You’re blind and your hair is a mess
aka Ophthalmology Befuddler 022
A 65 year-old man presents with sudden onset painless loss of vision affecting the lower half his right eye’s visual field. He says he skipped breakfast because it hurt to chew, and his hair is mess because it was too painful to comb. He has a low-grade fever and has been losing weight recently.
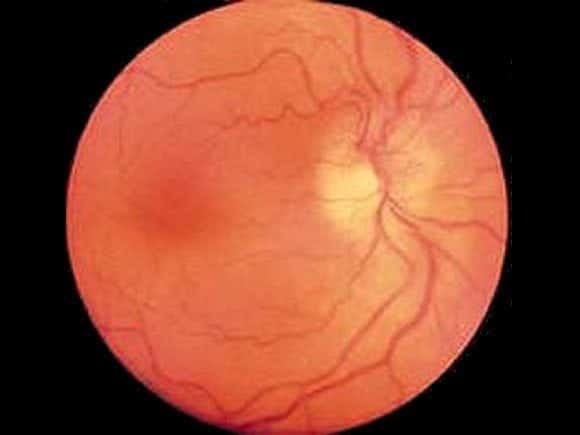
He can barely count fingers with his right eye, there is a relative afferent pupillary defect, he has a tender and palpable right temporal artery and on fundoscopy you see this:
Questions
Q1. What is the likely diagnosis?
Answer and interpretation
Anterior ischemic optic neuropathy (AION) due to giant cell arteritis
The history and examination is classic for giant cell arteritis, and papilloedema is evident on funduscopy.
Q2. What are the features on history?
Answer and interpretation
History:
- visual loss: sudden and painless, can be severe and bilateral, may be preceded by amaurosis fugax. 1/2 unilateral, 1/3 sequential, 1/6 bilateral.
- local symptoms: temporal headache, scalp tenderness (pain on combing hair), jaw claudication (pain with chewing)
- systemic symptoms: fever and night sweats, weight loss, malaise, anorexia
- polymyalgia rheumatica: generalised muscle pain and weakness, predominatly affects the muscles of the limb girdles
- age >50y (very rare younger than this, incidence rises with age)
- assess for factors that may complicate steroid treatment – e.g. peptic ulcer disease, GI bleeding, poorly controlled diabetes, Tb.
Q3. What are the features on examination?
Answer and interpretation
Examination:
- Visual acuity — poor e.g. CF only
- Visual fields — defect may be present, respects the horizontal meridian (‘altitudinal’) or central
- External examination — palpable and tender non-pulsatile temporal artery
- Pupils — RAPD
- Fundoscopy — papilloedema and flame-shaped hemorrhages may be seen, optic atrophy occurs late
Q4. Describe the investigation and management of this condition.
Answer and interpretation
Referral to ophthalmologist and arrange:
Immediate ESR/CRP (can be normal!) – thrombocytosis may also be present
Urgent treatment with corticosteroids: start when the diagnosis is suspected, do not wait for confirmation.
- use high-dose IV methyprednisolone initially — e.g. 250 mg IV q6h for 72 hours — more effective than oral prednisone in promoting recovery of vision and preventing the fellow eye from being affected; 1/3 with visual loss will recover.
- follow with oral prednisolone ~ 1mg/kg until GCA ruled out, or until symptoms improve and ESR normalises — then a reducing dose over 6-12+ months is commonly used.
- consider ulcer prophylaxis and risk of osteoporosis.
Temporal artery biopsy to confirm the diagnosis of GCA
- perform within 1 week of symptom onset.
- if negative on a 2cm biopsy but GCA is highly suspected, biopsy the other temporal artery
- if negative stop treatment with prednisolone unless the presentation is classic and responded to steroid
Q5. What is the upper limit of normal for ESR?
Answer and interpretation
A guide to the upper limit of normal ESR is:
- age/2 for men
- (age + 10)/2 for women
Q6. What other types of ischemic optic neuropathy are there?
Answer and interpretation
In addition to arteritic ischemic neuropathy (which is commonly caused by GCA, but can occur in other forms of vasculitis), there is also:
- Non-arteritic ischemic optic neuropathy: presents similar to arteritic ION but is usually less severe, and is without the systemic features or scalp/ facial symptoms. It is generally idiopathic, although may be linked to typical cardiovascular risk factors. The condition may be progressive or non-progressive and it is unclear if steroids are beneficial.
- Postoperative ischemic optic neuropathy: occurs within 1 week of general anesthesia and is of uncertain etiology. It is associated with many different types of surgery, as well as head-down positioning and prolonged operative times. Correction of intra-operative hypotension and anemia may be beneficial.
Q7. What is the differential diagnosis of ischemic optic neuropathy?
Answer and interpretation
- optic neuritis
- other optic neuropathies — e.g. glaucoma, compressive optic neuropathy, radiation optic neuropathy, metabolic and toxic optic neuropathies
- central retinal vein occlusion
- central retinal artery occlusion
- chiasmal and post-chiasmal visual loss
References
- Ehlers JP, Shah CP, Fenton GL, Hoskins EN. The Wills Eye Manual: Office and Emergency Room Diagnosis and Treatment of Eye Disease Lippincott Williams & Wilkins
- NSW Statewide Opthalmology Service. Eye Emergency Manual — An illustrated Guide. [Free PDF]

OPHTHALMOLOGY BEFUDDLER
Chris is an Intensivist and ECMO specialist at The Alfred ICU, where he is Deputy Director (Education). He is a Clinical Adjunct Associate Professor at Monash University, the Lead for the Clinician Educator Incubator programme, and a CICM First Part Examiner.
He is an internationally recognised Clinician Educator with a passion for helping clinicians learn and for improving the clinical performance of individuals and collectives. He was one of the founders of the FOAM movement (Free Open-Access Medical education) has been recognised for his contributions to education with awards from ANZICS, ANZAHPE, and ACEM.
His one great achievement is being the father of three amazing children.
On Bluesky, he is @precordialthump.bsky.social and on the site that Elon has screwed up, he is @precordialthump.
| INTENSIVE | RAGE | Resuscitology | SMACC
