Janeway lesions
Janeway lesions are small nontender, erythematous or hemorrhagic macules typically located on the palms and soles; associated with acute infective endocarditis. Unlike Osler nodes (which are tender), Janeway lesions are characteristically painless and blanching.

Janeway lesions are classically described as painless, erythematous or hemorrhagic macular lesions found on the palms and soles, particularly on the thenar and hypothenar eminences. They are a cutaneous manifestation of infective endocarditis (IE), most often seen in acute forms of the disease and associated with septic microemboli. Though uncommon, their presence holds significant diagnostic and prognostic value, included as minor criteria in the modified Duke Criteria for endocarditis.
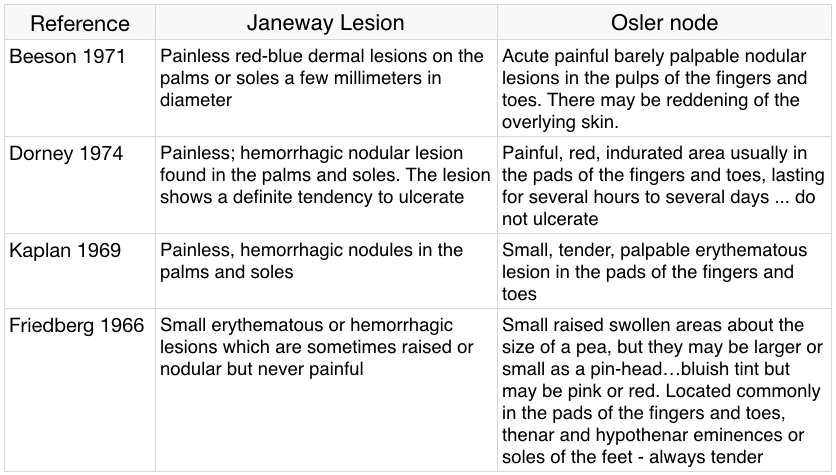
Histologically, Janeway lesions demonstrate neutrophilic dermal microabscesses, often with bacterial culture positivity, supporting an embolic aetiology. They contrast clinically with Osler nodes, which are typically painful and immunologically mediated. However, recent studies highlight histologic overlap between the two, suggesting a possible spectrum of cutaneous septic embolism.
Named after Edward G. Janeway (1841–1911), an American physician noted for his diagnostic acumen, the lesion’s eponym acknowledges his early clinical descriptions of non-tender petechial and nodular lesions on the hands and feet in patients with acute ulcerative endocarditis. Janeway’s observations predated Sir William Osler (1849-1919) popularization of endocarditis skin signs and were grounded in his 1882 and 1899 publications linking cerebral embolism, petechiae, and valvular heart disease.

History of the Janeway lesion
1882 – E. G. Janeway described acute ulcerative endocarditis as mimicking both brain disease and typhoid fever in his paper “Cases Bearing on the Diagnosis, and Localization of Cerebral Diseases, and Their Difficulties“. He noted that embolic fragments from heart valve vegetations could lodge in the brain or skin, causing petechiae and neurologic symptoms such as hemiplegia or aphasia.
We have in this, as you know, the development of soft masses on the heart-valves, which as a rule are ulcerated, and then the little fragments from these pass as emboli to the different organs, giving rise in the skin to petechias from the obstruction of small arteries
1899 – Janeway described the lesion in the context of separating “malignant” (acute) endocarditis from other infectious disorders
In trying to determine whether a given case is more probably due to endocarditis or to another malignant process I have found that attention to the position of the hemorrhages is at times very helpful. Several times I have noted numerous small hemorrhages with slight nodular character in the palms of the hand and soles of the feet, when possibly the arms and legs had but a scanty crop in malignant endocarditis, whereas this has not been my experience with processes likely to be mistaken for it.
1906 – Emanuel Libman (1872-1946), a student of Janeway, applied the eponym ‘Janeway lesion’. Libman pointed out that these lesions were not tender, in contrast to the exquisitely painful Osler node.
I would like to refer to a point which has been of great value… “the small hemorrhages in the palms and soles with slightly nodular character” I learned from Dr. Janeway when I had the privilege of serving under him…(keep) a sharp lookout for them as they will often direct attention to an acute endocarditis to which there was no other clue.
1912 – Sir William Osler (1849-1919) recorded lesions that may well have been Janeway lesions. He described the lesions as “peculiar areas of persistent erythema” on the palms and soles in a patient with subacute bacterial endocarditis [1912; 19: 103-107]. These were in stark contrast to the painful erythematous nodules he associated with infectious endocarditis that were later termed Osler nodes.
1923 – Libman originally considered Janeway lesions to be pathognomonic for acute bacterial endocarditis but later remarked that he had also seen them in three patients with subacute bacterial endocarditis.
Embolic lesions occur with great frequency in the acute and subacute bacterial cases. They consist of petechiae, Janeway lesions, Osler (tender cutaneous) nodes and purpura
1949 – Libman and Friedberg emphasized the fact that Janeway lesions were infrequent; more characteristic of acute bacterial endocarditis than subacute bacterial endocarditis; and were never painful. They noted that Janeway lesions may appear erythematous, rather than haemorrhagic, particularly in subacute bacterial endocarditis
1976 – Joseph B. Farrior, III evaluation of ‘classic‘ textbook descriptions of Janeway lesions and Osler nodes
1990 – Cardullo et al. publish a histopathologic review showing that both Janeway lesions and Osler nodes contain neutrophilic dermal abscesses, sometimes with bacteria, challenging the strict embolic–immunologic divide.
2014 – Servy et al. show that cutaneous manifestations in IE, including Janeway lesions, are associated with higher rates of systemic embolism and in-hospital complications.
2017 – Misin et al. document Janeway lesions in a patient with Staph aureus aortic endocarditis, reinforcing their diagnostic specificity and value in early clinical suspicion.
2024 – Wijdicks EF publishes a historical review affirming Janeway’s priority in naming and description, highlighting his neurological focus and underappreciated role in early endocarditis recognition.
Associated Persons
- Edward Gamaliel Janeway (1841-1911) [Janeway lesion]
- Emanuel Libman (1872-1946)
- Sir William Osler (1849-1919) [Osler nodes]
References
Original articles
- Janeway EG. Certain clinical observations upon heart disease. Medical News. 1899; 75: 257-262
- Libman E. On some experiences with blood cultures in the study of bacterial infection. Johns Hopkins Hospital Bulletin. 1906; 17: 215-228
- Osler W. Chronic infectious endocarditis with an early history like splenic anemia. Interstate Medical Journal 1912; 19: 103-107
- Libman E. The clinical features of subacute streptococcal (and influenzal) endocarditis in the bacterial stage. Medical Clinics of North America 1918; 2(1): 117-152
- Libman E. Characterization of various forms of endocarditis. JAMA 1923; 80: 813-818
Review articles
- Farrior JB, Silverman ME. A consideration of the differences between a Janeway’s lesion and an Osler’s node in infectious endocarditis. Chest. 1976 Aug;70(2):239-43.
- Cardullo AC, Silvers DN, Grossman ME. Janeway lesions and Osler’s nodes: a review of histopathologic findings. J Am Acad Dermatol. 1990 Jun;22(6 Pt 1):1088-90.
- Marrie TJ. Osler’s nodes and Janeway lesions. Am J Med. 2008 Feb;121(2):105-6
- Sethi K, Buckley J, de Wolff J. Splinter haemorrhages, Osler’s nodes, Janeway lesions and Roth spots: the peripheral stigmata of endocarditis. Br J Hosp Med (Lond). 2013 Sep;74(9):C139-42.
- Servy A et al; Association Pour l’Etude et la Prévention de l’Endocardite Infectieuse Study Group. Prognostic value of skin manifestations of infective endocarditis. JAMA Dermatol. 2014 May;150(5):494-500.
- Misin A, Di Bella S, Priolo L, Luzzati R. Image of the month: ‘Diagnostic hands’: Janeway lesions. Clin Med (Lond). 2017 Jul;17(4):373-374
- Panginikkod S, Gopalakrishnan V, Parikh M, Gupta N. Janeway Lesions: a Painless Manifestation of Infective Endocarditis. J Gen Intern Med. 2019 Jul;34(7):1360-1361.
- Parashar K, Daveluy S. Osler Node and Janeway Lesions. 2023 Jul 24. In: StatPearls
- Wijdicks EFM. Janeway and His Neurology of Acute Infectious Disease. Neurocrit Care. 2024 Jan 26.
eponymictionary
the names behind the name
Doctor in Australia. Keen interest in internal medicine, medical education, and medical history.
