Hyperammoniacal Encephalopathy
aka Pediatric Perplexity 001
A 7 year-old girl was brought to hospital with sudden onset vomiting followed by lethargy and irritability. A week previously she developed chicken pox and was recovering well, having been treated with regular aspirin and paracetamol for fever and discomfort.
There is no history of any other drug or toxin exposure and no family history of childhood diseases. When you review her she is afebrile, anicteric, drowsy and mildly dehydrated. She has mild hepatomegaly on palpation. She has no focal neurological deficits.
Relevant findings on her investigations include:
- Lumbar puncture — CSF essentially normal (WBC 2 x 109/L)
- CT head — suspicious for mild cerebral edema
- Metabolic screen — no evidence of any inborn error of metabolism (IEM), normal urinary copper excretion
- Blood tests — hyperammonaemia (NH3 210 micromol/L) and abnormal LFTs (ALT 1150 IU/L). An initial mild hypoglycemia was corrected with glucose administration.
Questions
Q1. What is the likely diagnosis?
Answer and interpretation
Reye syndrome
Reye syndrome is an acute metabolic encephalopathy associated with hepatic dysfunction characterized by ‘fatty metamorphosis’.
It was named after the Australian doctor [Ralph Douglas Kenneth Reye (1912-1977)] who described it in 1963 and has a mortality rate of about 20-40%.
It is has been an extremely rare diagnosis since the 1980s.
The disappearance of Reye Syndrome is attributed to our increased ability to diagnose IEMs that cause Reye-like syndromes and successful public health campaigns to stop the use of aspirin in children with febrile illnesses. Reye syndrome hardly ever affects adults.
Q2. What are the CDC diagnostic criteria for this condition?
Answer and interpretation
The CDC 1990 clinical case definition for Reye Syndrome is ‘an illness that meets all of the following criteria‘:
- Acute, noninflammatory encephalopathy that is documented clinically by:
- an alteration in consciousness and, if available,
- a record of the CSF containing less than or equal to 8 leukocytes/cu.mm or a histologic specimen demonstrating cerebral edema without perivascular or meningeal inflammation
- Hepatopathy documented by either:
- a liver biopsy or an autopsy considered to be diagnostic of Reye syndrome or
- a threefold or greater increase in the levels of the serum glutamic-oxaloacetic transaminase (SGOT), serum glutamic-pyruvic transaminase (SGPT), or serum ammonia
- No more reasonable explanation for the cerebral and hepatic abnormalities
Q3. What are the clinical features of this condition?
Answer and interpretation
Findings on the history include:
- Recent viral illness or vaccination:
- especially influenza A or B, and varicella zoster (chicken pox)
- Recent salicylate use (e.g. aspirin):
- over 80% of cases report aspirin use in the previous 3wks
- Vomiting:
- often with an abrupt onset within few days (12h to 3 weeks) of the resolution of the viral illness
- Neurological symptoms
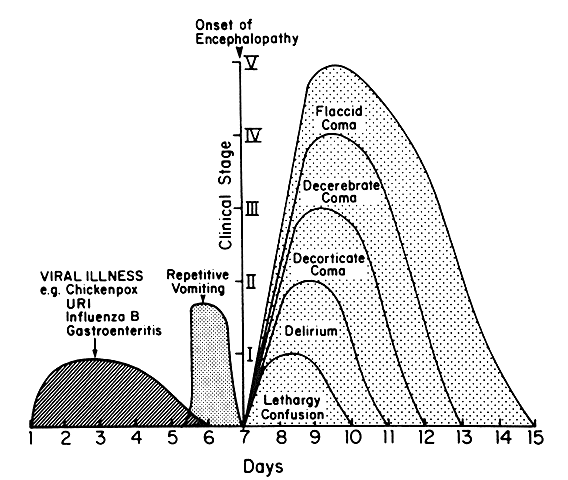
- Onset heralded by repetitive vomitingLethargy, irritability, restlessness, delirium, seizures, loss of brainstem reflexes, decorticate or decrebrate coma and flaccid paralysis.
Findings on physical examination include:
- Protracted vomiting ± dehydration
- Afebrile with encephalopathy (see neurological symptoms)
- hepatomegaly (~50%) but with minimal or absent jaundice
The severity of Reye syndrome is described using a 6 stage classification ranging from 0 (alert, wakeful) to V (flaccid non-responsive coma).
Q4. What is the cause of this condition? How is aspirin involved?
Answer and interpretation
The exact mechanisms leading to Reye syndrome are obscure.
It is thought to result when a sensitized virus-infected host is exposed to an agent that causes mitochondrial dysfunction.
This combination of insults leads to inhibition of oxidative phosphorylation and fatty-acid beta-oxidation and the resulting metabolic derangement manifests as neurological and hepatic dysfunction. The most important precipitating agents is thought to be:
Aspirin (and other salicylates)
The actions of the CDC and FDA in the early 1980’s led to the widespread banishment of aspirin from general use in children. Some experts still question whether aspirin has a causal role in the disorder as not every case of Reye syndrome involves aspirin exposure and only about about 1/1000 children using aspirin get the disorder. In my view, however, the relative disappearance of this terrible disease since the discontinuation of widespread aspirin use in children should not be trivialized. Other drugs and toxins might also act as triggers of mitochondrial dysfunction — paracetamol, valproate, and antiemetics have all been cited as potential culprits.
Q5. Describe appropriate management of this child?
Answer and interpretation
There is no specific treatment for Reye syndrome.
Standard supportive care and monitoring should be provided, generally in an ICU-level setting.
- Attend to ABCs
- Treat hypoglycemia
- Treat seizures — e.g. benzodiapines, phenytoin
- Treat vomiting — antiemetics e.g. ondansetron
- Appropriate fluid management
- Correct hyperammonaemia
- Consider use of ammonia detoxicants (sodium phenylacetate and sodium benzoate) that prevent ammonia production from glycine and glutamine.
- Prevent and treat raised intracranial pressure
- Treat severe metabolic acidosis
- Correct coagulopathy
- Prevent and treat other potential causes and complications, e.g. sepsis, multiple organ dysfunction syndrome (MODS), SIADH, diabetes insipidus.
References
- Ralph Douglas Kenneth Reye (1912-1977)
- Reye Syndrome – LITFL
- Reye RD, Morgan G, Baral J. Encephalopathy and fatty degeneration of the viscera. A Disease entity in childhood. Lancet. 1963; 2(7311):749–752. [PMID 14055046]
- Sarnaik AP. Reye’s syndrome: hold the obituary. Critical care medicine. 1999; 27(8): 1674-6 PMID: 10470794
- Schror K. Aspirin and Reye syndrome: a review of the evidence. Paediatric drugs. 2007; 9(3), 195-204 PMID: 17523700
- Glasgow JF, & Middleton B. Reye syndrome — insights on causation and prognosis. Archives of disease in childhood. 2001; 85(5): 351-3 PMID: 11668090

CLINICAL CASES
Paediatric Perplexity
Chris is an Intensivist and ECMO specialist at The Alfred ICU, where he is Deputy Director (Education). He is a Clinical Adjunct Associate Professor at Monash University, the Lead for the Clinician Educator Incubator programme, and a CICM First Part Examiner.
He is an internationally recognised Clinician Educator with a passion for helping clinicians learn and for improving the clinical performance of individuals and collectives. He was one of the founders of the FOAM movement (Free Open-Access Medical education) has been recognised for his contributions to education with awards from ANZICS, ANZAHPE, and ACEM.
His one great achievement is being the father of three amazing children.
On Bluesky, he is @precordialthump.bsky.social and on the site that Elon has screwed up, he is @precordialthump.
| INTENSIVE | RAGE | Resuscitology | SMACC