Ultrasound Case 097
Presentation
A 47 year old previously healthy man presents with sore throat / neck, dry cough and shortness of breath for 2 weeks. This had not improved despite inhalers and a course of antibiotics. He also describes widespread aches and pains including in both calves. There is some swelling in his right lower neck and you wonder whether it is lymphadenopathy, an abscess or something else.
Image 2: Longitudinal view of the right IJV.
Image 3: Transverse view of the left lower neck.
Image 4: Right lower chest and costophrenic recess.
Image 6: CT Chest.
Describe and interpret these scans
IMAGE INTERPRETATION
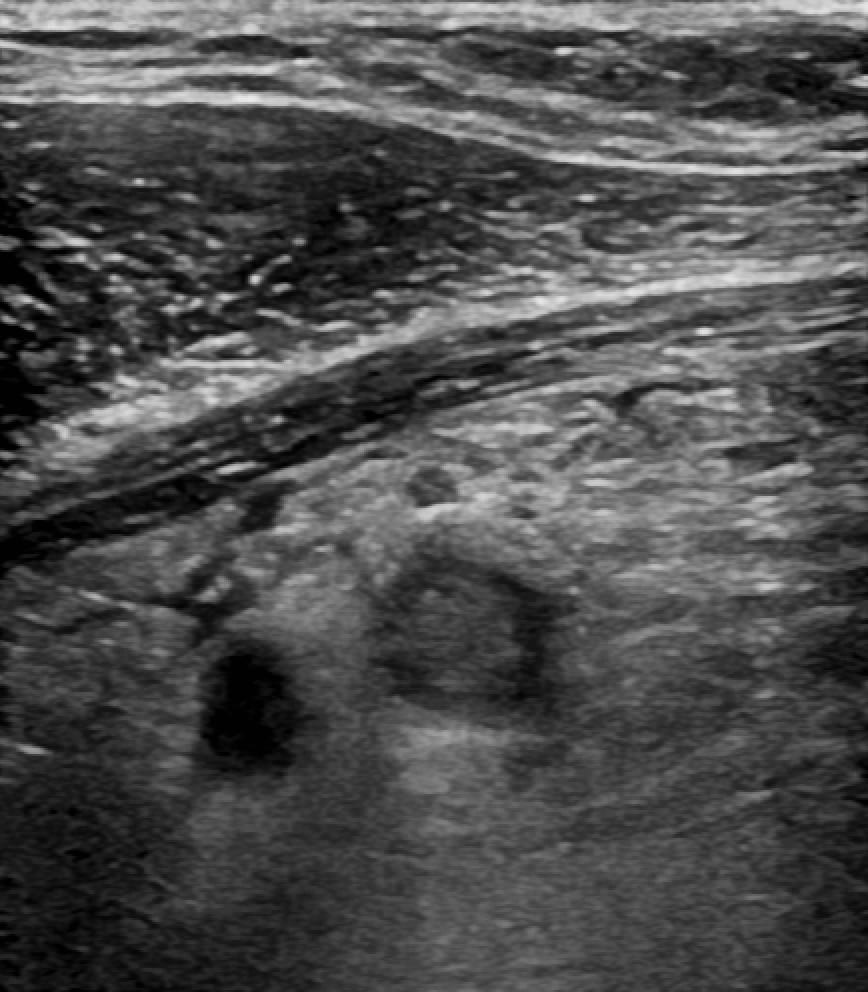
Image 1: Transverse view of the right internal jugular vein (IJV).
The IJV contains heterogeneous and echogenic thrombus. There is oedema surrounding the vein with echogenic fat and numerous lymph nodes. This suggests inflammatory change and thrombophlebitis.

Image 2: Longitudinal view of the right IJV.
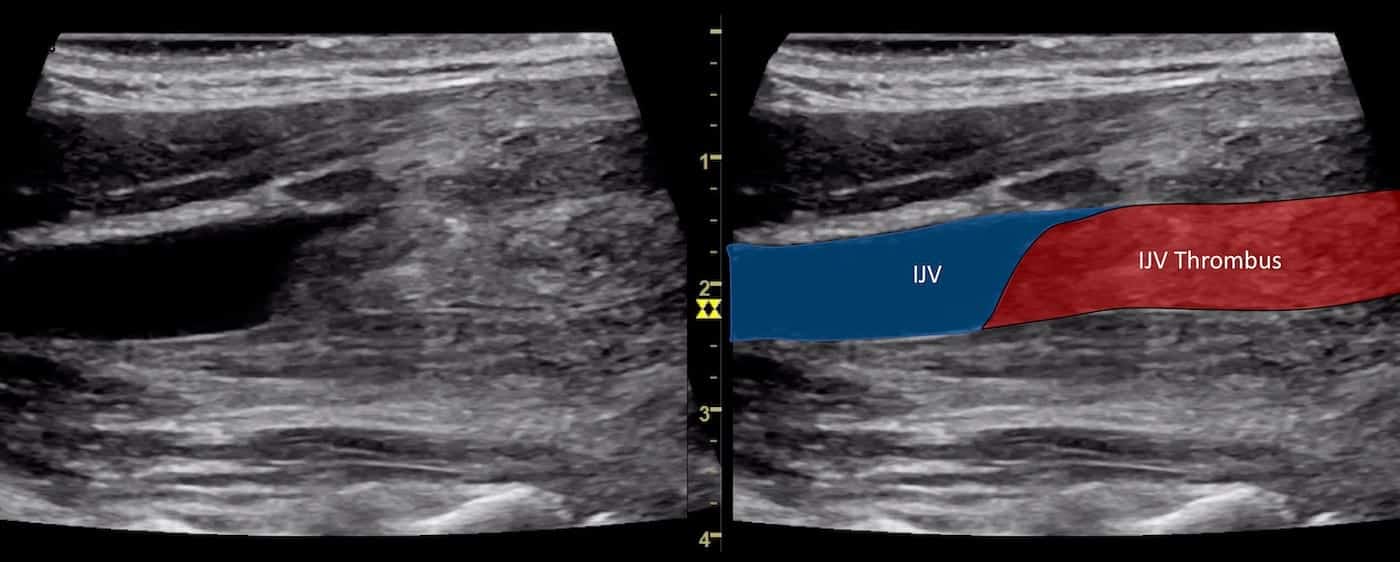
Image 3: Transverse view of the left lower neck.
Marked lymphadenopathy is seen. The appearance of these nodes is concerning for malignancy.
Image 4: Right lower chest and costophrenic recess.
There is a pleural effusion with fine echogenic debris. This is non-specific but is definitely not a transudate which would be anechoic. The relatively anechoic area in the posterior costophrenic recess is due to mirror artefact.
Image 5: Transverse view of the axillary vessels.
The thrombophlebitis extends into the deep vessels of the right upper limb.
Image 6: CT Chest.
Visualize the significant cervical lymphadenopathy, mediastinal mass extending from the right lung hilum, small bilateral subsegmental pulmonary embolisms and right pleural effusion and consolidation of the right lower lung with an appearance concerning for lymphangitis carcinomatosis.
CLINICAL CORRELATION
Primary lung malignancy with pleural effusion, lymph node metastases and paraneoplastic migratory thrombophlebitis with pulmonary emboli. Trousseau syndrome
Internal jugular vein thrombophlebitis.
Simple internal jugular vein thrombosis usually does not demonstrate the degree of perivenous inflammatory change seen in this case. This is thrombophlebitis and the differential we considered was infectious thrombophlebitis or paraneoplastic thrombophlebitis. Lemierre syndrome could certainly cause this appearance. Lemierre’s is infectious thrombophlebitis of the IJV usually in previously well people, the usual organism being Fusobacterium necrophorum. You would expect the patient to be very unwell with sepsis and our patient was remarkably well clinically.
Lymph node morphology.
Reactive and normal lymph nodes usually look like small kidneys (reniform). They have a defined hilum where vessels enter and emerge, an echogenic centre and a surrounding hypoechoic cortex. They usually lie transverse to the skin and their long axis lies parallel to the skin.
With malignant involvement lymph nodes become disorganised, enlarged and lose their traditional morphological signature. They often change shape, becoming “taller than wide”, and appear round or lobulated. They lose the differentiation between the cortex and medulla and frequently become hypoechoic. Their vascularity changes and instead of a single central hilum, disorganised flow patterns emerge. It is important to realize that there is a broad spectrum of the appearance of lymph nodes benign and malignant, with considerable overlap. Clinical correlation is essential and biopsy with histology the only path to a definitive diagnosis.
The Trousseau sign of malignancy or Trousseau syndrome is a recurrent and migratory thrombophlebitis that may involve superficial or deep veins. It is most commonly associated with the hypercoagulable state induced by adenocarcinoma (particularly pancreatic, gastric or lung).
In this case a primary lung adenocarcinoma with pleural effusion and extensive lymph node metastasises was present. In addition thrombophlebitis of the right IJV and deep veins of the right upper limb was present. Clots in both popliteal veins were also demonstrated as were several bilateral small pulmonary emboli.
FURTHER READING
- Armand Trousseau (1801-1867) and Trousseau syndrome
- Trousseau A. Lectures on clinical medicine: delivered at the Hôtel-Dieu, Paris. 1861
- André-Alfred Lemierre (1875-1956) and Lemierre syndrome (1936)
- Lemierre A. On certain septicemias due to anaerobic organisms. Lancet. 1936; 227(5874): 701-703
TOP 100 ULTRASOUND CASES