where expected
- Results in decreased or absent pacemaker function
- Multiple causes including oversensing, wire fracture, lead displacement, or interference
Failure to capture
- Failure to capture occurs when paced stimulus does not result in myocardial depolarisation
- Multiple causes including electrode displacement, wire fracture, electrolyte disturbance, MI or exit block
NB. If the patient’s native heart rate is above the pacemaker threshold, no pacemaker activity is expected and therefore output failure and capture failure cannot be recognised on the ECG.
Pacemaker Associated Dysrhythmias
Several types of pacemaker associated dysrhythmias can occur including pacemaker-mediated tachycardia (PMT), sensor-induced tachycardia, runaway pacemaker, pacemaker-mediated Wenckebach AV block and lead dislodgement dysrhythmia.
Pacemaker-mediated tachycardia (PMT)
- Also known as endless-loop tachycardia or pacemaker circus movement tachycardia.
- PMT is a re-entry tachycardia in which the pacemaker forms the antegrade pathway with retrograde conduction occurring via the AV node
- Caused by retrograde p waves being sensed as native atrial activity with subsequent ventricular pacing
- The paced ventricular complex results in further retrograde conduction with retrograde p wave generation thus forming a continuous cycle
- Results in a paced tachycardia with the maximum rate limited by the pacemaker programming
- Can be terminated by slowing AV conduction e.g. adenosine or activation of magnet mode
- Newer pacemakers contain programmed algorithms designed to terminate PMT
- May result in rate related ischaemia in the presences of IHD
Sensor-induced tachycardia
- Modern pacemakers are programmed to allow increased heart rates in response to physiological stimuli such as exercise, tachypnoea, hypercapnia or acidaemia
- Sensors may “misfire” in the presence of distracting stimuli such as vibrations, loud noises, fever, limb movement, hyperventilation or electrocautery (e.g. during surgery)
- This misfiring leads to pacing at an inappropriately fast rate
- The ventricular rate cannot exceed the pacemaker’s upper rate limit (usually 160-180 bpm)
- These will also usually terminate with application of a magnet
Runaway pacemaker
- This potentially life-threatening malfunction of older-generation pacemakers is related to low battery voltage (e.g. overdue pacemaker replacement)
- The pacemaker delivers paroxysms of pacing spikes at 200 bpm, which may provoke ventricular fibrillation
- Paradoxically, there may be failure to capture — causing bradycardia — because the pacing spikes are very low in amplitude (due to the depleted battery voltage) and because at very high rates the ventricle may become refractory to stimulation
- Application of a magnet can be life saving but definitive treatment requires replacement of the pacemaker
- Some great cases of runaway pacemaker are discussed here
Lead displacement dysrhythmia
- A dislodged pacing lead may float around inside the right ventricle, intermittently “tickling” the myocardium and causing ventricular ectopics or runs of VT (in much the same way as the guide wire of a central line!), alternating with failure of capture
- If the paced QRS morphology changes from a LBBB pattern (indicating RV placement) to a RBBB pattern (indicating LV placement), this suggests that the electrode has eroded through the interventricular septum
- A chest x-ray will usually help to confirm the diagnosis
Pacemaker Syndrome
- Caused by improper timing of atrial and ventricular contractions resulting in AV dyssynchrony and loss of atrial “kick”
- Variety of clinical symptoms including fatigue, dizziness, palpations, pre-syncope
- Associated decrease in systolic blood pressure > 20 mmHg during change from native rhythm to paced rhythm
Twiddler’s Syndrome
- Patient manipulation of the pulse generator (accidentally or deliberately)
- The pacemaker rotates on its long axis, resulting in dislodgement of pacing leads
- Can result in diaphragmatic or brachial plexus pacing (e.g. arm twitching) depending on extent of lead migration
ECG in Pacemaker Malfunction
- Normal pacemaker rhythms can result in absent pacing activity, irregular pacing and absence of pacing spikes
- Diagnosis of pacemaker malfunction on the ECG is very difficult and may be impossible depending on the underlying native rhythm
- If pacemaker malfunction is suspected cardiology review is required to facilitate pacemaker interrogation and testing
ECG Examples
Example 1
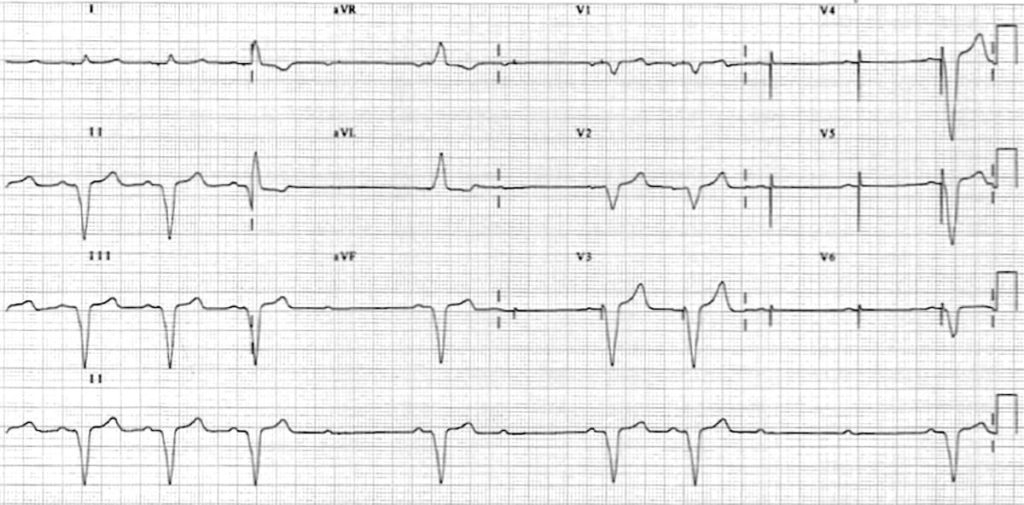
Pacing failure:This ECG shows a ventricular paced rhythm with intermittent failure to capture:
- Atrial sensing appears to be intact — ventricular pacing spikes follow each P wave, most easily seen in V3-6 (tiny pacing spikes are also visible in I, aVR and V1).
- There is presumably an underlying complete heart block or high-grade 2nd degree AV block, as the native P waves do not capture the ventricles.
Example 2
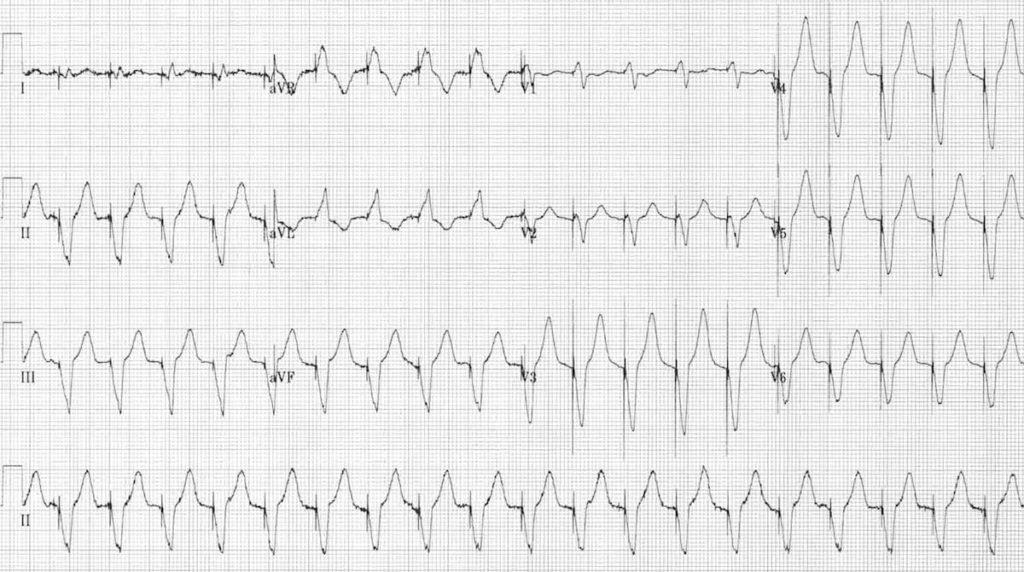
Rapid ventricular pacing
There is a rapid ventricular-paced rhythm (120 bpm) with no evidence of preceding atrial activity (except for the first complex). The differential diagnosis of this rhythm would include:
- Pacemaker-mediated tachycardia (with retrograde P waves buried in the QRS complexes /T waves).
- Sensor-induced tachycardia.
- Could potentially be normal in the presence of an appropriate physiological stimulus (e.g. exercise).
Example 3 – Runaway pacemaker
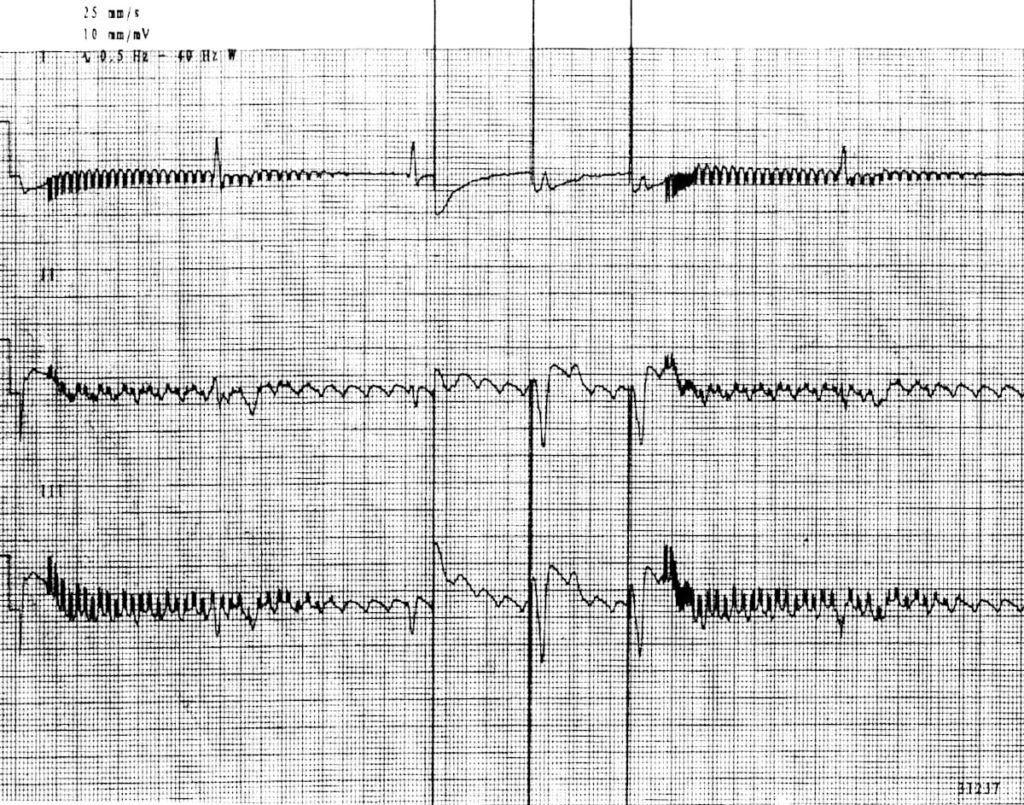
- Paroxysms of rapid pacing spikes at 2000 bpm with decreasing amplitude and rate — this fails to excite the ventricles due to the low amplitude spikes.
- The underlying rhythm is atrial flutter with 3rd degree AV block and ventricular escape rhythm at 30 bpm.
- In the middle, three pacing spikes are seen at 60 ppm in VOO mode: the first is ventricular refractory (failed capture).
This ECG and interpretation is reproduced from Ortega et al. (2005).
Related Topics
References
- Nicholson WJ, Tuohy KA, Tilkemeier P. Twiddler’s Syndrome N Engl J Med 2003; 348:1726-1727.
- Ortega DF, Sammartino MV, Pellegrino GM, Barja LD, Albina G, Segura EV, Balado R, Laiño R, Giniger AG. Runaway pacemaker: a forgotten phenomenon? Europace. 2005 Nov;7(6):592-7. Epub 2005 Sep 8. PubMed PMID: 16216762
Advanced Reading
Online
- Wiesbauer F, Kühn P. ECG Mastery: Yellow Belt online course. Understand ECG basics. Medmastery
- Wiesbauer F, Kühn P. ECG Mastery: Blue Belt online course: Become an ECG expert. Medmastery
- Kühn P, Houghton A. ECG Mastery: Black Belt Workshop. Advanced ECG interpretation. Medmastery
- Rawshani A. Clinical ECG Interpretation ECG Waves
- Smith SW. Dr Smith’s ECG blog.
- Wiesbauer F. Little Black Book of ECG Secrets. Medmastery PDF
Textbooks
- Zimmerman FH. ECG Core Curriculum. 2023
- Mattu A, Berberian J, Brady WJ. Emergency ECGs: Case-Based Review and Interpretations, 2022
- Straus DG, Schocken DD. Marriott’s Practical Electrocardiography 13e, 2021
- Brady WJ, Lipinski MJ et al. Electrocardiogram in Clinical Medicine. 1e, 2020
- Mattu A, Tabas JA, Brady WJ. Electrocardiography in Emergency, Acute, and Critical Care. 2e, 2019
- Hampton J, Adlam D. The ECG Made Practical 7e, 2019
- Kühn P, Lang C, Wiesbauer F. ECG Mastery: The Simplest Way to Learn the ECG. 2015
- Grauer K. ECG Pocket Brain (Expanded) 6e, 2014
- Surawicz B, Knilans T. Chou’s Electrocardiography in Clinical Practice: Adult and Pediatric 6e, 2008
- Chan TC. ECG in Emergency Medicine and Acute Care 1e, 2004
LITFL Further Reading
- ECG Library Basics – Waves, Intervals, Segments and Clinical Interpretation
- ECG A to Z by diagnosis – ECG interpretation in clinical context
- ECG Exigency and Cardiovascular Curveball – ECG Clinical Cases
- 100 ECG Quiz – Self-assessment tool for examination practice
- ECG Reference SITES and BOOKS – the best of the rest
ECG LIBRARY
Emergency Physician in Prehospital and Retrieval Medicine in Sydney, Australia. He has a passion for ECG interpretation and medical education | ECG Library |
MBBS DDU (Emergency) CCPU. Adult/Paediatric Emergency Medicine Advanced Trainee in Melbourne, Australia. Special interests in diagnostic and procedural ultrasound, medical education, and ECG interpretation. Co-creator of the LITFL ECG Library. Twitter: @rob_buttner


I have to say I haven’t read all of this but the content makes me cringe at times Ed, just reading about under/oversensing. Pacing spikes within QRS may mimick undersensing, well that is not quite right. More commonly people are having Carts for heart failure and actually as part of the response to intrinsic activation most companies have algorithms in place to offer some form of biV pacing in response to these for example conducted AF which naturally is a fast conducted rhythm. Secondly it’s like pseudo malfunction as the leads based on position don’t sense until the intrinsic A or V event has started so you might get pseudofusion which is entirely normal.
You say about large P waves being an issue for oversensing which I can only assume you mean for crosstalk right (being sensed in the V). This isn’t really an issue anymore due to effective blanking periods namely PAVB in this case preventing cross talk as the V is functionally blanked during this period. I have to say other content as well such as runaway PPMs don’t really occur unless the device has been significantly damaged by say radiation of high frequency and 2000 bpm… Come on I think at times you’re trying to scare people reading this, I worry that physiologists everywhere will get inundated with queries as people will be reading this on your site.