Trauma! Extremity Arterial Hemorrhage
aka Trauma Tribulation 030
A 24 year old man has been stabbed in the right upper limb with a large kitchen knife. The ambulance officers have just brought him into the emergency department. They report that there was a large amount of blood at the scene. They describe brisk pulsatile bleeding from a wound proximal to the man’s right elbow and have treated it with a compression bandage, that appears to be soaked through with blood dripping onto the floor…
Looks like your dinner break is going to have to wait!
Questions
Q1. How would you recognize severe arterial hemorrhage from extremity trauma?
Answer and interpretation
Recognition
- Penetrating extremity injury (e.g. stab or gunshot) or severe blunt trauma (e.g. arterial injury due to associated fracture)
- Cold, pale and pulseless distal extremity or a rapidly expanding hematoma suggests arterial compromise — look for ‘hard signs’ (Q7 below) and ‘soft signs’ (Q8 below)
- Check arterial pressure index (API) (Q9 below).
- Assess for hemorrhagic shock
- Angiography can be performed only if the patient is hemodynamically stable
Q2. How would you manage severe arterial hemorrhage from extremity trauma?
Answer and interpretation
Management
- Immediate surgical consult
- Apply direct pressure and elevation
- Consider applying adrenaline soaked gauze or hemostatic dressings if available
- Tourniquets may be life saving
- Reduce and splint long bone fractures, apply a pelvic binder for pelvic fractures
- Correct coagulopathy and commence hemostatic resuscitation as required
- Do not clamp or tie off a vessel in a bleeding wound, unless it is superficial and clearly visible. Blindly clamping an artery may damage a nerve that often runs alongside the artery.
Learn more: Broome Docs — Clinical Case 018: Life and limb (not life OR limb)
Q3. What is the best way to apply direct pressure when there is arterial bleeding?
Answer and interpretation
Direct digital pressure is the best method initially
- Take universal precautions (wear sterile gloves, goggles and gown)
- Ensure there are no hazardous objects in the wound
- Use one finger, with interposed gauze, to press directly on the bleeding vessel just proximal to the bleeding point
- Maintain this for 10 minutes
Q4. What is the best way to apply a pressure bandage over a bleeding point?
Answer and interpretation
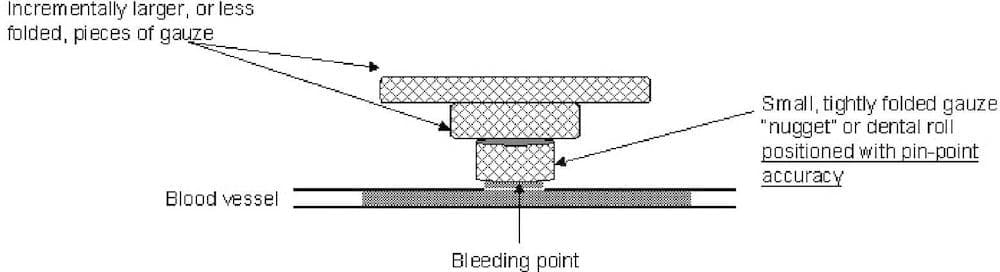
I like the ‘nugget method‘ described by Shokrollahi et al (2008) as follows:
- The occluding finger should be substituted with a dental roll or tightly folded “nugget” of gauze.A tourniquet may be temporarily applied proximally to facilitate this.
- Once the positioning is correct and no further bleeding is occurring, slightly larger or less folded pieces of gauze can be placed one on top of the other, creating an inverted pyramid of gauze.
- The layers of gauze are secured with a loose bandage. Only very light pressure need be applied to the top layer of gauze to maintain hemostasis, as the pressure is “focused” onto the bleeding point. This technique is based on the equation: Pressure=Force/Area
- The tightness of the bandage can be judged from the amount of pressure needed to maintain hemostasis when applying the top layer of gauze.
Q5. How is a tourniquet applied in the presence of an uncontrolled arterial bleeder?
Answer and interpretation
The easiest way in the ED is to apply a blood pressure cuff proximal to the bleeding point.
- Inflate the cuff above systolic blood pressure
- Clamp the tubing with a hemostat to prevent leakage and loss of pressure
An alternative is to use a pneumatic cuff, like that used for Bier’s blocks.
When applying a tourniquet ensure the following:
- Record the time of application
- Perform a neurological exam at the time of application
- Do not leave the tourniquet on for more than 120 minutes
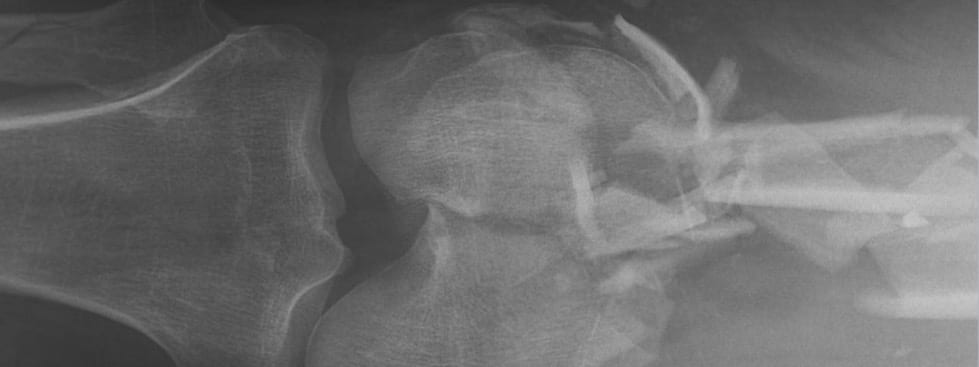
Q6. What are the two transition points where proximal control of a peripheral vascular injury becomes exceedingly difficult?
Answer and interpretation
These are the two transition points
- Femoral artery at the inguinal ligament
- Axillary artery as it emerges from under the clavicle
Bleeding points proximal to these sites cannot be controlled by externally applied direct pressure or tourniquets. Call a surgeon!
Q7. What are the hard signs of vascular injury?
Answer and interpretation
Hard signs
- Absent pulses
- Bruit or thrill
- Active or pulsatile hemorrhage
- Signs of limb ischemia/ compartment syndrome (the 6 Ps)
- Pulsatile or expanding hematoma
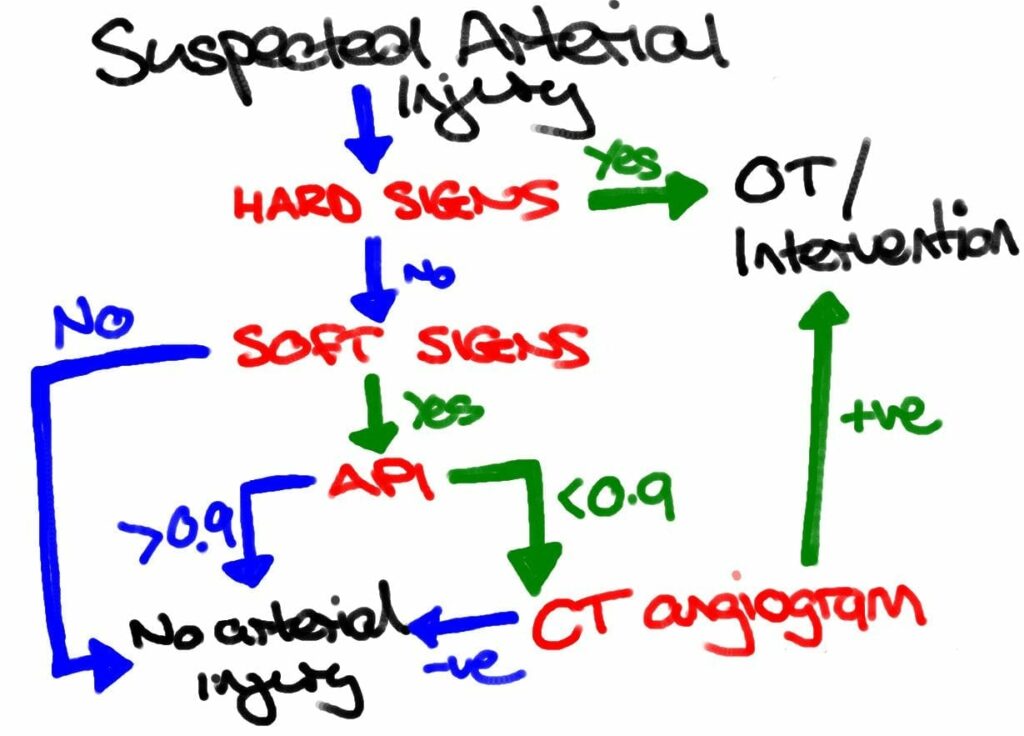
These patients require operative intervention. Imaging is not needed unless the site of bleeding is uncertain.
Q8. What are the soft signs of vascular injury?
Answer and interpretation
Soft signs
- Proximity of injury to vascular structures
- Major single nerve deficit (e.g. sciatic, femoral, median, ulna or radial)
- Non-expanding hematoma
- Reduced pulses
- Posterior knee or anterior elbow dislocation
- Hypotension or moderate blood loss at the scene
Patients with soft signs may or may not need imaging, depending on the API (arterial pressure index)
- those with an otherwise normal physical exam and API >0.9 can be observed following appropriate wound care.
- API < 0.9 indicates possible vascular injury: requires further evaluation, preferably by computed tomography angiogram (CTA)
The incidence of arterial injuries in such patients ranges from 3% to 25%, depending on which soft sign or combination of soft signs is present.
Q9. How is an arterial pressure index (API) performed and calculated? What does it mean?
Answer and interpretation
Arterial pressure index (API) is also known as DPI (Doppler Pressure Index) or Arterial Brachial Index or Ankle Brachial Index (ABI) – despite the last name, the same procedure can be performed for upper extremity injuries.
The procedure is performed as follows for an injured upper extremity:
- The patient is placed supine with the cuff placed on the injured upper extremity
- The ipsilateral brachial artery is detected with a Doppler device until the brachial artery is clearly heard. Alternatively the cuff can be placed on the forearm and the ulnar or radial arteries are assessed (the cuff has to be distal to the injury!).
- The cuff is pumped up 20 mmHg past the point where the Doppler sound disappears. The cuff is slowly released until the Doppler device picks up the arterial sound again (the systolic pressure)
- The pressure at which this sound occurs is recorded and the procedure is repeated for the opposite uninjured upper extremity.
IT can also be performed for an injured lower extremity:
- The patient is placed supine with the cuff placed on the injured lower extremity.
- The ipsilateral dorsalis pedis or posterior tibial artery is detected with a Doppler device until the artery is clearly heard
- The cuff is pumped up 20 mmHg past the point where the Doppler sound disappears. The cuff is slowly released until the Doppler device picks up the arterial sound again (the systolic pressure)
- The pressure at which this sound occurs is recorded and the procedure is repeated for the opposite uninjured lower extremity
- The blood pressure is also measured at the brachial artery in an uninjured upper extremity.
The API is calculated as
API = the systolic pressure of the injured extremity (ankle or forearm) divided by the brachial systolic pressure in the uninjured upper extremity
i.e.
API = Injured SBP / Uninjured brachial SBP
The magic number is 0.9
- API > 0.9 is highly unlikely to have a vascular injury and may be observed/ discharged depending on the nature of any other injuries, premorbid and social factors.
- API < 0.9 indicates possible vascular injury: requires further evaluation, preferably by computed tomography angiogram (CTA). Doppler ultrasound (50-100% sensitive, 95% specific) can be used as an alternative, and surgeons can perform intraoperative angiograms under fluoroscopy.
How good is API?
The performance characteristics of API vary between studies, but is quoted as 95% sensitive and 97% specific for arterial injury by Lynch and Johannsen (1991). In a small prospective study of knee dislocations ABI was 100% sensitive and specific (Mills et al, 2004). It is also cost effective (Levy et al, 2005).
API will miss non-obstructing vascular injuries and will give false positive results in patients with shock or significant peripheral vascular disease. Some trauma centers use a difference in API of >=0.1 as an indication of arterial injury in elderly patients and those with known pre-existing peripheral vascular disease.
Below is a simplified approach to suspected arterial injury in trauma. Stabilise the patient first, and ensure that any fractures or dislocations are reduced.
The WEST guidelines (Feliciano et al, 2011) are much more complex and detail a number of exceptions. For instance, CTA may be performed in the presence of hard signs if there is a shot gun injury or multiple fractures to help localise the vascular injury before operating.
Interventions are discussed in Q10 below.
Patients discharged following a normal API require close outpatient follow up. This is because 1-4% of these patients, primarily those with penetrating wounds, eventually require an operation as the original undetected injury (i.e. small pseudoaneurysm) progresses rather than heals.
Q10. What are the surgical options for repair of vascular injuries?
Answer and interpretation
Injuries to most major ‘named’ arteries requiring repair or intervention include:
- extravasation
- pulsatile hematoma
- occlusion
- pseudoaneurysm
- fistula formation
The surgeon may repair damaged vessels by:
- Direct repair — sutures, patch angioplasty, interposition graft or vein patches
- Ligation — only small, distal and redundant arteries (most are repaired)
- Damage control surgery using intravascular shunts to allow immediate restoration of distal blood flow, with later definitive repair once the patient has been resuscitated and normal physiology has resumed.
Interventional radiology measures such as embolisation are also useful in certain arterial injuries.
Injuries that do not usually need immediate intervention:
- Some injuries, such as intimal defects (87-95% heal spontaneously), usually do not require intervention.
- Some arteries (profunda femoris, anterior tibial, posterior tibial, or peroneal arteries) do not require surgery but can be re-imaged at 3-5 days to check progress if occluded, or undergo embolisation if the injury involves extravasation or arteriovenous fistula.
References
FOAM
- Trauma! Extremity Injuries
- Trauma! Major Haemorrhage
- Trauma! Massive Transfusion
- Broome Docs — Clinical Case 018: Life and limb (not life OR limb)
- ScanCrit — The Mother of All Tourniquets (abdominal aorta tourniquet!)
- The Trauma Professional’s Blog — Using CT To Diagnose Extremity Vascular Injury
- The Trauma Professional’s Blog — Penetrating Injuries to the Extremities
Publications
- Conrad MF, Patton JH Jr, Parikshak M, Kralovich KA. Evaluation of vascular injury in penetrating extremity trauma: angiographers stay home. Am Surg. 2002 Mar;68(3):269-74. PubMed PMID: 11893106.
- Feliciano DV, Moore FA, Moore EE, West MA, Davis JW, Cocanour CS, Kozar RA, McIntyre RC Jr. Evaluation and management of peripheral vascular injury. Part 1. Western Trauma Association/critical decisions in trauma. J Trauma. 2011 Jun;70(6):1551-6. PubMed PMID: 21817992.
- Fildes J, et al. Advanced Trauma Life Support Student Course Manual (8th edition), American College of Surgeons 2008.
- Inaba K, Potzman J, Munera F, McKenney M, Munoz R, Rivas L, Dunham M, DuBose J. Multi-slice CT angiography for arterial evaluation in the injured lower extremity. J Trauma. 2006 Mar;60(3):502-6; discussion 506-7. PubMed PMID: 16531846.
- Inaba K, Branco BC, Reddy S, Park JJ, Green D, Plurad D, Talving P, Lam L, Demetriades D. Prospective evaluation of multidetector computed tomography for extremity vascular trauma. J Trauma. 2011 Apr;70(4):808-15. PubMed PMID: 21610388.
- Kragh JF Jr, Walters TJ, Baer DG, Fox CJ, Wade CE, Salinas J, Holcomb JB. Practical use of emergency tourniquets to stop bleeding in major limb trauma. J Trauma. 2008 Feb;64(2 Suppl):S38-49; discussion S49-50. PubMed PMID: 18376170.
- Legome E, Shockley LW. Trauma: A Comprehensive Emergency Medicine Approach, Cambridge University Press, 2011.
- Levy BA, Zlowodzki MP, Graves M, Cole PA. Screening for extremity arterial injury with the arterial pressure index. Am J Emerg Med. 2005 Sep;23(5):689-95. Review. PubMed PMID: 16140180.
- Lynch K, Johansen K. Can Doppler pressure measurement replace “exclusion” arteriography in the diagnosis of occult extremity arterial trauma? Ann Surg. 1991 Dec;214(6):737-41. PubMed PMID: 1741655; PubMed Central PMCID: PMC1358501.
- Lundin M, Wiksten JP, Peräkylä T, Lindfors O, Savolainen H, Skyttä J, Lepäntalo M. Distal pulse palpation: is it reliable? World J Surg. 1999 Mar;23(3):252-5. PubMed PMID: 9933695.
- Marx JA, Hockberger R, Walls RM. Rosen’s Emergency Medicine: Concepts and Clinical Practice (7th edition), Mosby 2009. [mdconsult.com]
- Mills WJ, Barei DP, McNair P. The value of the ankle-brachial index for diagnosing arterial injury after knee dislocation: a prospective study. J Trauma. 2004 Jun;56(6):1261-5. PubMed PMID: 15211135.
- Shokrollahi K, Sharma H, Gakhar H. A technique for temporary control of hemorrhage. J Emerg Med. 2008 Apr;34(3):319-20. Epub 2007 Dec 27. PubMed PMID: 18164163.
- Newton EJ, Love J. Acute complications of extremity trauma. Emerg Med Clin North Am. 2007 Aug;25(3):751-61, iv. PMID: 17826216.
CLINICAL CASES
Trauma Tribulation
Chris is an Intensivist and ECMO specialist at The Alfred ICU, where he is Deputy Director (Education). He is a Clinical Adjunct Associate Professor at Monash University, the Lead for the Clinician Educator Incubator programme, and a CICM First Part Examiner.
He is an internationally recognised Clinician Educator with a passion for helping clinicians learn and for improving the clinical performance of individuals and collectives. He was one of the founders of the FOAM movement (Free Open-Access Medical education) has been recognised for his contributions to education with awards from ANZICS, ANZAHPE, and ACEM.
His one great achievement is being the father of three amazing children.
On Bluesky, he is @precordialthump.bsky.social and on the site that Elon has screwed up, he is @precordialthump.
| INTENSIVE | RAGE | Resuscitology | SMACC