ECG Case 049
Elderly male presenting with dizziness. Describe the ECG
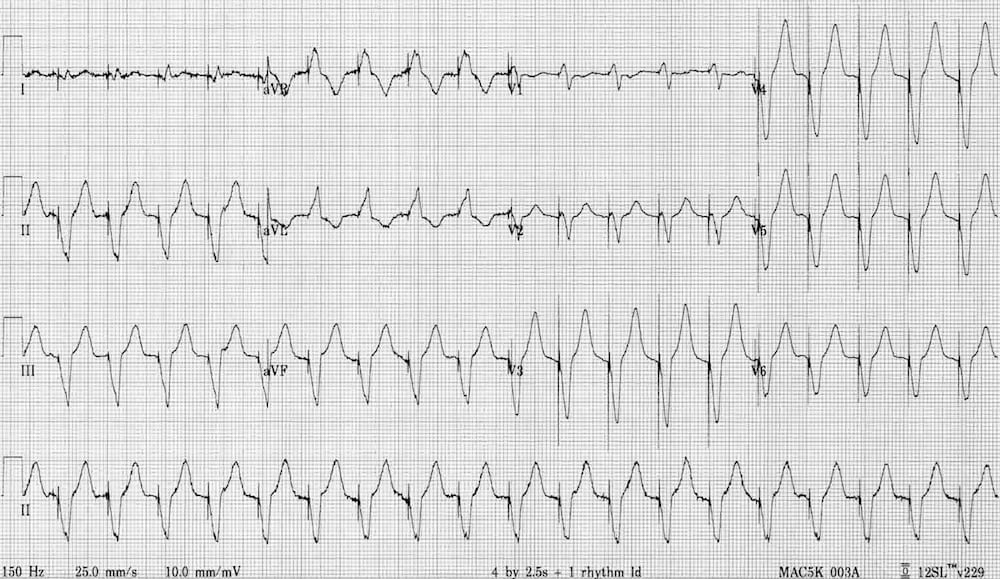
Describe and interpret this ECG
ECG ANSWER and INTERPRETATION
Main Abnormalities
- Broad complex tachycardia at ~ 120 bpm.
- Pacing spikes precede each QRS complex.
- LBBB morphology (dominant S wave in V1-2) indicates a pacing electrode in the right ventricle.
- Negative concordance is seen in V1-6 (all precordial leads
show negative complexes). This is an often-cited feature of VT, but also
occurs with paced rhythms. It simply indicates that ventricular
depolarisation is spreading from anterior to posterior (away from V1-6),
e.g. due to a pacemaker electrode stimulating the anterior wall of the
RV.
These features are consistent with a pacemaker malfunction resulting in a rapid ventricular-paced rhythm.
Differential Diagnosis
The differential diagnosis of this rhythm includes:
- Pacemaker-mediated tachycardia
- Sensor-induced tachycardia
- Atrial tachycardia (e.g. sinus, AF) driving the pacemaker to its
maximum rate — may be appropriate response to exercise, shock, sepsis,
etc.
Pacemaker Mediated Tachycardia (PMT)
This is a re-entrant rhythm involving the pacemaker circuit. It behaves very much like the atrioventricular re-entry tachycardia (AVRT) seen with WPW syndrome, except that in this case the “accessory pathway” is formed by the pacemaker circuit.
PMT is triggered when ventricular impulses pass retrogradely through the AV node and depolarise the atria.
The retrograde P wave is sensed by the pacemaker, which then immediately paces the ventricles. This is followed by another retrograde P wave that maintains the circus movement.
The rhythm can be terminated by activating magnet mode (which switches off sensing), or by reprogramming the pacemaker box (e.g. increasing the refractory period to “block out” the retrograde P waves).
Sensor Induced Tachycardia (SIT)
- Modern pacemakers are programmed to allow increased heart rates in
response to physiological stimuli such as exercise, tachypnoea,
hypercapnia or acidaemia. - Sensors may “misfire” in the presence of distracting stimuli such as
vibrations, loud noises, fever, limb movement, hyperventilation or
electrocautery (e.g. during surgery). - This misfiring leads to pacing at an inappropriately fast rate.
- The ventricular rate cannot exceed the pacemaker’s upper rate limit.
- Similar to PMT, these may also terminate with application of a magnet, or with removal of the inciting stimulus.
CLINICAL PEARLS
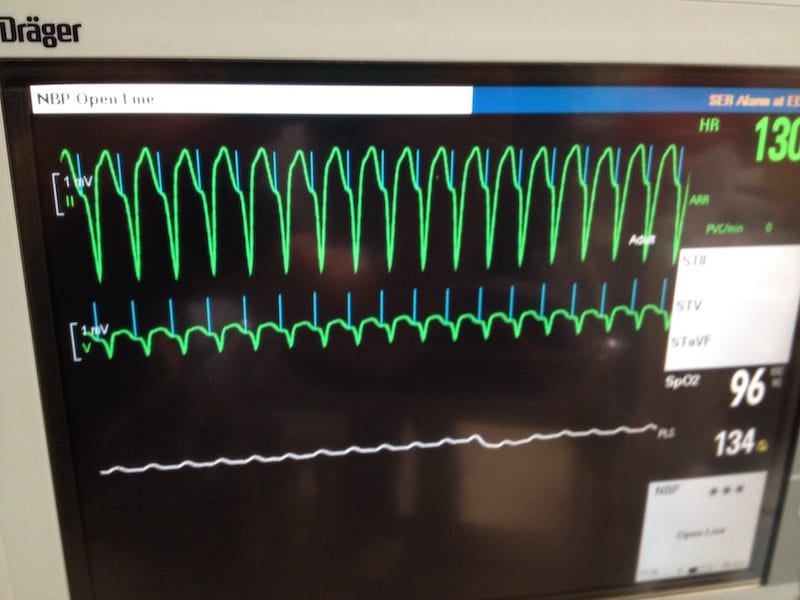
Tips for Dealing with Rapid Paced Rhythms
If the patient is attached to critical care monitoring, ensure that you switch off respiratory impedence monitoring mode (where the monitor senses respiratory rate via the ECG electrodes). This gives off an electrical signal that is known to interfere with pacemakers. If this doesn’t work, try changing monitors to one that does not use respiratory impedance technology.
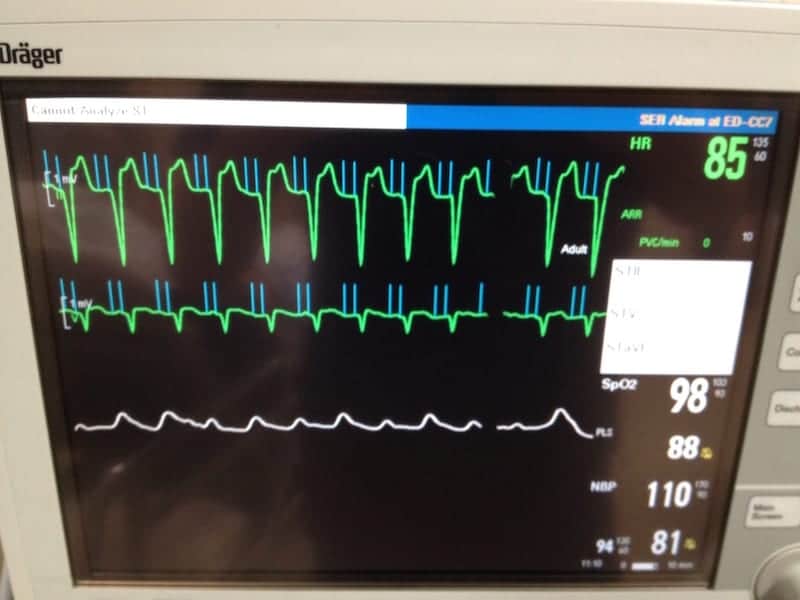
Apply a magnet to the pacemaker box. This activates magnet mode, which resets the pacemaker to provide temporary asynchronous pacing (AOO, VOO or DOO).
Arrange for an urgent pacemaker check. A pacemaker technician may be able to adjust the settings to terminate the dysrhythmia and prevent its recurrence.
If a pacemaker technician is not readily available, then a trial of AV nodal blocking drugs (e.g. beta blockers, verapamil) may be successful in terminating PMT.
References
Further Reading
- Wiesbauer F, Kühn P. ECG Mastery: Yellow Belt online course. Understand ECG basics. Medmastery
- Wiesbauer F, Kühn P. ECG Mastery: Blue Belt online course: Become an ECG expert. Medmastery
- Kühn P, Houghton A. ECG Mastery: Black Belt Workshop. Advanced ECG interpretation. Medmastery
- Rawshani A. Clinical ECG Interpretation ECG Waves
- Smith SW. Dr Smith’s ECG blog.
- Wiesbauer F. Little Black Book of ECG Secrets. Medmastery PDF
TOP 100 ECG Series
Emergency Physician in Prehospital and Retrieval Medicine in Sydney, Australia. He has a passion for ECG interpretation and medical education | ECG Library |

What about T wave in this case? No hyperkalemia?