Trauma! Major Haemorrhage
aka Trauma Tribulation 025
A scaffolder was driving home in his van when he had a ‘head-on’ collision with a BMW that crossed the center line. The van was jam-packed with loosely bound scaffolding equipment and the impact sent it rolling into into a ditch. The paramedics are bringing him into the resus room and the trauma team is at the ready. You see that the patient is unresponsive with a vacant stare, he has a grey complexion, and is covered in blood. The word exsanguination springs to mind…
Managing major bleeding should be core business for a Trauma junkie like you, so let’s quickly put these Q&As to rest.
Questions
Q1. What are your main objectives in managing major hemorrhage resulting from trauma?
Answer and interpretation
We have 3 main goals:
- Stop bleeding
- Rapid and effective restoration of blood volume
- Maintain functional blood composition to preserve blood function:
— hemostasis, oxygen carrying capacity, oncotic pressure and biochemistry
Critical bleeding is major haemorrhage that is life threatening and may require massive transfusion.
Q2. What are the likely sources of major hemorrhage?
Answer and interpretation
When assessing the major trauma patient, remember the mantra:
“FIND the bleeding, STOP the bleeding”
It is convenient to consider injuries to 6 regions which may account for major blood loss. Think SCALPeR when finding the bleeding:
- ‘Street’: scalp and external sources (especially small children)
- Chest
- Abdomen
- Long bones (especially femurs)
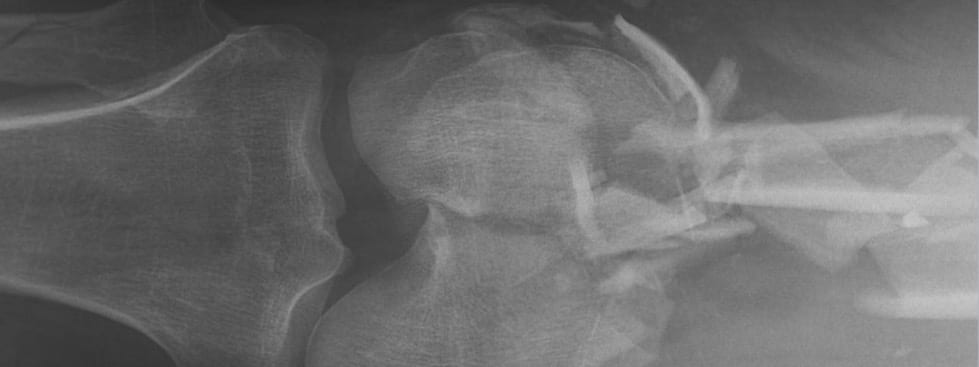
- Pelvis
- Retroperitoneum
Don’t search satisfice and settle for one site of bleeding… be thorough and systematic.
The patient has multiple penetrating wounds and is bleeding profusely from his head. His left thigh is clearly swollen and his pelvis is mushed. An EFAST scan is in progress.
Q3. Describe your overall approach to stopping bleeding?
Answer and interpretation
Yet another handy tip:
Whenever you think ‘control hemorrhage’, think ‘correct coagulopathy’
Approach to hemorrhage control:
- Find the cause
- Initial measures, such as:
— Direct pressure and elevation,
— Adrenaline soaked gauze, hemostatic dressings
— Reduce and splint long bone and pelvic fractures
— Tourniquets - Invasive measures, such as:
— sutures
— tamponade, by packing or foley catheter with balloon inflated
— tie off vessels
— cautery
— interventional radiology
— damage control surgery - Correct coagulopathy
Learn more:
- Resus.ME — Simple emergency haemorrhage control (foley catheter technique for neck wounds)
The patient has cool peripheries and weak radial pulses. His systolic blood pressure is difficult to measure, but is probably about 70 mmHg.
Q4. How useful is pulse palpation as a guide to blood pressure?
Answer and interpretation
Traditional ATLS teaching held that:
- If only the carotid pulse is palpable, the systolic blood pressure (SBP) is 60-70 mmHg
- If the carotid and femoral pulses are palpable, the SBP is 70-80 mmHg
- If the radial pulse is also palpable, the SBP is >80 mmHg
In reality, the pulses are lost in that order (radial, then femoral, then carotid) but the SBP at which they disappear varies and is often lower than what ATLS advises. Thus the ATLS guide will tend to overestimate blood pressure.
Remember that perfusion is more important than blood pressure anyway!
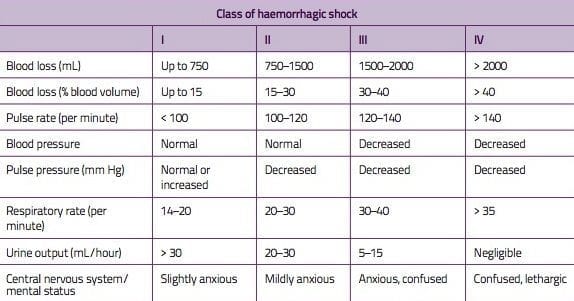
Q5. What are the classic stages of hemorrhagic shock?
Q6. Are the classic stages of hemorrhagic shock useful in clinical practice? Why or why not?
Answer and interpretation
Unfortunately, patients in the real world don’t tend to read ATLS manuals… or if they do they often choose to ignore them!
The classic stages of hemorrhagic shock (a la ATLS) don’t bear out in reality
The reasons for this include:
- Differences in compensation for different types of injuries (e.g. blunt versus penetrating trauma)
- Age (e.g. blunted physiological responses in the elderly)
- Comorbidities
- Medications (e.g. beta-blockade may conceal shock by preventing tachycardia)
Also, bradycardia is often seen in major haemorrhage:
- One theory is that there are 2 phases of response to bleeding:
— inital catacholamine surge with tachycardia, followed by
— subsequent bradycardia of uncertain mechanism (parasympathetically mediated?) - But there also seems to be a group of patients who have relative bradycardia — they fail to mount the initial tachycardia. Some have also noted that bradycardia is more common in acute rapid blood loss (Thomas and Dixon, 2004).
- Some have explained the bradycardia as being due to vagal stimulation from peritoneal stimulation in intra-abdominal hemorrhage, but bradycardia has been seen in penetrating extremity trauma too (Thompson et al, 1990).
Learn more:
- Resus.ME — Evidence refutes ATLS shock classification
No doubt about it, this chap is in haemorrhagic shock. You recognise that you need to deal with ‘the lethal triad’ STAT.
Q7. What is the lethal triad?
Answer and interpretation
The lethal triad is:
- Hypothermia
- Coagulopathy
- Acidosis
These three factors both cause, and contribute to, acute coagulopathy of trauma/ shock (ACoTS) which leads to, and result from, major hemorrhage. They feed off one another, such that bleeding begets more bleeding. This is the theoretical rationale for damage control resuscitation (see below).

The patient’s temperature is 35.9C. Could be worse… but could definitely be better. You decide to do something about it.
Q8. What measures can be used to prevent and treat hypothermia?
Answer and interpretation
Prevent and treat hypothermia with the following:
- Aggressive resuscitation with blood products
- Use warmed fluids (e.g. Level 1 Fluid Warmer)
- Bair Hugger or warm blankets
- Minimise exposure
- Increase ambient temperature
- Continuous temperature monitoring
The patient is being aggressively resuscitated. Crystalloids anyone?
Q9. What is damage control resuscitation?
Answer and interpretation
Damage control resuscitation has 3 components:
- permissive hypotension (aka minimal normotension)
- early hemostatic resuscitation
- damage control surgery
The underlying principles are to limit ongoing haemorrhage, identify and correct coagulopathy and restrict the use of crystalloids.
Permissive hypotension
- Permissive hypotension, or minimal normotension, seeks to avoid excessive fluid administration (and the associated problems of hemodilution, fluid overload and clot disruption). Classically a target SBP of 80 to 100 mmHg is advised.
- As perfusion is more important than blood pressure, an alternate strategy (a la EMCrit) is to target a MAP >65 mmHg together with a good radial pulse and pulse oximetry waveform. If the BP is too high, use titrated aliquots of fentanyl (e.g. 25 micrograms IV) to provide sympatholysis as well as analgesia.
Damage control surgery
Damage control surgery refers to limited surgical interventions that serve to control haemorrhage and minimize contamination until the patient has sufficient physiological reserve to undergo definitive interventions. The strategy aims to bring the ‘lethal triad’ under control, so that the patient will be able to tolerate further surgery once he or she improves.
Hemostatic resuscitation and massive transfusion protocols are discussed in the Trauma Tribulation 026 — Trauma! Massive Transfusion.
Learn more:
Q10. What are the potential downsides of traditional ‘crystalloid first’ resuscitation of trauma patients?
Answer and interpretation
Traditional ATLS teaching is to initiate fluid resuscitation with 1-2 L of crystalloid such as normal saline or compound sodium lactate (Hartmann’s solution).
Potential downsides of this approach include:
- dilutional coagulopathy
- impaired oxygen delivery due to dilutional anaemia
- hypothermia
- worsening metabolic acidosis (especially hyperchloremic non-anion gap metabolic acidosis from normal saline administration)
- clot dislodgement and haemorrhage from blood pressure elevation
References
- LITFL Hematology Hoodwinker 002 – Recombinant Factor VIIa to the rescue!?
- LITFL Hematology Hoodwinker 003 – Managing the Critical Bleeder!!
- Bickell WH, Wall Jr MJ, et al. Immediate vs. Delayed Fluid Resuscitation for Hypotensive Patients with Penetrating Torso Injuries. N Engl J Med. 1994; 331:1105 [Free fulltext]
- Deakin CD, Low JL. Accuracy of the advanced trauma life support guidelines for predicting systolic blood pressure using carotid, femoral, and radial pulses: observational study. BMJ. 2000 Sep 16;321(7262):673-4. PubMed PMID: 10987771; PubMed Central PMCID: PMC27481.
- Duchesne JC, et al. Damage control resuscitation: from emergency department to the operating room. Am Surg 2011; 2:201-6. Pubmed PMID: 21337881
- Fildes J, et al. Advanced Trauma Life Support Student Course Manual (8th edition), American College of Surgeons 2008.
- Guly HR, Bouamra O, Little R, Dark P, Coats T, Driscoll P, Lecky FE. Testing the validity of the ATLS classification of hypovolaemic shock. Resuscitation. 2010 Sep;81(9):1142-7. PubMed PMID: 20619954.
- Legome E, Shockley LW. Trauma: A Comprehensive Emergency Medicine Approach, Cambridge University Press, 2011.
- LITFL CCC — Major Haemorrhage in Trauma
- Marx JA, Hockberger R, Walls RM. Rosen’s Emergency Medicine: Concepts and Clinical Practice (7th edition), Mosby 2009. [mdconsult.com]
- Poulton TJ. ATLS paradigm fails. Ann Emerg Med. 1988 Jan;17(1):107. PubMed PMID: 3337405.
- Resus.ME — European Trauma Bleeding Guidelines updated
- Thomas I, Dixon J. Bradycardia in acute haemorrhage. BMJ. 2004 Feb 21;328(7437):451-3. PubMed PMID: 14976102; PubMed Central PMCID: PMC344269.
- Thompson D, Adams SL, Barrett J. Relative bradycardia in patients with isolated penetrating abdominal trauma and isolated extremity trauma. Ann Emerg Med. 1990 Mar;19(3):268-75. PubMed PMID: 2310066.
CLINICAL CASES
Trauma Tribulation
Chris is an Intensivist and ECMO specialist at The Alfred ICU, where he is Deputy Director (Education). He is a Clinical Adjunct Associate Professor at Monash University, the Lead for the Clinician Educator Incubator programme, and a CICM First Part Examiner.
He is an internationally recognised Clinician Educator with a passion for helping clinicians learn and for improving the clinical performance of individuals and collectives. He was one of the founders of the FOAM movement (Free Open-Access Medical education) has been recognised for his contributions to education with awards from ANZICS, ANZAHPE, and ACEM.
His one great achievement is being the father of three amazing children.
On Bluesky, he is @precordialthump.bsky.social and on the site that Elon has screwed up, he is @precordialthump.
| INTENSIVE | RAGE | Resuscitology | SMACC