The Goggle-eyed Fisherman
aka Ophthalmology Befuddler 023
A 38 year-old professional fisherman presents to your emergency department after returning to shore from a 3 week trip. Over the past week he has had progressively worsening left eye symptoms and is now feeling quite unwell.
He has been having fevers, has a constant headache and his left eye has become swollen. He reports a history of double vision but now he has trouble seeing anything out of his left eye. Any movement of the eye causes significant pain.
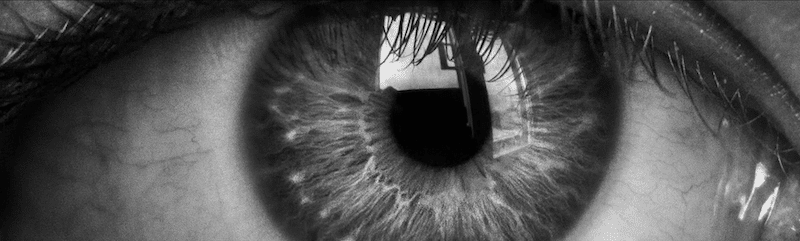
His eye looks like this:

Questions
Q1. What is the likely diagnosis?
Answer and interpretation
Orbital/ post-septal cellulitis
Features present in the image include:
- eyelid edema and erythema
- chemosis and an engorged conjunctiva
- proptosis
Q2. What features should be assessed when taking the history?
Answer and interpretation
History:
- Symptoms — red eye, pain, blurred vision, double vision, eyelid swelling, nasal congestion, sinus headache/ pressure, tooth pain, periorbital pain or hypesthesia.
- Consider possible underlying causes — trauma, surgery, ENT or systemic infection, diabetes mellitus, and immunosuppression
Q3. What features should be looked for on examination?
Answer and interpretation
Examination:
- Visual acuity: may be reduced in severe cases due to optic nerve stretch or compression
- External exam:
eyelids: eyelid edema, erythema, warmth, tenderness
conjunctiva: chemosis and injection
proptosis
other: purulent discharge and decreased periorbital sensation may be present - Extraocular eye movements: restricted ocular motility with pain on attempted eye movement.
- Pupils: RAPD may be present in severe cases due to optic nerve stretch or compression
- Fundoscopy: retinal venous congestion and optic disc edema in severe cases.
- General exam: Fever; and in severe and progressive disease altered mental state and meningism may occur. Look for evidence of an underlying cause or predisposition (see Q2).
Q4. What causative organisms are usually responsible for this condition in the different settings in which it can occur?
Answer and interpretation
- Adults: Staphylococcus species, Streptococcus species, Bacteroides
- Children — Staphylococcus species, Streptococcus species, Haemophilus influenzae (rarely in vaccinated children)
- Post-traumatic: Gram-negative bacteria
- Dental abscess: mixed, aggressive aerobes and anaerobes
- Immunocompromised or diabetes mellitus: consider fungi, e.g. mucormycosis/zygomycosis, aspergillosis.
Q5. What investigations are required when considering this diagnosis?
Answer and interpretation
- Laboratory: FBC, blood cultures, wound swabs, consider the need for lumbar puncture.
- CT scan of the orbits and sinuses: confirms the diagnosis and helps to exclude cavernous sinus thrombosis, orbital or subperiosteal abscesses, paranasal sinus disease and foreign bodies
Q6. What is the appropriate management?
Answer and interpretation
Referral to ophthalmology for admission to hospital. An infectious diseases consult is often appropriate
Consider consultant the following:
- neurology — if suspected CNS infection
- ENT — if drainage of the sinuses is needed
- oral/maxillofacial surgeons — if emergency dental extraction is needed
Based on the Australian Therapeutic Guidelines, at least 3 days of:
- cefotaxime 2 g (child: 50 mg/kg up to 2 g) IV 8-hourly
- or ceftriaxone 2 g (child: 50 mg/kg up to 2 g) IV daily
- AND flucloxacillin 2 g (child: 50 mg/kg up to 2 g) IV, 6-hourly.
Followed by:
- amoxycillin+clavulanate 875+125 mg (child: 22.5+3.2 mg/kg up to 875+125 mg) orally, 12-hourly to complete a total of 14 days antibiotics.
Further anaerobic cover may be required (e.g. metronidazole), for instance, if a dental cause is suspected. If MRSA is suspected consult an infectious disease specialist and consider treatment with vancomycin.
Other treatments may be required:
- analgesia
- Nasal decongestant spray as needed for up to 3 days.
- Erythromycin ointment qid — for corneal exposure and chemosis if there is severe proptosis.
- canthotomy/cantholysis — may be required if the orbit is tight, optic neuropathy is present or the IOP is severely elevated.
- abscess drainage
Your next patient is a small child who is systemically well. He has developed redness and swelling around his right eye over the past few days:

Q7. What is the likely diagnosis?
Answer and interpretation
Periorbital/ pre-septal cellulitis
Q8. What are the clinical features of this condition, and how is it distinguished from the goggle-eyed fisherman’s diagnosis?
Answer and interpretation
Periorbital (or preseptal) cellulitis is a soft-tissue infection of the eyelids that does not extend past the orbital septum posteriorly. It causes eyelid and periorbital edema, redness, and discomfort.
The ocular exam should be essentially normal:
- normal visual acuity
- FROEM without significant discomfort
- absence of proptosis
Sometimes the clinical distinction is unclear and imaging is necessary (e.g. CT orbits and sinuses).
Q9. What organisms cause this condition in children <5 years of age?
Answer and interpretation
Much the same as for orbital cellulitis:
- Staphylococcus aureus
- Streptococcus pneumoniae
- Streptococcus anginosus/milleri group
- Haemophilus influenzae type b (Hib) in the unvaccinated
Q10. What is the antibiotic treatment of this condition?
Answer and interpretation
Systemically well children <5 years of age:
- amoxycillin+clavulanate 22.5+3.2 mg/kg po q12h for 7 days
- OR cephalexin 12.5 mg/kg orally, 6-hourly for 7 days
Older children or adults or children with an infected wound or stye, etc:
- flucloxacillin 500 mg (child: 12.5 mg/kg up to 500 mg) orally, 6-hourly for 7 days – (cephalexin and clindamycin are options in the setting of penicillin hypersensitivity)
If systemically unwell it is best to treat and investigate for orbital cellulitis.
References
- Ehlers JP, Shah CP, Fenton GL, Hoskins EN. The Wills Eye Manual: Office and Emergency Room Diagnosis and Treatment of Eye Disease Lippincott Williams & Wilkins
- NSW Statewide Opthalmology Service. Eye Emergency Manual — An illustrated Guide. [Free PDF]
OPHTHALMOLOGY BEFUDDLER
Chris is an Intensivist and ECMO specialist at The Alfred ICU, where he is Deputy Director (Education). He is a Clinical Adjunct Associate Professor at Monash University, the Lead for the Clinician Educator Incubator programme, and a CICM First Part Examiner.
He is an internationally recognised Clinician Educator with a passion for helping clinicians learn and for improving the clinical performance of individuals and collectives. He was one of the founders of the FOAM movement (Free Open-Access Medical education) has been recognised for his contributions to education with awards from ANZICS, ANZAHPE, and ACEM.
His one great achievement is being the father of three amazing children.
On Bluesky, he is @precordialthump.bsky.social and on the site that Elon has screwed up, he is @precordialthump.
| INTENSIVE | RAGE | Resuscitology | SMACC
