AVNRT for two
A 56 year old year old woman presents to the Emergency Department with a referral from her General Practitioner for “assessment and management of severe tachycardia and possible myocardial infarction” following a sudden onset of palpitations. Objectively she was found to have a regular tachycardia with no overt signs of cardiovascular compromise.
- The patient described experiencing the sudden onset of palpitations whilst cleaning at 10:30am that morning. She stated that the palpitations came on without warning and had not gone away after she ceased cleaning to lie down – they were ‘regular and extremely fast’. There were no associated symptoms of shortness of breath, dizziness or chest pain. Five hours later, upon her presentation to the Emergency Department, the rapid heart rate is still continuing.
- She describes to you a five year history of occasional episodes of suddenly increased heart rate, but in all cases, they self-resolved within one minute and she did not seek medical investigation or treatment.
- On examination in the emergency department, her heart rate is 160bpm and regular, RR 20bpm and BP 134/75. She was apyrexial and saturating at 97% on room air. Cardiovascular and respiratory examination revealed no abnormalities aside from the tachycardia.
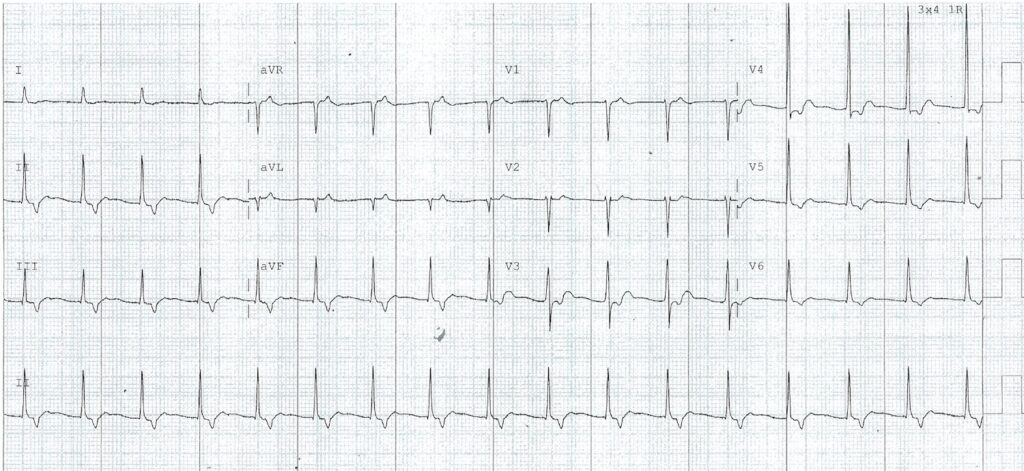
ECG On Arrival
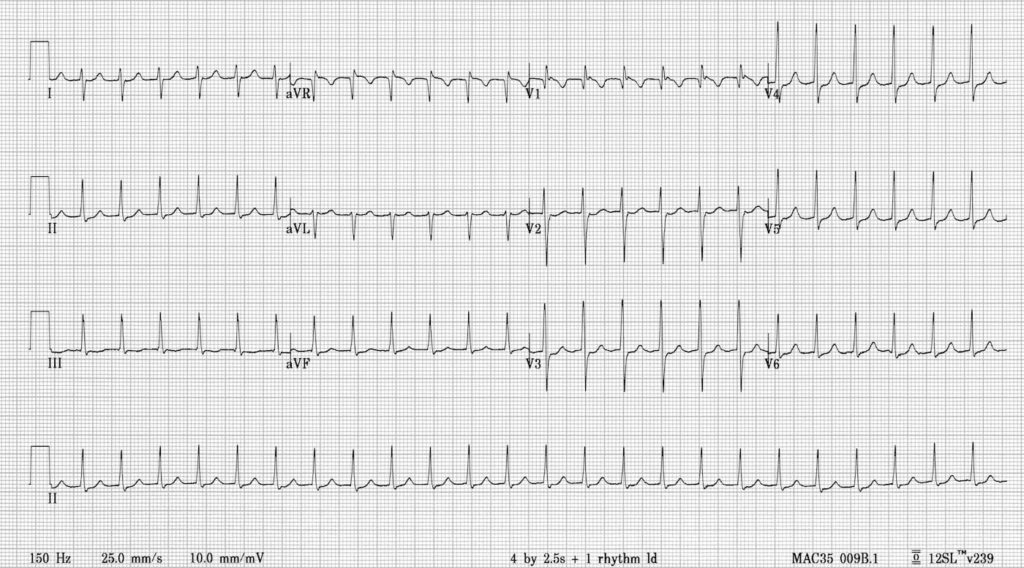
On the history, examination and ECG findings, the patient was diagnosed with ‘Slow-Fast AVNRT’ (Atrioventricular Nodal Reentrant Tachycardia) and successfully treated with 6mg of adenosine.
What is AVNRT?
Atrioventricular Nodal Reentrant Tachycardia is a type of supraventricular tachycardia (ie it originates above the level of the Bundle of His) and is the commonest cause of palpitations in patients with hearts exhibiting no structurally abnormality.
Clinical Features of AVNRT
- AVNRT is typically paroxysmal and may occur spontaneously in patients or upon provocation with exertion, coffee, tea or alcohol. It is more common in women than men (~75% of cases occurring in women) and may occur in young and healthy patients as well as those suffering chronic heart disease.
- Patients will typically complain of the sudden onset of rapid, regular palpitations. The patient may experience a brief fall in blood pressure causing presyncope or occasionally syncope.
- If the patient has underlying coronary artery disease the patient may experience chest pain similar to angina (tight band around the chest radiating to left arm or left jaw).
- The patient may complain of shortness of breath, anxiety and occasionally polyuria due to elevated atrial pressure releasing atrial natriuretic peptide.
- The tachycardia typically ranges between 140-280 bpm and is regular in nature. It may cease spontaneously (and abruptly) or continue indefinitely until medical treatment is sought.
- The condition is generally well tolerated and is rarely life threatening in patients with pre-existing heart disease.
Pathophysiology and types of AVNRT
- AVNRT is caused by a reentry circuit in or around the AV node.
- The circuit is formed by the creation of two pathways forming the re-entrant circuit, namely the slow and fast pathways.
- The fast pathway is usually anteriorly situated along septal portion of tricuspid annulus with the slow pathway situated posteriorly, close to the coronary sinus ostium.
- Sustained reentry occurs over a circuit comprising the AV node, His Bundle, ventricle, accessory pathway and atrium.
- The various forms of AVNRT can be described in terms of ECG appearance such as R-P intervals or Slow/Fast pathway dominance.
Descriptive Terminology
The ‘descriptive’ terminology regarding AVNRT classification can be confusing…and I am still confused!
Slow-Fast AVNRT (Common AVNRT)
- Accounts for 80-90% of AVNRT
- Associated with Slow AV nodal pathway for anterograde conduction and Fast AV nodal pathway for retrograde conduction.
- The retrograde P wave is obscured in the corresponding QRS or occurs at the end of the QRS complex as pseudo r’ or S waves
- ECG:
- P waves are often hidden – being embedded in the QRS complexes.
- Pseudo r’ wave may be seen in V1
- Pseudo S waves may be seen in leads II, III or aVF.
- In most cases this results in a ‘typical’ SVT appearance with absent P waves and tachycardia
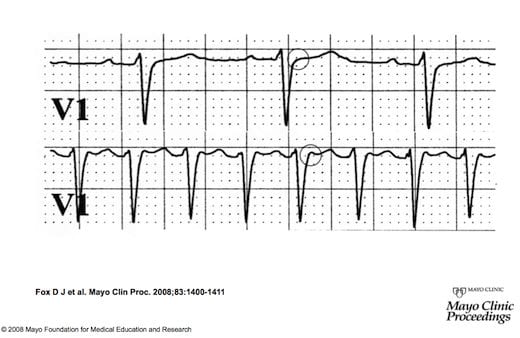
Cardiac rhythm strips demonstrating (top) sinus rhythm and (bottom) paroxysmal supraventricular tachycardia. The P wave is seen as a pseudo-R wave (circled in bottom strip) in lead V1during tachycardia. By contrast, the pseudo-R wave is not seen during sinus rhythm (it is absent from circled area in top strip). This very short ventriculoatrial time is frequently seen in typical Slow-Fast Atrioventricular Nodal Reentrant Tachycardia.
Fast-Slow AVNRT (Uncommon AVNRT)
- Accounts for 10% of AVNRT
- Associated with Fast AV nodal pathway for anterograde conduction and Slow AV nodal pathway for retrograde conduction.
- The retrograde P wave appears after the corresponding QRS
- ECG
- QRS -P-T complexes
- P waves are visible between the QRS and T wave
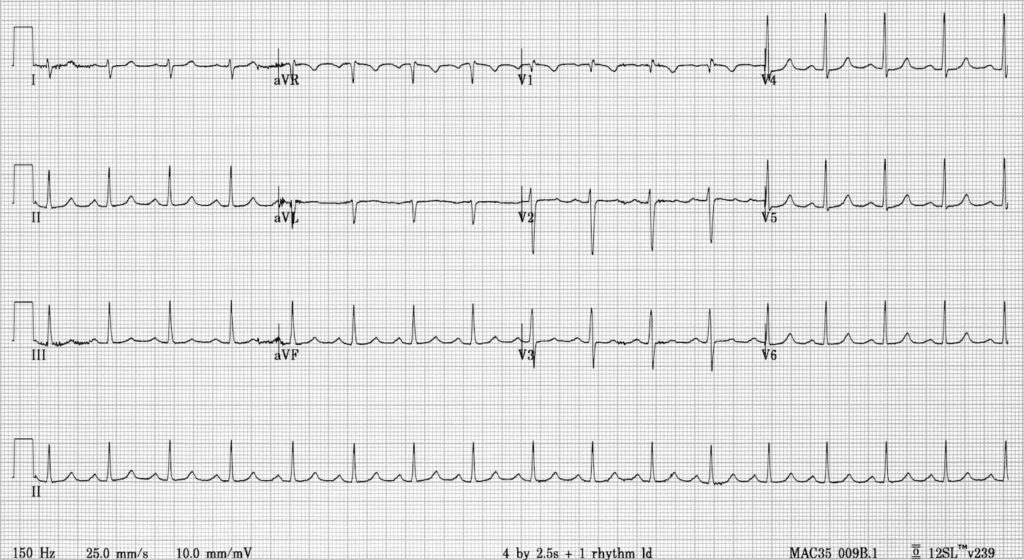
Example 1
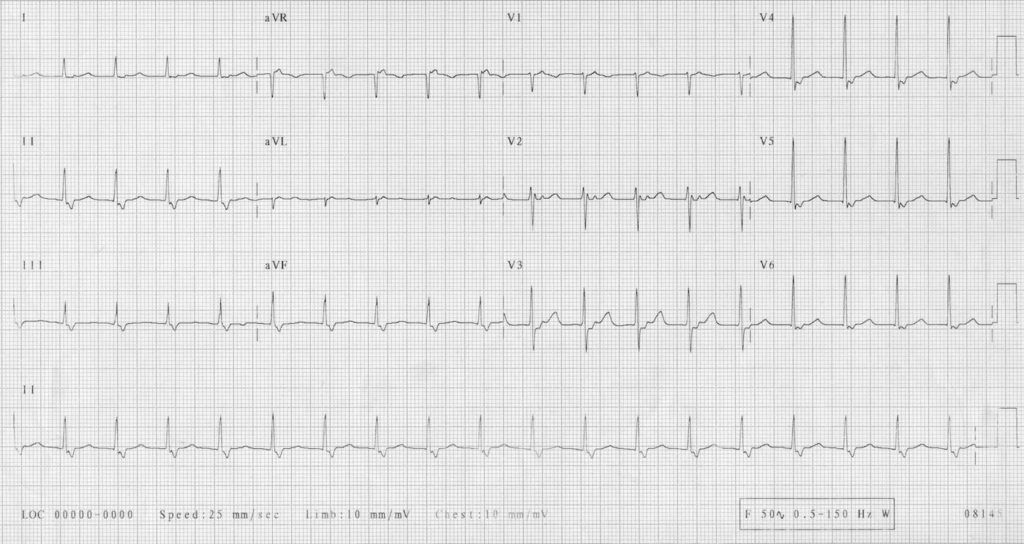
Example 2
Slow-Slow AVNRT (AtypicalAVNRT)
- 1-5% AVNRT
- Associated with Slow AV nodal pathway for anterograde conduction and Slow left atrial fibres approaching the AV node as the pathway for retrograde conduction.
- ECG: Tachaycardia with a P-wave seen in mid-diastole… effectively appearing ‘before the QRS complex’…
- Confusing as a P wave appearing before the QRS complex in the face of a tachycardia might honestly be read as a sinus tachycardia…
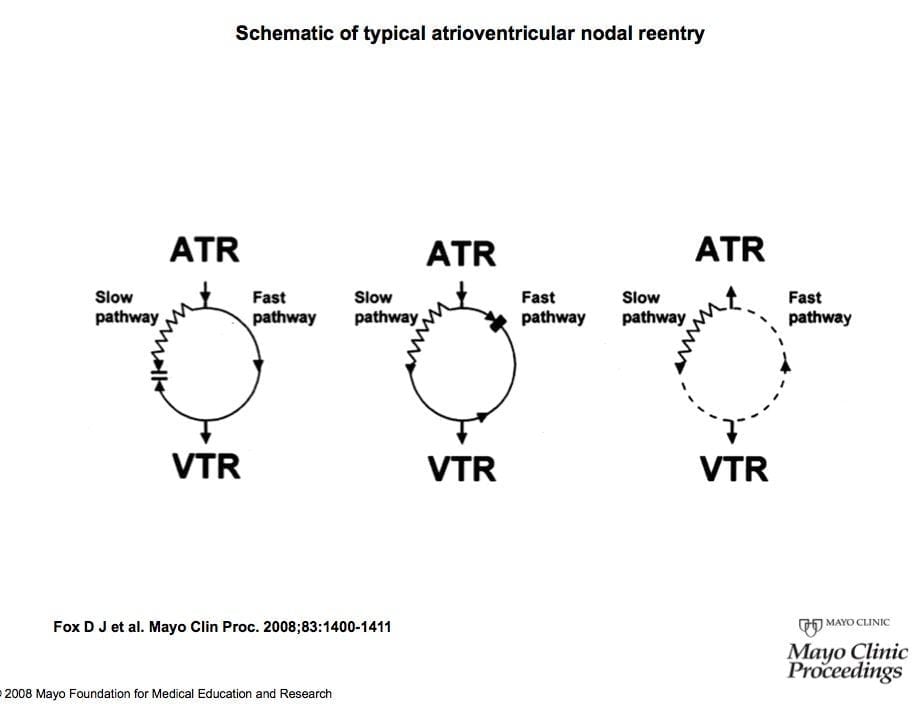
- Left Panel: Anterograde conduction from the atrium (ATR) to the ventricle (VTR) over both slow and fast pathways. The ventricle is activated initially in sinus rhythm by the fast pathway.
- Centre Panel: The effect of a premature atrial complex (PAC). Although the fast pathway conducts rapidly, it repolarizes slowly. In this hypothetical scenario, the fast pathway is refractory to the PAC, allowing the PAC to proceed via the slow pathway, which has a shorter refractory period.
- Right Panel: Anterograde conduction of the PAC occurs via the slow pathway, with subsequent recovery of the fast pathway. These conditions allow retrograde conduction into the atrium via the fast pathway, thereby creating the first beat of typical slow-fast atrioventricular nodal reentrant tachycardia.
Investigations
The ECG will typically show a tachycardia of 140-280 bpm with normal and regular QRS complexes. There will be either
- No visible P-waves (hidden within the QRS complex) or
- P-waves immediately before the QRS or
- P-waves immediately after the QRS complex
For recurrent episodes of palpitations, a Holter monitor and EPS may be useful in identifying rhythms typical of AVNRT. An echocardiogram may be useful in evaluating for structural heart disease and electrophysiological studies may be necessary if considering ablative therapy. Blood tests that may be appropriate in patients experiencing palpitations include cardiac markers (to investigate for myocardial infarction), urea and electrolytes (to identify imbalances in potassium, magnesium or calcium) or thyroid function tests (hyperthyroidism may trigger AVNRT or other arrhythmias).
Management
Patients may be instructed to undertake vagal manoeuvres upon the onset of symptoms which can be effective in stopping the AVNRT. This may involve carotid sinus massage or valsalva manoeuvres, which will both stimulate the vagus nerve. Alternative strategies include:
- Adenosine, beta-blockers or calcium channel blockers can suppress an AVNRT event by blocking or slowing the AV node. Other second-line therapies may include amiodarone or flecainide.
- Cardioversion is rarely used on patients with AVNRT, usually when the tachycardia is refractory to other medical therapies or the tachycardia is causing haemodynamic instability (falling blood pressure, development of heart failure etc.)
- Radiofrequency catheter ablation can be offered to patients with frequent attacks for whom medical therapy isn’t appropriate in the long term, and can be curative.
Advanced Reading
Online
- Wiesbauer F, Kühn P. ECG Mastery: Yellow Belt online course. Understand ECG basics. Medmastery
- Wiesbauer F, Kühn P. ECG Mastery: Blue Belt online course: Become an ECG expert. Medmastery
- Kühn P, Houghton A. ECG Mastery: Black Belt Workshop. Advanced ECG interpretation. Medmastery
- Rawshani A. Clinical ECG Interpretation ECG Waves
- Smith SW. Dr Smith’s ECG blog.
- Wiesbauer F. Little Black Book of ECG Secrets. Medmastery PDF
Textbooks
- Zimmerman FH. ECG Core Curriculum. 2023
- Mattu A, Berberian J, Brady WJ. Emergency ECGs: Case-Based Review and Interpretations, 2022
- Straus DG, Schocken DD. Marriott’s Practical Electrocardiography 13e, 2021
- Brady WJ, Lipinski MJ et al. Electrocardiogram in Clinical Medicine. 1e, 2020
- Mattu A, Tabas JA, Brady WJ. Electrocardiography in Emergency, Acute, and Critical Care. 2e, 2019
- Hampton J, Adlam D. The ECG Made Practical 7e, 2019
- Kühn P, Lang C, Wiesbauer F. ECG Mastery: The Simplest Way to Learn the ECG. 2015
- Grauer K. ECG Pocket Brain (Expanded) 6e, 2014
- Surawicz B, Knilans T. Chou’s Electrocardiography in Clinical Practice: Adult and Pediatric 6e, 2008
- Chan TC. ECG in Emergency Medicine and Acute Care 1e, 2004
LITFL Further Reading
- ECG Library Basics – Waves, Intervals, Segments and Clinical Interpretation
- ECG A to Z by diagnosis – ECG interpretation in clinical context
- ECG Exigency and Cardiovascular Curveball – ECG Clinical Cases
- 100 ECG Quiz – Self-assessment tool for examination practice
- ECG Reference SITES and BOOKS – the best of the rest
ECG LIBRARY

Hi,
Just wanted to ask re: slow-slow and fast-slow pathways. Most other sources, including Braunwald, state that slow-slow AVNRT has the retrograde p-wave buried in the T-wave (or midway in the cardiac cycle), and that fast-slow AVNRT typically has the retrograde p-wave appear before the QRS. How does that line up with the information here, which essentially states it is the other way around?
From Braunwald – “In less than 5% to 10% of patients with AV nodal reentry, anterograde conduction proceeds over the
fast pathway and retrograde conduction over the slow pathway (termed the unusual or atypical form of
fast-slow AV nodal reentry), with production of a long VA interval and a relatively short AV interval
(generally an AV/VA ratio <0.75; see Fig. 37.8B). The least common form (slow-slow) exhibits a
retrograde P wave midway in the cardiac cycle.”
(also just a massive thank you for this site in general – it’s an amazing resource!)