CT Case 100
A 54-year-old lady with end stage renal failure (ERSF) presents to the the emergency department with abdominal pain.
She has missed haemodialysis for the last week as she was feeling too unwell to attend.
Her past medical history includes severe LV dysfunction (with PPM), ventricular tachycardia, and superior mesenteric artery (SMA) stenosis secondary to calcification.
Her ECG at the time of presentation is shown below
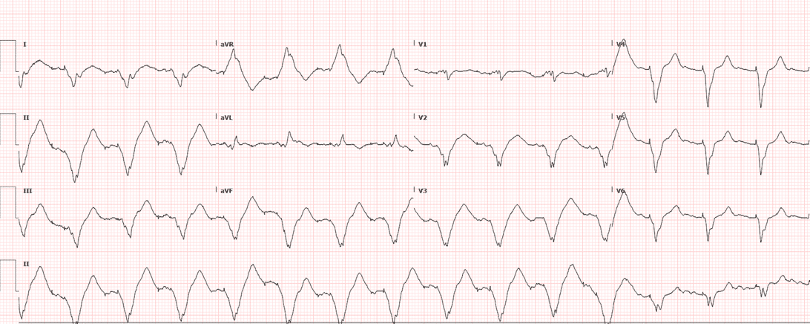
There was a delay getting CT imaging due hyperkalaemia associated with hypotension.
Following aggressive treatment of hyperkalaemia, her QRS narrowed and her haemodynamics improved enough to safely go to CT.
CT abdomen
Describe and interpret the CT scan
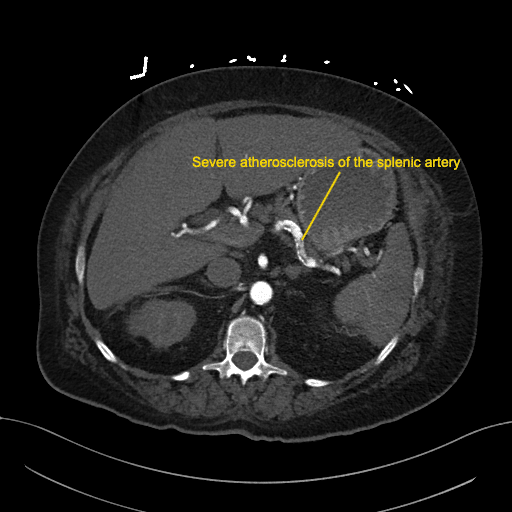
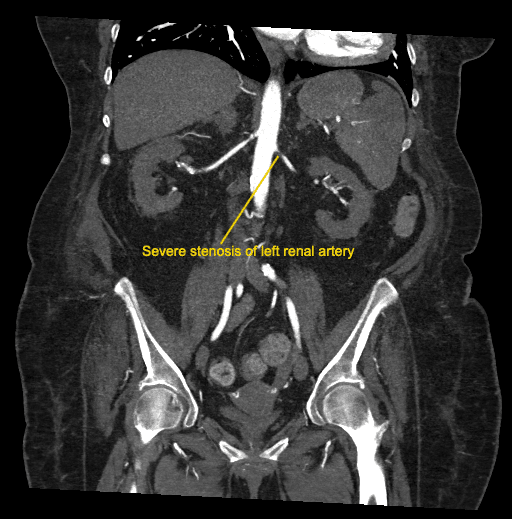
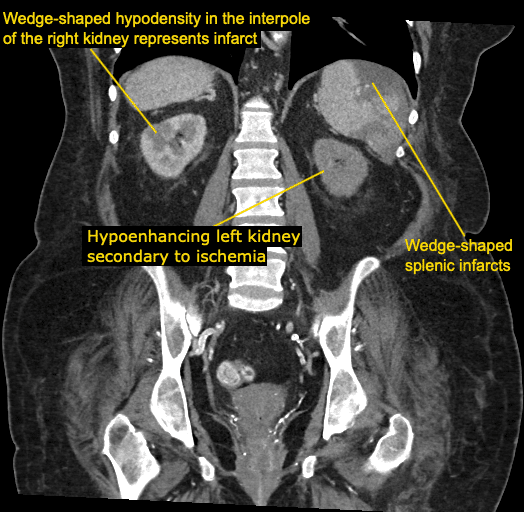
There is severe atherosclerosis of the splenic artery and the left renal artery.
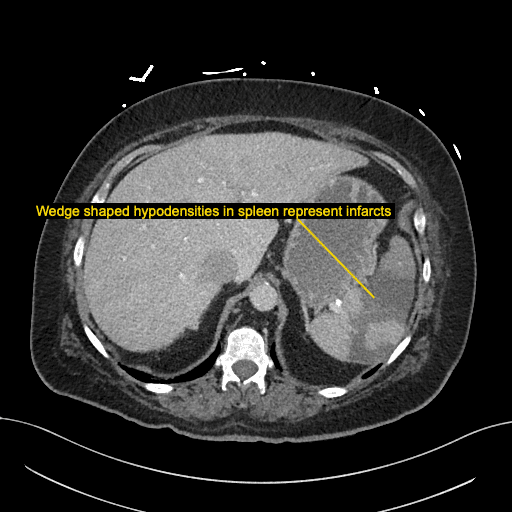
There is diffuse left kidney infarction as well as extensive wedge-shaped splenic infarction.
There is also a wedge shaped hypodensity in the interpole (middle portion) of right kidney due to infarct.
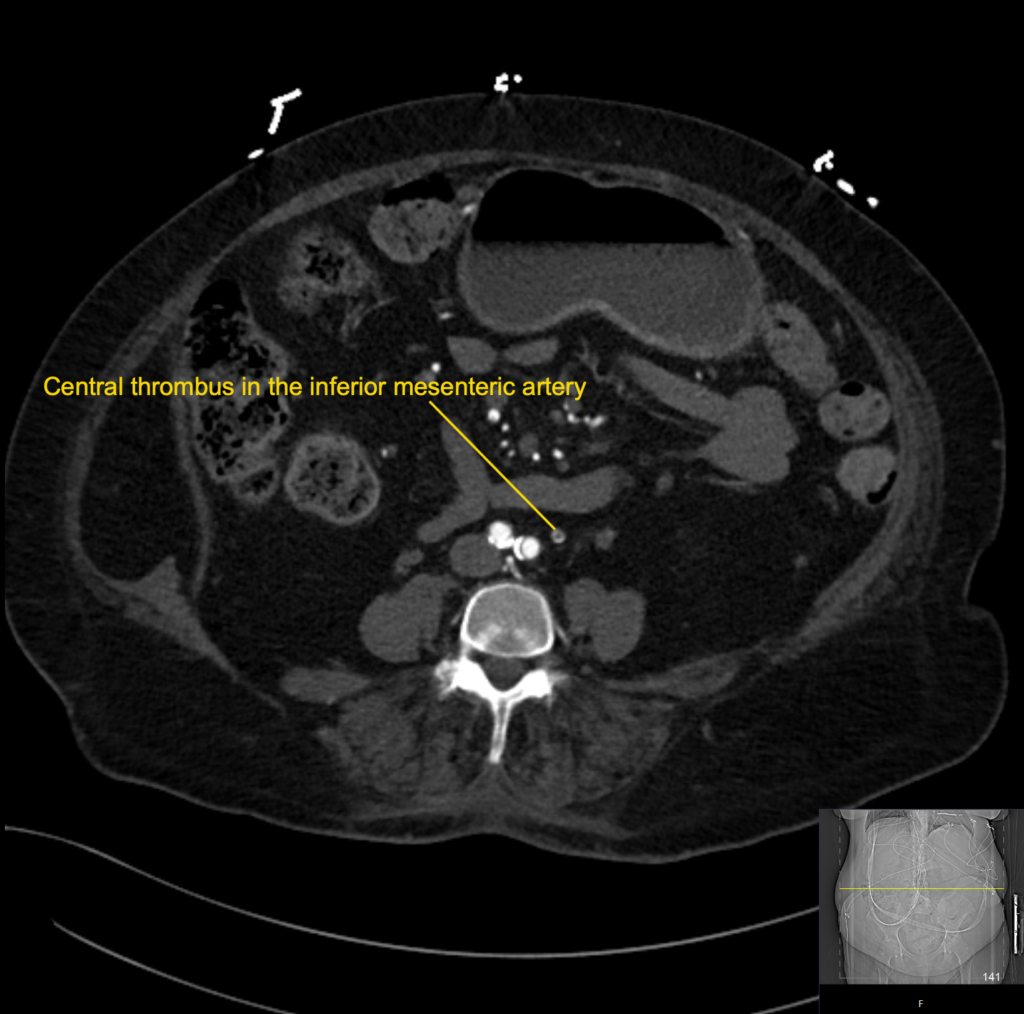
There is a short segment of central occlusion of the IMA. There are multiple thrombi within all branches of the coeliac trunk.
Clinical Pearls
Splenic infarction occurs when blood supply to the spleen is compromised, it can be related to arterial or venous obstruction resulting in necrosis.
The two most common causes are thromboembolic or infiltrative haematological disease.
Causes can be classified as;
- Hypercoagulable states; pregnancy, malignancy, sickle cell disease
- Thromboembolic; AF, endocarditis, prosthetic heart valves
- Blood borne malignancies; leukaemia, lymphoma, myelofibrosis
- Blunt abdominal trauma
- Pancreatic disorders; pancreatitis, compressive mass
Treatment of splenic infarcts is based on identifying and treating the underlying disease.
Concerning complications of splenic infarct include aneurysm, splenic rupture, pseudocyst formation and abscess.
Abdominal pain due to uncomplicated splenic infarction will resolve within 7 to 10 days.
This patient’s condition was incredibly difficult to manage.
She had diffuse atherosclerotic disease (with known SMA, and now IMA disease) and subsequent complications with renal and splenic infarction despite therapeutic anticoagulation, there was also presumed intestinal ischaemia.
This patient was admitted to the ICU for haemodialysis and monitoring.
The vascular team felt there were no endovascular therapeutic options and unfortunately it is anticipated that she may experience further intestinal ischaemia, exacerbated by haemodialysis.
She is currently being worked up for other possible embolic sources.
References
- Chapman J, Helm TA, Kahwaji CI. Splenic Infarcts. Stat Pearls
TOP 100 CT SERIES
Dr Leon Lam FRANZCR MBBS BSci(Med). Clinical Radiologist and Senior Staff Specialist at Liverpool Hospital, Sydney
Sydney-based Emergency Physician (MBBS, FACEM) working at Liverpool Hospital. Passionate about education, trainees and travel. Special interests include radiology, orthopaedics and trauma. Creator of the Sydney Emergency XRay interpretation day (SEXI).
Provisional fellow in emergency radiology, Liverpool hospital, Sydney. Other areas of interest include paediatric and cardiac imaging.
Emergency Medicine Education Fellow at Liverpool Hospital NSW. MBBS (Hons) Monash University. Interests in indigenous health and medical education. When not in the emergency department, can most likely be found running up some mountain training for the next ultramarathon.









