Bone Marrow Transplantation
OVERVIEW
- used in a wide range of malignant and non-malignant disorders
- can be autologous or allogeneic
- autologous = donor and recipient are the same person (avoids GVHD)
- allogeneic = genetically different but from the same species (GVHD and doesn’t need to be stored, but a limited amount of GVHD may have an anti-tumour effect)
- don’t take an entirely nihilistic approach to these patients if marrow recovery is imminent.
- however, prolonged ventilation and/or dialysis in these patients results in a poor prognosis.
- hematopoietic stem cells are obtained from either marrow aspiration or from peripheral blood by apheresis using a blood cell separator following stimulation of the marrow with hematopoietic growth factors +/- chemotherapy.
PRINCIPLES
- tumour must be responsive to chemotherapy +/- radiotherapy
- the limitation of chemotherapeutic agents used must related to bone marrow toxicity and not other organs
- must have a source of un- or minimally contaminated hematopoietic stem cells (autologous or allogeneic)
- appropriate hematopoietic supportive therapy must be available during the marrow aplastic period
- high quality clinical and laboratory must be available for the collection and preservation of hematopoietic stem cells.
- strong MDT commitment
- well-documented clinical protocols and effective implementation
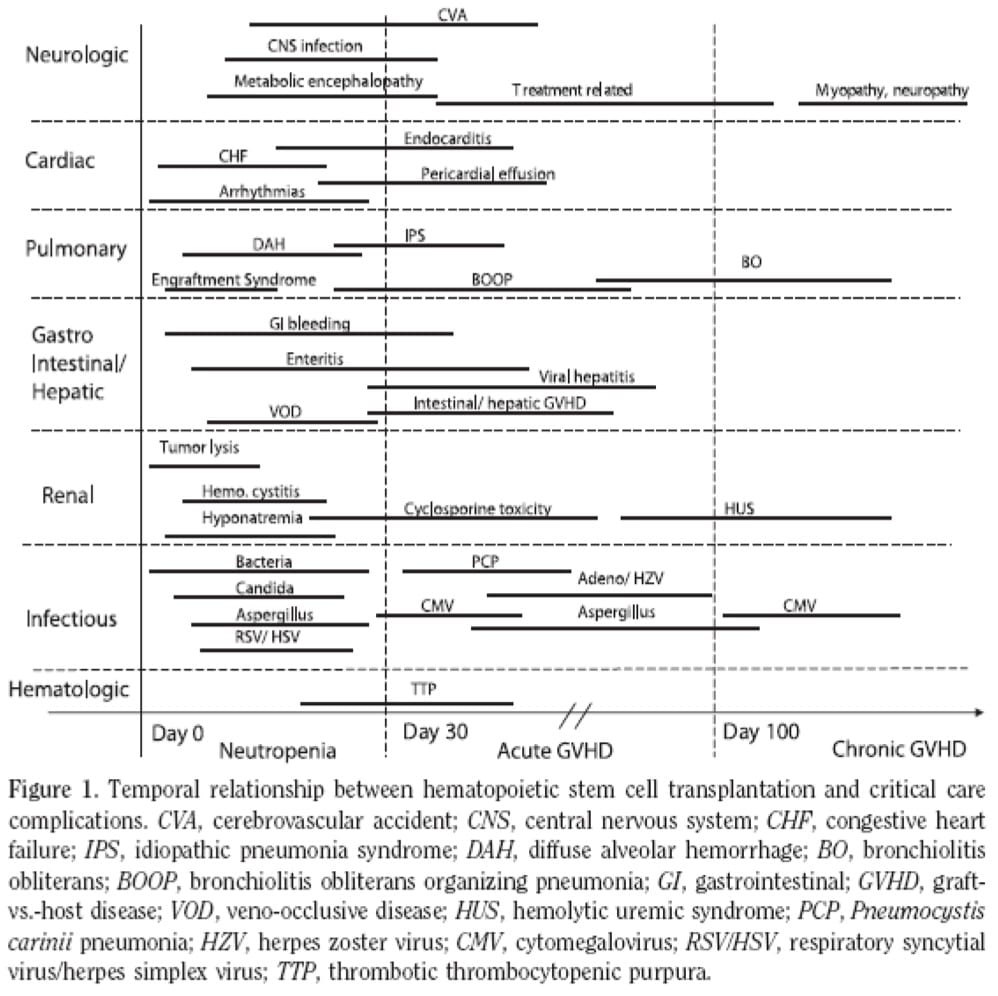
GENERAL OVERVIEW OF COMPLICATIONS
NEUROLOGICAL COMPLICATIONS
- > with allogeneic transplantation
- risk factors: high dose chemotherapy, immunosuppression, GVHD, thrombocytopaenia
CVA
- median day of presentation = 28
- usually haemorrhage (intracerebral, SAH) from thrombocytopaenia
- other causes: infarction from infection or thrombosis, non-bacterial endocarditis and embolism
- high mortality (70%)
- standard management
CNS Infections
- aspergillosis (main cause), CMV, HSV, toxoplasma, Candida, Cryptococcus, bacterial meningitis
- prognosis is extremely poor
Metabolic Encephalopathy
- > in allogeneic transplantation
- altered mental status, seizures, Wernicke encephalopathy (altered mental status, ataxia, ophthalmoplegia)
- causes: hypoxaemia, electrolyte abnormalities, metabolic acidosis, sepsis, hepatic failure, medications (sedatives and analgesics), thiamine deficiency
- supportive care
Treatment related neurological complications
- OKT3: aseptic meningitis (can decrease risk with corticosteroids)
- cranial radiation
- imipenem: seizures
- corticosteroids: myopathy, psychosis
- cyclosporine A: encephalopathy, leukoencephalopathy, generalised cerebellar dysfunction, hemiparesis, quadriplegia, seizures.
Graft vs Host Disease
- acute GVHD: encephalopathy associated with other organ dysfunction
- chronic GVHD: polyneuropathy, polymyositis, MG
- treatment: intensification of immunosuppressive therapy
CARDIAC COMPLICATIONS
Pulmonary oedema
- commonest cardiac indication for ICU admission
- risk factors: low EF, fluid overload, ARF, veno-occlusive disease, severe sepsis, anaemia and high dose chemotherapy
Pericardial tamponade
- rare
- usually related to: cyclophosphamide toxicity, viral syndrome, chronic GVHD, renal failure, bacterial infection (rarely)
Endocarditis
- rare (1.3%)
- clinical features are subtle: left sided murmurs, indwelling CVC’s, disruption of skin and mucosal barriers by high dose chemotherapy and GVHD
- organisms: Staph aureus, Strep viridans, fungal, aseptic
Arrhythmia
- electrolyte abnormalities
- hypoxaemia
- sepsis
- MOF
PULMONARY COMPLICATIONS
- many reasons
- bilateral pulmonary infiltrate differential =
(1) Pneumonia
- Viral – CMV, HSV, VSV
- Bacterial – see Pneumonia in the immunocompromised Document
- Fungal – Pneumocystis, Aspergillus, Candida
- Protozoa – Toxoplasma
(2) Engraftment syndrome
(3) Bronchiolitis obliterans +/- organizing pneumonia (BOOP)
(4) Diffuse alveolar haemorrhage
(5) Idiopathic pneumonia syndrome
- organisms causing infection are temporally distributed:
-> early (< 30 days): bacteria, candida, aspergillus, HSV, RSV
-> mid (30-100 days): CMV, PCP, adenovirus, HZV, aspergillus
-> late (> 100 days): CMV
GASTROINTESTINAL COMPLICATIONS
GVHD of Intestine
- clinical features: abdominal pain, N+V, diarrhoea, bleeding, may have peritonism, often associated with hepatitis and a skin rash (acute GVHD)
- CT: bowel wall oedema
- treatment: intensification of immunosuppressive therapy
Intestinal Pseudo-obstruction
- supportive and minimizing aggravating factors
Veno-occlusive Disease of Liver
- common
- may be mild -> rapidly fatal (in 40%)
- pathogenesis: thrombosis of the small central hepatic venules due to endothelial cell damage by high dose chemotherapy
- clinical features: during first 21 days following transplant, weight gain, tender liver, jaundice
- investigations: transaminitis, hyperbilirubinaemia, Doppler U/S showing reversal or diminished portal flow.
- management: supportive, fluid restriction, diuresis, paracentesis, avoid infections and hepatotoxic medications, oral ursodeoxycholic acid (lowers bilirubin) possibly thrombolytics
GI Bleeding
- diffuse mucosal bleeding of the small intestine, mucosal ulcers and necrosis
- causes: chemotherapy induced, GVHD, adenovirus, CMV
- management: supportive, endoscopy (rarely required), surgery
Enteritis
- mild to self limiting -> severe dehydration, hypotension and ARF
- causes: GVHD, bacterial infection (clostridia), viral infections (rotavirus, adenovirus, CMV, HSV, HZV)
- treatment: supportive, octreotide (decrease secretory hormones), rotavirus (oral immunoglobulins)
Intestinal Perforation
- causes: CMV ulcers, corticosteroids, GVHD
- treatment: standard care
Pancreatitis
- rare
- causes: medications (cotrimoxazole, corticosteroids, cyclosporine A), infections (CMV and adenovirus), GVHD, biliary sludge
- treatment: standard
Other Liver Disease
- viral hepatitis: adenovirus, HSV, HZV, CMV, Hep B and C
- acute GVHD: rarely producers fulminant liver failure
- fungal infection: liver involvement of Candida and Aspergillus
RENAL COMPLICATIONS
- if develops the need for dialysis -> mortality 90%
Tumour Lysis Syndrome
- rare as tumour burden is reduced prior to transplantation
- clinical features: hyperuricaemia, hyperkalaemia, hyperphosphataemia, hypocalcaemia, renal failure
- treatment: IVF, allopurinol, rasburicase, phosphate binders, dialysis
Infusion of Stem Cells
- haemolysis -> haemoglobinuria -> proximal ATN -> ARF
- treatment: hydration, alkalinsation
Haemorrhagic Cystitis
- risk factors: cyclophosphamide, busulfan, irradiation, viral infections
- prevention: IVF, diuresis, irrigation of the bladder, mesna
Veno-occlusive Renal Disease
- clinical features: day 10-21 post transplant, hepatorenal syndrome
- risk factors: mismatched graft, age > 25 years, pre-existing renal failure, sepsis, amphotericin B
Drug Nephrotoxicity
- cyclosporine A: intensive renal arteriolar vasoconstriction
- nitrourea
- methotrexate
- cyclophosphamide
- amphotericin B
- acyclovir
- foscanet
- aminoglycosides
- tacrolimus
INFECTIOUS COMPLICATIONS
Viral
- CMV: pneumonitis is the most lethal -> ganciclovir/foscarnet, Ig’s
- RSV: URTI -> LRTI -> nasal wash/BAL, aerosolized ribavirin, Ig’s
- HSV-6: pneumonitis, marrow suppression, encephalitis -> ganciclovir/foscarnet
- HZV: pneumonia, hepatitis, skin rash, encephalitis, DIC -> high dose acyclovir
Bacterial
- risk factors: neutropenia, mucositis, skin breakdown, GI problems, IV catheters
- organisms: gram negatives (Pseudomonas, Klebsiella), gram positives (MRSA, Strep viridans, enterococci)
Fungal
- invasive pulmonary aspergillus: lungs to haematogenous dissemination -> CXR: halo sign and air crescent sign, sputum, BAL, voriconazole/caspofungin
- candida: fluconazole or caspofungin (evidence of endophthalmitis or resistant organisms)
- PCP: rare now c/o co-trimoxazole prophylaxis -> requires a BAL
SUMMARY
Acute (< 30 days)
- neutropenia
- acute tumour lysis
- infection: bacterial, fungal and viral
- respiratory: engraftment, haemorrhage
- cardiovascular: CHF, arrhythmias, tamponade
- gastrointestinal: GIH, enteritis, veno-occlusive disease of liver
- nervous: CVA, encephalopathy
- other: haemorrhagic cystitis
Early (30-100 days)
- acute GVHD
- graft failure
- pneumonitis
- BOOP
- infection: bacterial, viral, fungi
Late (>100 days)
- chronic GVHD
- myopathy
- neuropathy
- HUS
- infection: CMV
- infertility
- second malignancy
- cataracts
PROGNOSIS
- critical illness during engraftment period (< 30 days post BMT) -> mortality 33%
- acute GVHD (moderate to severe) -> mortality 90%
- more than two organ systems and need for mechanical ventilation/RRT are associated with very poor outcome
References and Links
LITFL
- Paul Young’s ICU Mind Maps — Bone Marrow Transplant – Cardiac
- Paul Young’s ICU Mind Maps — Bone Marrow Transplant – Complications
- Paul Young’s ICU Mind Maps — Bone Marrow Transplant – Gastrointestinal
- Paul Young’s ICU Mind Maps — Bone Marrow Transplant – Infections
- Paul Young’s ICU Mind Maps — Bone Marrow Transplant – Neurological
- Paul Young’s ICU Mind Maps — Bone Marrow Transplant – Renal

Critical Care
Compendium
Chris is an Intensivist and ECMO specialist at The Alfred ICU, where he is Deputy Director (Education). He is a Clinical Adjunct Associate Professor at Monash University, the Lead for the Clinician Educator Incubator programme, and a CICM First Part Examiner.
He is an internationally recognised Clinician Educator with a passion for helping clinicians learn and for improving the clinical performance of individuals and collectives. He was one of the founders of the FOAM movement (Free Open-Access Medical education) has been recognised for his contributions to education with awards from ANZICS, ANZAHPE, and ACEM.
His one great achievement is being the father of three amazing children.
On Bluesky, he is @precordialthump.bsky.social and on the site that Elon has screwed up, he is @precordialthump.
| INTENSIVE | RAGE | Resuscitology | SMACC