Trauma! Massive Transfusion
aka Trauma Tribulation 026
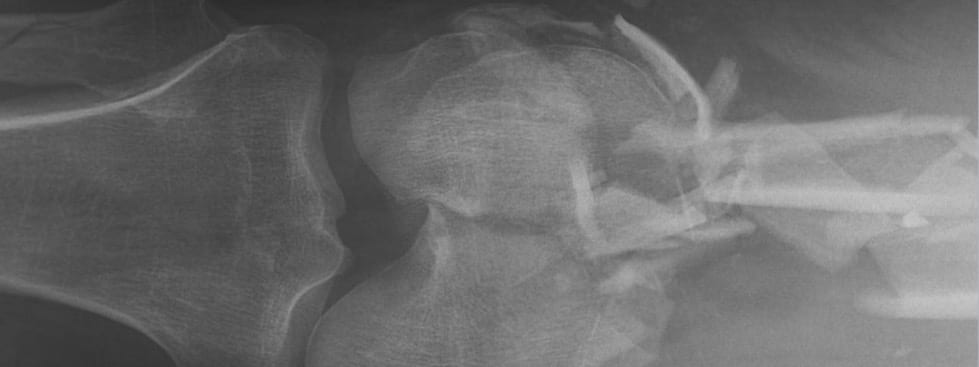
The unfortunate scaffolder from Trauma Tribulation 025 is still in extremis, he is bleeding from multiple sites and is in hemorrhagic shock. The trauma team is hard at work and the operating theatre staff are preparing for his arrival. He is being actively resuscitated…
A lot has changed in recent years, with the rise of damage control resuscitation and the development of massive transfusion protocols. If you’re the Trauma Team Leader (and, in this case, you are!) you’d better know all the ins and outs.
Questions
Q1. When should a massive transfusion protocol be triggered?
Answer and interpretation
The simplest trigger is when a senior clinician suspects impending or actual hemorrhagic shock in bleeding patient.
Various scoring systems have been developed to predict the need for massive transfusion, such as the ABC score, the TASH score and the McLaughlin score
There is also research that methods such as thromboelastometry can give an early warning of acute coagulopathy of trauma/ shock (ACoTS).
Assessment of Blood Consumption (ABC) score
- ED SBP <90mmHg(0=no; 1=yes)
- ED HR >120bpm
- Penetrating mechanism
- Positive fluid on FAST exam
Score of 3 predicts 45% need for massive transfusion; score of 4 predicts 100% need for massive transfusion
Trauma-Associated Severe Hemorrhage
- SBP
- Gender
- Hb
- Fluid on ultrasound
- HR
- Base excess
- Extremity or pelvic fracture
McLaughlin score
- HR > 105/min
- SBP < 110 mmHg
- pH < 7.25
- Hct < 32%
Q2. What is the definition of massive transfusion?
Answer and interpretation
Definitions vary… They include:
- 10 unit transfusion in 24 h
- transfusion of an entire blood volume in 24 h
- replacement of 50% blood volume over 3 h
Up to 5% of civilian trauma patients require massive transfusion, and of these 25% have trauma-associated coagulopathy on assessment in ED.
Q3. What ‘essential’ history is required when activating the massive transfusion protocol?
Answer and interpretation
- Age, gender, mechanism of injury
- Blood components given pre-hospital
- FFP and platelets are likely to be needed earlier if the patient has been transfused pre-hospital
- Known bleeding diathesis
- Bleeding disorders and coagulopathies
- Drugs, e.g. warfarin, aspirin and clopidogrel
- History of previous transfusions, antibodies, reactions if known
Q4. What is the general guide to blood component therapy until major haemorrhage is controlled?
Answer and interpretation
Administer a 1:1:1 ratio of red cells, FFP and platelets
This ratio of blood products emulates the composition of whole blood. The target is to achieve 1:1:1 ratio over 6 hours.
The protocol I’m most familiar with involves:
- Activation of massive transfusion protocol (includes alerting the hematologist on call and laboratory staff)
- Send blood tests: cross match, coags, FBC, blood gas (including iCa)
- Give initial major hemorrhage pack (4 units PRBCS and 2 units thawed FFP)
- In the presence of ongoing uncontrolled haemorrhage give alternating packs A and B, with repeat blood tests after each pack:
— Pack A: 2 units PRBC, 2 units FFP, 1 adult bag of platelets
— Pack B: 2 units PRBC, 2 units FFP
Note that 1 adult bag of platelets is equivalent to 4 units PRBCs for the purposes of maintaining the 1:1 ratio.
Note that the 1:1:1 concept is mainly supported by the fact that it makes sense pathophysiologically and by retrospective and observational studies. It has not been conclusively proven in the way that a large double-blind randomised controlled trial would. Indeed, there are concerns that at least some of the perceived benefit of hemostatic resuscitation and the ‘1:1:1’ ratio is due to survivor bias. Cliff Reid states this eloquently:
“In some circles, ‘wuntwuntwun’ is in danger of becoming the new dogma of trauma fluid replacement (ie. 1 unit of plasma and 1 unit of platelets for every unit of red cells). Since it takes longer to thaw some plasma than it does to throw in some O negative packed red cells, some really sick patients may be dead before they get the plasma, biasing comparisons that show a reduced mortality in patients who were still alive to receive plasma. This ‘survivor bias’ has been suggested as a reason that high plasma:red cell ratios are associated with mortality reduction, although this has been challenged.”
Learn more:
- Broome Docs — Managing Traumatic bleeding: how can we apply the evidence in smaller hospitals?
- EMCrit Lecture: Haemostatic Resuscitation by Richard Dutton
- EMCrit Podcast 30 – Haemorrhagic Shock Resuscitation
- Resus.ME — Battlefield Resuscitation
- Resus.Me — Plasma: Red cell ratios (survivor bias)
Q5. What is the role of tranexamic acid in patients with major trauma?
Answer and interpretation
Current Australian guidelines advise that tranexamic acid should be considered in trauma patients with, or at risk of, significant haemorrhage.
Tranexamic acid an antifibrinolytic that works by competitively inhibiting the activation of plasminogen to plasmin plasmin is responsible for the degradation of fibrin. Given that tranexamic acid is cheap, one of the few interventions with proven mortality benefit (NNT = 67) and few adverse effects I think clinicians should strongly consider this using this agent in major trauma patients.
Tranexamic acid is given as 1g IV loading dose followed by 1g over 8 hours. It should be given with 3 hours of major trauma.
Tranexamic acid should be given early, within 3 hours of the time of injury.
Learn more:
- EMCrit Podcast 67 – Tranexamic Acid (TXA), Crash 2, & Pragmatism with Tim Coats
- Emergency Medicine Literature of Note — Critique of Crash-2
- Emergency Medicine Ireland — Crash-2
- ICU Rounds Podcast — EARLY use of Tranexamic Acid may improve survival from bleeding in trauma
- Resus.ME — How about pre-hospital tranexamic acid?
- Resus.ME — Tranexamic acid saves lives in trauma
- The Lancet — Crash-2: Tranexamic Acid and Trauma Patients (includes link to fulltext pdf)
- The NNT — Tranexamic acid for Trauma
Q6. What specific blood component interventions may be initiated, and what should trigger their administration?
Answer and interpretation
Again, based on the protocol with which I am most familiar:
Platelets
- Give platelets 1 adult dose if platelets <50 x 10E9/L
FFP
- Give FFP 4 units if INR > 1.5 or APTT >50
Cryoprecipitate
- Give cryoprecipitate 8 units if fibrinogen <1.o g/L
Calcium
- Give 10% calcium chloride 10 mL if ionized calcium <1.1 mmol/L
The main difference in the Australian National Blood Authority guidelines is that FFP 15 mL/kg is recommended rather than 4 units.
Q7. What is the role of recombinant factor VIIa?
Answer and interpretation
Recombinant Factor VIIa may be considered for use in consultation with a hematologist if there is:
- Uncontrolled haemorrhage
- That is not amenable to surgical or interventional radiological therapies
- In a salvageable patient with
— optimal blood component therapy (INR, APTT, platelets and fibrinogen all in the normal range),
— pH 7.2, and
— normothermia (T>34C)
Factor VIIa is dosed at 100 mcg/kg to the nearest vial. Further blood component therapy can be given according to serial blood test results.
Remember that Factor VIIa is very expensive and has not been proven to affect clinically meaningful outcomes in the setting of major haemorrhage.
References
Journal Articles and Textbooks
- Cap AP, Baer DG, Orman JA, Aden J, Ryan K, Blackbourne LH. Tranexamic acid for trauma patients: a critical review of the literature. J Trauma. 2011 Jul;71(1 Suppl):S9-14. Review. PubMed PMID: 21795884.
- Crash-2 trial collaborators. Effects of tranexamic acid on death, vascular occlusive events, and blood transfusion in trauma patients with significant haemorrhage (CRASH-2): a randomised, placebo-controlled trial.Lancet. 2010 Jul 3;376(9734):23-32. Pubmed PMID: 20554319 [fulltext]
- CRASH-2 collaborators, Roberts I, Shakur H, Afolabi A, Brohi K, Coats T, Dewan Y, Gando S, Guyatt G, Hunt BJ, Morales C, Perel P, Prieto-Merino D, Woolley T. The importance of early treatment with tranexamic acid in bleeding trauma patients: an exploratory analysis of the CRASH-2 randomised controlled trial. Lancet. 2011 Mar 26;377(9771):1096-101, 1101.e1-2. PubMed PMID: 21439633.
- Fildes J, et al. Advanced Trauma Life Support Student Course Manual (8th edition), American College of Surgeons 2008.
- Legome E, Shockley LW. Trauma: A Comprehensive Emergency Medicine Approach, Cambridge University Press, 2011.
- Marx JA, Hockberger R, Walls RM. Rosen’s Emergency Medicine: Concepts and Clinical Practice (7th edition), Mosby 2009. [mdconsult.com]
- McLaughlin DF, Niles SE, Salinas J, Perkins JG, Cox ED, Wade CE, Holcomb JB. A predictive model for massive transfusion in combat casualty patients. J Trauma. 2008 Feb;64(2 Suppl):S57-63; discussion S63. PubMed PMID: 18376173.
- Nunez TC, Voskresensky IV, Dossett LA, Shinall R, Dutton WD, Cotton BA. Early prediction of massive transfusion in trauma: simple as ABC (assessment of blood consumption)? J Trauma. 2009 Feb;66(2):346-52. PubMed PMID: 19204506.
- Yücel N, Lefering R, Maegele M, Vorweg M, Tjardes T, Ruchholtz S, Neugebauer EA, Wappler F, Bouillon B, Rixen D; Polytrauma Study Group of the German Trauma Society. Trauma Associated Severe Hemorrhage (TASH)-Score: probability of mass transfusion as surrogate for life threatening hemorrhage after multiple trauma. J Trauma. 2006 Jun;60(6):1228-36; discussion 1236-7. PubMed PMID: 16766965.
Social Media and Web Resources
- LITFL Hematology Hoodwinker 002 – Recombinant Factor VIIa to the rescue!?
- LITFL Hematology Hoodwinker 003 – Managing the Critical Bleeder!!
- EMCrit Podcast 71 – Critical Questions on Massive Transfusion Protocols with Kenji Inaba
- Resus.ME — European Trauma Bleeding Guidelines updated
- Traumacast — The CONTROL trial: Factor VIIa in Trauma – Podcast #4
- Traumacast — Trauma Exsanguination Protocols in Trauma – Podcast #5
- Traumacast — Thromboelastography (TEG) in Trauma Care – Podcast #6
CLINICAL CASES
Trauma Tribulation
Chris is an Intensivist and ECMO specialist at The Alfred ICU, where he is Deputy Director (Education). He is a Clinical Adjunct Associate Professor at Monash University, the Lead for the Clinician Educator Incubator programme, and a CICM First Part Examiner.
He is an internationally recognised Clinician Educator with a passion for helping clinicians learn and for improving the clinical performance of individuals and collectives. He was one of the founders of the FOAM movement (Free Open-Access Medical education) has been recognised for his contributions to education with awards from ANZICS, ANZAHPE, and ACEM.
His one great achievement is being the father of three amazing children.
On Bluesky, he is @precordialthump.bsky.social and on the site that Elon has screwed up, he is @precordialthump.
| INTENSIVE | RAGE | Resuscitology | SMACC
