ECG Case 120
A 75-year-old woman with a background of stage 3 CKD, Type 2 diabetes and hypertension presents to the emergency department with a 12-hour history of diarrhoea and vomiting. She suffers a PEA arrest shortly after arrival and receives 2 minutes of CPR.
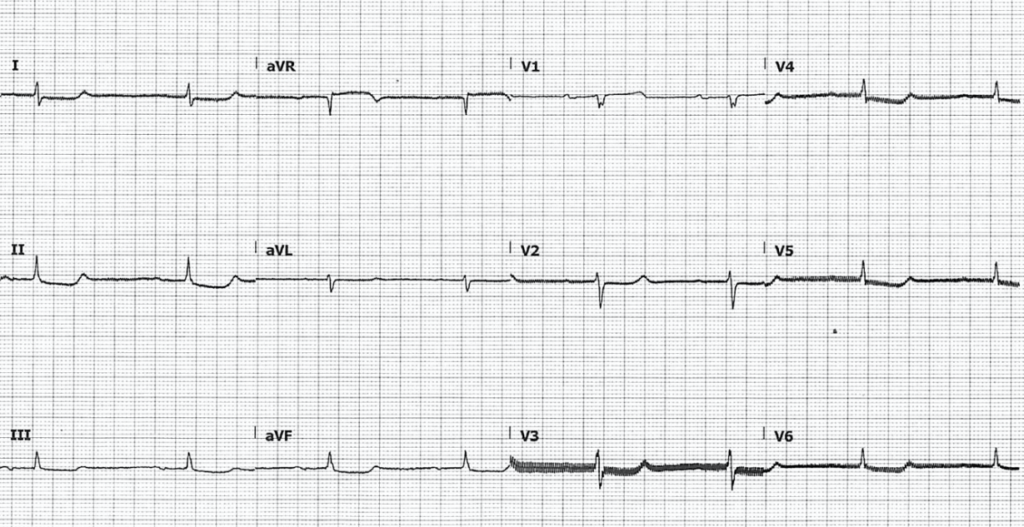
Her post-ROSC ECG is below:
Describe and interpret this ECG
ECG ANSWER and INTERPRETATION
- Sinus bradycardia, rate 44
- Normal axis
- PR interval is significantly prolonged at 330ms
- Normal width QRS
- There are non-specific ST segment abnormalities, most prominent in inferolateral leads
- QTC is normal at approximately 420ms
What are some potential causes of this rhythm?
Reveal answer
Sinus bradycardia in the unwell patient is most commonly due to:
- Inferior myocardial infarction
- Electrolyte abnormalities (K, Mg)
- AV-nodal blocking agents including beta-blockers, calcium-channel blockers, digoxin
- Raised intracranial pressure
The patient was found to have a K of 7.8. Her regular medications include atenolol, candesartan, metformin and gliclazide.
What is the diagnosis?
Reveal answer
This patient was suffering from BRASH syndrome:
- Bradycardia
- Renal failure
- AV-nodal blockade
- Shock
- Hyperkalaemia
Due to synergism from AV-nodal blocking medications, these patients may have significant hyperkalaemia without other typical associated ECG features such as QRS prolongation and T-wave abnormalities.
PATHOPHYSIOLOGY
BRASH syndrome occurs due to a cyclical interplay between AV-nodal blocking drugs and hypoperfusion:
- Hyperkalaemia and AV-nodal blocking medications cause bradycardia
- Bradycardia subsequently reduces cardiac output, which impairs renal perfusion, causing acute kidney injury
- Renal failure exacerbates hyperkalaemia, and elevates serum levels of medications that undergo renal excretion such as beta-blockers
In most published case reports the initial trigger is a mild clinical event such as dehydration. Some patients present with a normal blood pressure despite severe bradycardia, compensating with a pronounced vasoconstrictive response, which causes further renal hypoperfusion.
For an in-depth review of the pathophysiology and management of BRASH syndrome, see this excellent article by Josh Farkas.
CLINICAL PEARLS
Hyperkalaemia and sinus bradycardia without other typical ECG features of hyperkalaemia should raise suspicion for BRASH syndrome and prompt correction of underlying triggers such as hypovolaemia.
These cases are refractory to treatment of hyperkalaemia alone. Patients may require haemodynamic support in the form of vasopressors and/or pacing until accumulated drug effect has been eliminated.
- Patients with BRASH syndrome may not exhibit the typical ECG findings of hyperkalaemia beyond bradycardia
- Always suspect hyperkalaemia in any patient with profound bradycardia
Further reading
Related topics
Expert Review
- Smith SW. Bradycardia, SOB, in a dialysis patient. Dr Smith’s ECG Blog. 2014
- Farkas J. PulmCrit – BRASH syndrome: Bradycardia, Renal failure, AV blocker, Shock, Hyperkalaemia. 2016
References
- Lee TH et al. Hypotension and sinus arrest with exercise-induced hyperkalaemia and combined verapamil/propranolol therapy. Am J Med. 1986 Jun;80(6):1203-4
- Mohanlal V, Haririan A, Weinman EJ, et al. Bradycardia without “classical” EKG changes in hyperkalemic hemodialysis patients. Clin Nephrol. 2013;80(6):464–8.
- Golchin K, Zhou M, Khan AH. Bradycardia, renal failure, AV-nodal blockers, shock, and hyperkalemia (BRASH) – a new clinical syndrome. Am J Respir Crit Care Med. 2018;197
TOP 150 ECG Series
MBBS DDU (Emergency) CCPU. Adult/Paediatric Emergency Medicine Advanced Trainee in Melbourne, Australia. Special interests in diagnostic and procedural ultrasound, medical education, and ECG interpretation. Co-creator of the LITFL ECG Library. Twitter: @rob_buttner