ECG Case 119
A 34 year-old male presents to your emergency department with palpitations. His vitals checked at triage include pulse >170; BP 112/76; sO2 98%; GCS 15
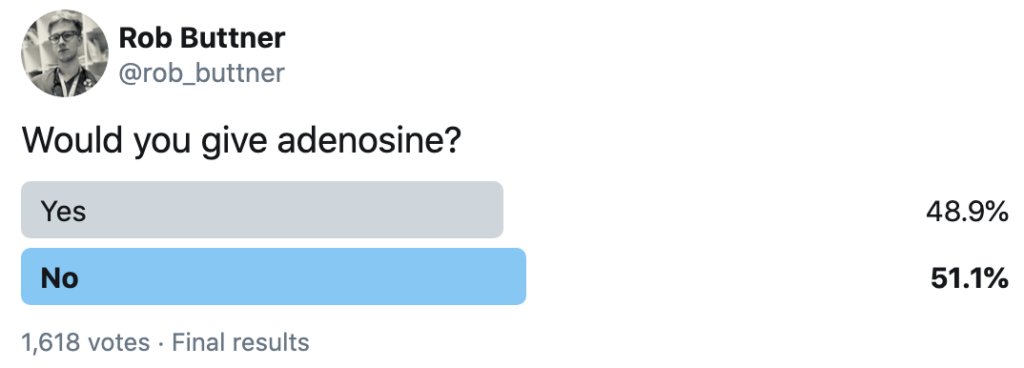
Would you give adenosine?
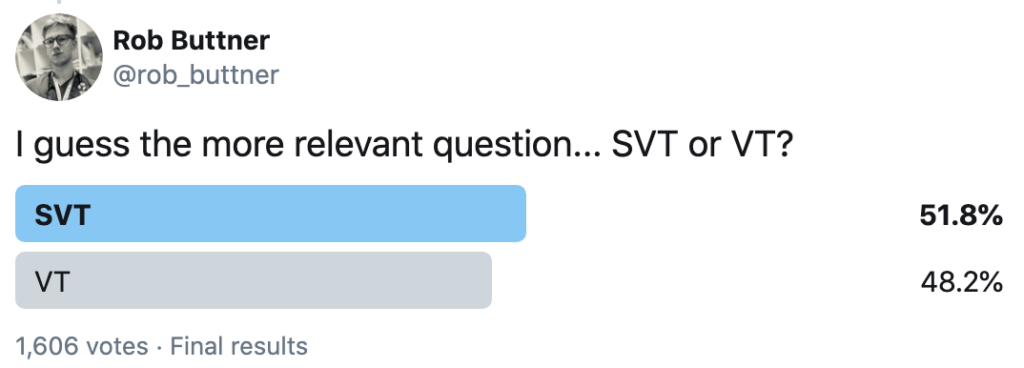
We presented the ECG to the medical Twitter community and asked what they would do, and what was the most likely ECG diagnosis:
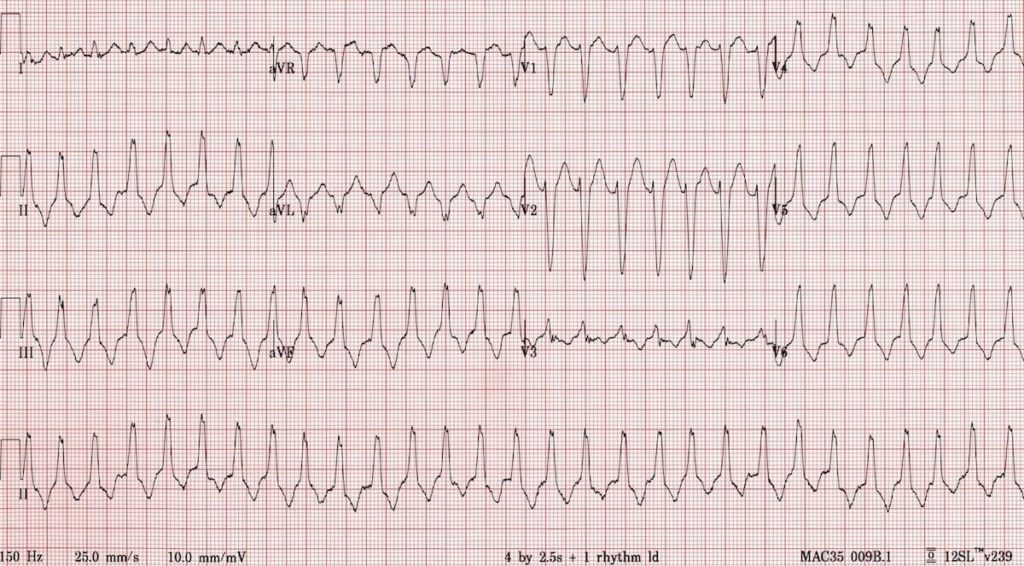
Describe and interpret this ECG
ECG ANSWER and INTERPRETATION
On first glance this may appear to be SVT with LBBB as there is:
- Regular broad-complex tachycardia, rate 174
- Typical LBBB morphology in aVR, V1 and V6
- Absence of fusion or capture beats
However, there is one feature here that is unusual for LBBB, can you spot it?
Reveal answer
There is an inferior axis (+90 degrees), which is atypical for LBBB. LBBB normally has a leftward axis.
The combination of a regular broad complex tachycardia with typical LBBB morphology, and inferior axis (+90 degrees), should raise suspicion for a form of monomorphic VT known as right ventricular outflow-tract tachycardia (RVOT tachycardia).
In addition, there are other features suggestive of VT, can you spot them?
Pathophysiology
The differential diagnosis of a regular broad complex tachycardia is VT versus SVT with aberrant conduction (due to bundle branch block or Wolff-Parkinson-White Syndrome). For an in-depth review of differentiating between the two, see VT versus SVT.
RVOT tachycardia is a form of monomorphic VT originating from the outflow tract of the right ventricle or occasionally from the tricuspid annulus. It is most commonly a form of idiopathic VT, whereby no structural heart disease, metabolic/electrolyte abnormalities, or long QT syndrome can be found. It can also be seen in patients with Arrhythmogenic Right Ventricular Dysplasia (ARVD).
The RVOT is divided into rightward (free wall), anterior, leftward, and posterior (septal) parts. RVOT tachycardia can originate from any of these sites but all carry common ECG characteristics.
ECG features of RVOT VT:
- LBBB morphology
- Inferior axis
- rS complex in V1 and R complex in V6
- Precordial transition usually ≥ V3, with the exception of septal origin, which occurs at ≤ V3
Other general features of VT, such as AV dissociation, fusion and/or capture beats may also be present.
Back to our initial question: Would you give adenosine?
If the patient is stable, you can administer adenosine…
- Acute termination of idiopathic RVOT VT in a stable patient can be achieved by vagal manoeuvres or adenosine (6mg up to 24mg)
- IV verapamil is an alternative if the patient has adequate blood pressure
- DCCV is always the management preference if there is haemodynamic instability.
RVOT tachycardia in ARVD generally does not terminate with adenosine. Differentiation between idiopathic RVOT tachycardia and that caused by ARVD can be difficult and may rely on previous ECG findings as well as family history. In ARVD, the baseline ECG usually shows inverted T waves in right precordial leads, and when present, RV conduction delay with an epsilon wave best seen in V1-2.
What if there was still uncertainty regarding the rhythm?
In stable patients with a regular broad complex tachycardia, adenosine is useful and safe as a diagnostic and potentially therapeutic agent.
In unstable patients, if there is doubt regarding the rhythm (SVT v VT), proceed to DCCV.
FURTHER READING
Related topics
- VT versus SVT
- RVOT Tachycardia
- Arrhythmogenic Right Ventricular Dysplasia (ARVD)
- Supraventricular Tachycardia (SVT)
References
- Corrado D et al. Three-dimensional electroanatomical voltage mapping and histologic evaluation of myocardial substrate in right ventricular outflow tract tachycardia. J Am Coll Cardiol 2008;51:731–739.
- Jadonath RL, Schwartzman DS, Preminger MW, Gottlieb CD, Marchlinski FE. Utility of the 12-lead electrocardiogram in localizing the origin of right ventricular outflow tract tachycardia. Am Heart J. 1995; 130:1107–1113.
- Josephson ME, Horowitz LN, Waxman HL, Cain ME, Spielman SR, Greenspan AM, Marchlinski FE, Ezri MD. Sustained ventricular tachycardia: role of the 12-lead electrocardiogram in localizing site of origin. Circulation. 1981; 64:257–272.
- Joshi S, Wilber DJ. Ablation of idiopathic right ventricular outflow tract tachycardia: current perspectives. J Cardiovasc Electrophysiol. 2005; 16(suppl 1):S52–S58. DOI: 10.1111/j.1540-8167.2005.50163.
- Timmermans C, Rodriguez LM, Medeiros A, Crijns HJ, Wellens HJ. Radiofrequency catheter ablation of idiopathic ventricular tachycardia originating in the main stem of the pulmonary artery. J Cardiovasc Electrophysiol. 2002; 13:281–284.
- Tada H, Kurosaki K, Ito S, Naito S, Yamada M, Miyaji K, Hashimoto T, Oshima S, Nogami A, Taniguchi K. Idiopathic premature ventricular contractions arising from the pulmonary artery: importance of mapping in the pulmonary artery in left bundle branch block-shaped ventricular arrhythmias. Circ J. 2005; 69:865–869.
- Sekiguchi Y, Aonuma K, Takahashi A, Yamauchi Y, Hachiya H, Yokoyama Y, Iesaka Y, Isobe M. Electrocardiographic and electrophysiologic characteristics of ventricular tachycardia originating within the pulmonary artery. J Am Coll Cardiol. 2005; 45:887–895. DOI: 10.1016/j.jacc.2004.10.071
- Dixit S, Gerstenfeld EP, Callans DJ, Marchlinski FE. Electrocardiographic patterns of superior right ventricular outflow tract tachycardias: distinguishing septal and free-wall sites of origin. J Cardiovasc Electrophysiol. 2003; 14:1–7.
- Yamada T, McElderry HT, Doppalapudi H, Kay GN. Catheter ablation of ventricular arrhythmias originating in the vicinity of the His bundle: significance of mapping the aortic sinus cusp. Heart Rhythm. 2008; 5:37–42. DOI: 10.1016/j.hrthm.2007.08.032
- Yamauchi Y, Aonuma K, Takahashi A, Sekiguchi Y, Hachiya H, Yokoyama Y, Kumagai K, Nogami A, Iesaka Y, Isobe M. Electrocardiographic characteristics of repetitive monomorphic right ventricular tachycardia originating near the His-bundle. J Cardiovasc Electrophysiol. 2005; 16:1041–1048. DOI: 10.1111/j.1540-8167.2005.40787.
- Marill KA et al. Adenosine for wide-complex tachycardia: Efficacy and safety. 2009; Critical Care Medicine 37(9):2512-
TOP 150 ECG Series
MBBS DDU (Emergency) CCPU. Adult/Paediatric Emergency Medicine Advanced Trainee in Melbourne, Australia. Special interests in diagnostic and procedural ultrasound, medical education, and ECG interpretation. Co-creator of the LITFL ECG Library. Twitter: @rob_buttner
Dr Tom Cassidy MBBS FACEM. Emergency physician, Perth Australia. Father of two humans and whimsical lyricist. Special skills: relocating ECGs, reading toxidromes and interpreting dislocations | @tgpcassidy | LinkedIn |