Tissue Oxygenation Assessment
TYPE OF HYPOXIA
- Hypoxaemic – low oxygen tension
- Stagnant – reduced tissue blood flow
- Anaemic – low Hb
- Histiotoxic/cytopathic – abnormal cellular oxygen utilisation
OXYGEN TOXICITY
- cell dysfunction from high oxygen tension
OXYGEN DELIVERY MEASUREMENT
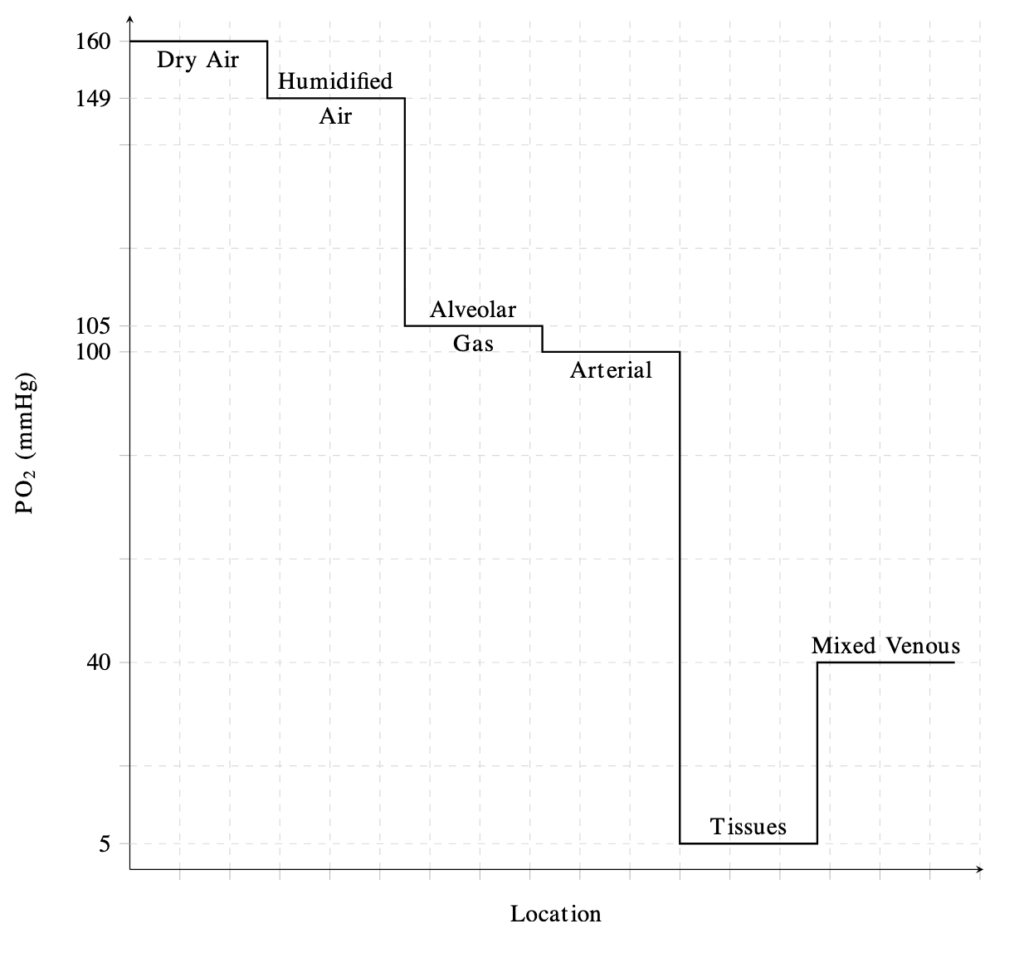
Inspired O2 (PiO2)
- PiO2 = FiO2 x (barometric pressure – saturated vapour pressure of H20)
- PiO2 = 0.21 x (760 – 47) – sea level
- PiO2 = 150mmHg
- gas supply pressures are continuously measured
- FiO2 is monitored within the inspiratory limb of ventilators
- Note that gas supply may vary in extent of humidification, however the inspired gas will be humidified (ideally close to 100%) during passage to the alveoli through the respiratory conduction system
PiO2 to Alveoli
- Open communication between inspired gas supply and the alveoli is indicated by:
- absence of upper airway obstruction
- expired tidal and minute volumes and airway pressures for the ventilated are within correctly set alarms
- an appropriate end-tidal CO2 waveform
Alveolar Gas (PAO2)
- marked variation in PO2 between lung units makes measurement of ETO2 pointless
- clinical assessment chest movement, air entry and CXR
- electrical impedance tomography: non-invasive tracking of lung volume changes
- assessment of V/Q mismatch: Multiple Inert Gas Technique (MIGET) -> impractical, FiO2 to SpO2 is more practical
- The ‘short’ form of the alveolar gas equation is: PAO2 = PiO2 – PaCO2/0.8
- where PiO2 = (Patm – PH2O) x FiO2
- PiO2 is the partial pressure of oxygen inspired by the lung alveoli
- the ‘long form’ is PAO2 = (Patm – PH2O) x FiO2 – PaCO2/RQ+ f
- Patm is atmospheric pressure
- PH20 is the water vapour pressure (47mmHg if 100% humidification at body temperature, 37C)
- FiO2 is the fraction of inspired oxygen
- PaCO2 is the arterial partial pressure of CO2
- RQ is the respiratory quotient (usually 0.8 but can , and vary with diet and metabolic state)
- F is a commonly ignored correction factor of 2-3 mmHg accounting for changes in the partial pressure of nitrogen.
- where PiO2 = (Patm – PH2O) x FiO2
Alveolar Gas to Arterial Blood (PAO2 -> PaO2)
- A-a gradient
- PaO2/FiO2 ratio
- venous admixture (Qs/Qt): use of the shunt equation, requires a PAC
Arterial Blood
- blood gas analysis and co-oximetry
- continuous intra-arterial blood gas monitoring: invasive, not validated yet, accurate
- transcutaneous PO2 and PCO2 monitoring: reliable CO2, not so accurate O2, heat skin -> burns, regular calibration required
- pulse oximetry
- haemoglobin-oxygen affinity: described by the oxy-Hb dissociation curve
OXYGEN CONSUMPTION MEASUREMENT
DO2/VO2 relationships
- oxygen delivery index (DO2I): CI x arterial oxygen content (CaO2) x 10, difficult to interpret because varies greatly in illness
- oxygen consumption index (VO2I): CI x (CaO2-CvO2) x 10 via the reverse Fick method or indirect calorimetry – many random error and inaccuracies
Mixed Venous Blood
- blood aspirated from an unwedged PA
- mixed venous PO2 (PvO2): low value -> intracellular hypoxia, high value -> doesn’t exclude histiotoxic hypoxia or tissue shunting.
- mixed venous oxygen saturation (SvO2): normal = 0.7-0.8, hypoxia + lactate acidosis = 0.3-0.5, > 0.8 = high flow states (sepsis, hyperthyroidism, severe liver disease)
- central venous saturation (SCVO2): normally 3% lower than SvO2, trends and response to management run in parallel.
- venoarterial PCO2 gradient (∆PCO2): normally about 6mmHg, markedly increases in low output states and cardiac arrest, lacks sensitivity and specificity as a global index of tissue hypoxia.
Plasma Lactate and Redox indices
- produced as a result of anaerobic metabolism in the context of inadequate tissue oxygenation.
- lactic acidosis: production exceeds metabolism or metabolism is decreased by organ dysfunction.
- normal = < 1mmol/L
Regional Oxygenation Indices
- regional PCO2: reflects the balance between PaCO2, tissue blood flow and tissue CO2 production, a rising gap between PaCO2 and tissue PCO2 signifies falling tissue blood flow (gastric tonometry and sublingual capnometry)
- cerebrovenous oxygen saturation monitoring: retrograde passing of catheter into jugular bulb to measure venous saturation (goal = 55-85%)
- direct tissue PO2 measurement: animal data, highly impractical
- othrogonal polarisation spectroscopy: microcirculation assessment
- in vivo MRI
- optical spectroscopy

Critical Care
Compendium
Chris is an Intensivist and ECMO specialist at The Alfred ICU, where he is Deputy Director (Education). He is a Clinical Adjunct Associate Professor at Monash University, the Lead for the Clinician Educator Incubator programme, and a CICM First Part Examiner.
He is an internationally recognised Clinician Educator with a passion for helping clinicians learn and for improving the clinical performance of individuals and collectives. He was one of the founders of the FOAM movement (Free Open-Access Medical education) has been recognised for his contributions to education with awards from ANZICS, ANZAHPE, and ACEM.
His one great achievement is being the father of three amazing children.
On Bluesky, he is @precordialthump.bsky.social and on the site that Elon has screwed up, he is @precordialthump.
| INTENSIVE | RAGE | Resuscitology | SMACC
