Neuro 101: Peripheral Nervous System
The peripheral nervous system (PNS) connects the central nervous system (CNS) to the limbs and organs, enabling voluntary movement, sensation, and autonomic function. Disorders of the PNS can result in characteristic patterns of weakness, sensory loss, and reflex changes that assist with lesion localisation.
In this section, we will cover the anatomy of the peripheral nervous system, localisation of nerve injuries, pathology affecting peripheral nerves, the brachial and lumbosacral plexuses, peripheral nerve examination, common peripheral neuropathies, and diseases affecting the neuromuscular junction.
Function
The peripheral nervous system transmits motor, sensory, and autonomic signals between the CNS and the body. Peripheral nerves are made up of a mix of sensory and motor fibers, which are derived from several spinal roots via the plexuses.
- Conducts efferent (motor) output from the CNS to muscles and glands
- Conducts afferent (sensory) input from the periphery to the CNS
- Mediates reflexes in conjunction with spinal circuits
Pathology of nerves can involve the destruction of axons, or the deterioration of the myelin coatings.
Pathology
Anatomy
- Connection to the CNS occurs at the nerve root level
- Nerve roots form plexuses where motor and sensory fibres mix before forming peripheral nerves
- Peripheral nerves consist of mixed motor and sensory fibres derived from several spinal roots
- Axons may be myelinated or unmyelinated; pathology may affect axons or myelin
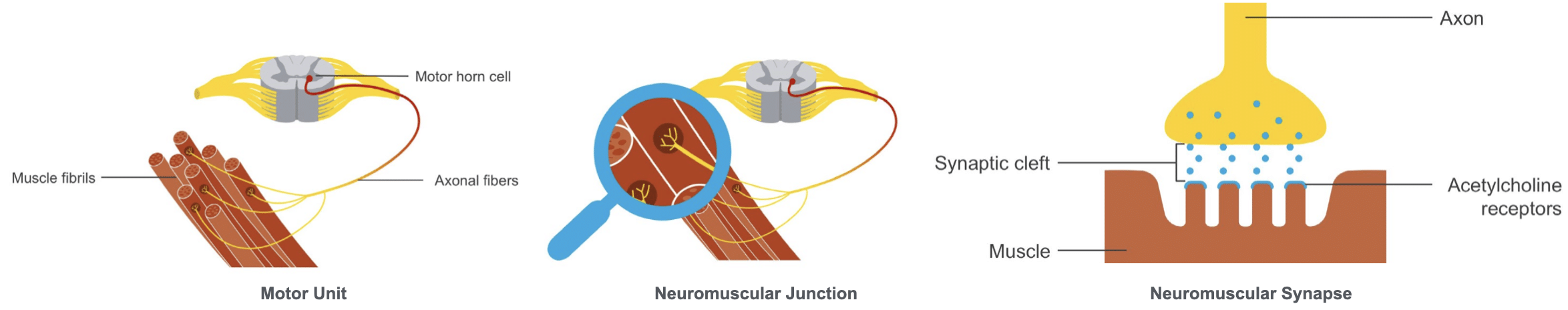
Motor Unit
- A motor unit consists of one anterior horn cell and all the muscle fibres it innervates
Neuromuscular Junction
- The connection a motor horn cell axon has with each muscle fibril is called the neuromuscular junction.
- This is a chemical synapse between the axon terminus and the muscle fiber. Acetylcholine is the neurotransmitter released from the axon terminal. Acetylcholine traverses the synaptic space, binding to specific receptors, which activates the muscle, resulting in contraction.
Testing
Clinical examination of the PNS requires careful assessment of motor, sensory, and reflex function to aid localisation.
- Identify patterns of weakness and sensory loss
- Assess for dermatomal or peripheral nerve distribution patterns
- Evaluate reflexes for asymmetry or loss
- Observe for signs of muscle atrophy, fasciculations, and trophic changes
- Distinguish between nerve root, plexus, or peripheral nerve involvement
Localising a Peripheral Nerve Injury
Signs of lower motor neuron injury:
- Atrophy
- Fasciculations
- Weakness and fatigue
- Reflex changes
Sensory findings:
- Anaesthesia
- Hypoaesthesia
- Hyperaesthesia
Axonal damage:
- Distal > proximal impairment (glove and stocking pattern)
- Atrophy in advanced cases (e.g. diabetic neuropathy)
Demyelination:
- Loss of stretch reflexes
- Weakness
- Sensory changes
Pathology Affecting Peripheral Nerves
Motor neuron disease
- Degeneration of anterior horn cells
- Varying degrees of upper motor neuron loss
- No sensory loss
- Amyotrophic lateral sclerosis (ALS)
- upper and lower motor neuron involvement;
- Babinski response; hyperreflexia
- atrophy; fasciculations
Nerve root lesions
- Herniated disc → radiculopathy
- C5–C7 and L4–S1 most commonly affected
- Sensory and/or motor symptoms
- Cauda equina syndrome → bilateral symptoms
Dorsal root lesions
- Shingles (herpes zoster)
- Tabes dorsalis (syphilis)
The Brachial Plexus
Innervates upper limb motor and sensory function.
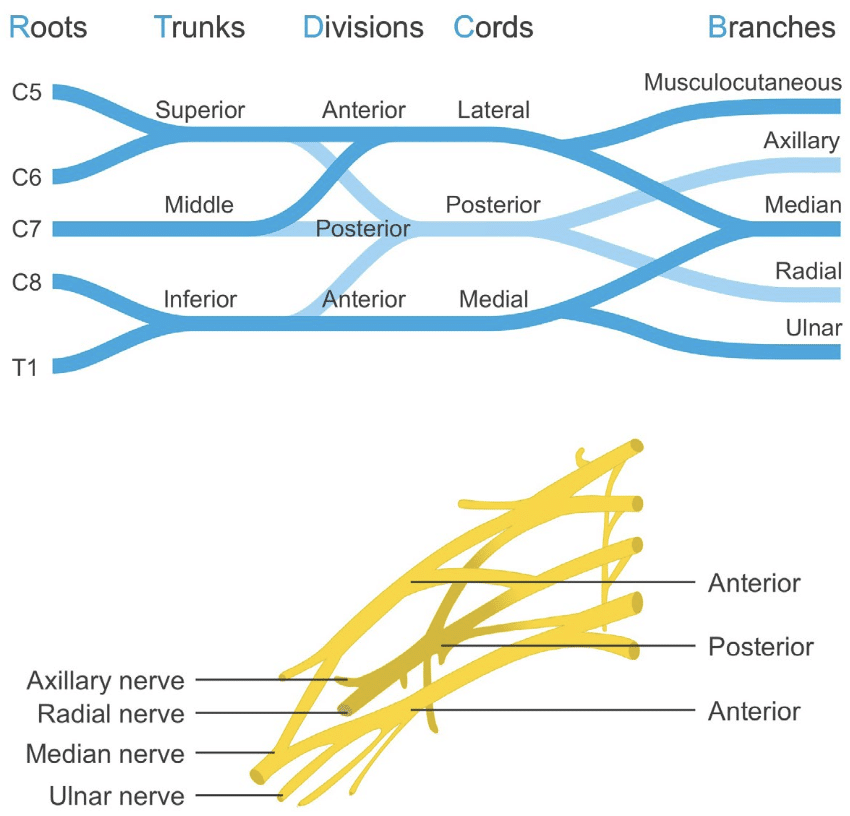
Upper plexus injuries
- Mechanism: traction injury (e.g. difficult birth)
- Erb’s palsy: medial rotation of arm, forearm pronation, wrist/finger flexion, winged scapula
Lower plexus injuries
- Mechanism: compression (e.g. Pancoast tumour)
- Klumpke palsy: claw hand, forearm supination, wrist/finger flexion
- Horner syndrome: miosis, anhidrosis, ptosis
Other causes
- Diabetic amyotrophy
- Brachial plexitis
- Neoplasia
- Post-irradiation injury
- Obstetric palsy
- Postoperative plexopathy
- Thoracic outlet syndrome
The Lumbosacral Plexus
Two plexuses (lumbar and sacral) innervate lower limb motor and sensory function.
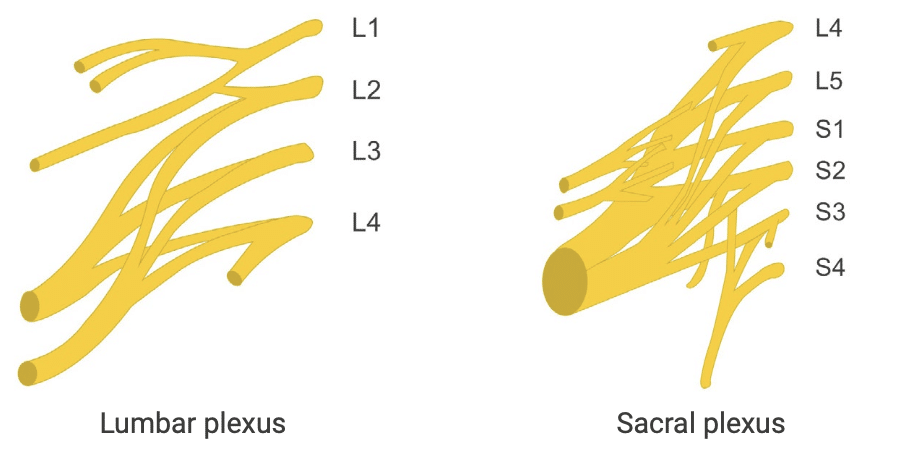
Clinically important nerves
- Femoral
- Sciatic (tibial, peroneal)
Common causes of injury
- Diabetes
- Neoplasia
- Retroperitoneal haemorrhage
- Post-irradiation plexopathy
Peripheral Examination
Examination of peripheral nervous system issues requires pattern recognition. One needs to examine and assess the appearance of the muscles, muscle power, peripheral sensation, and muscle reflexes to get a good localization of peripheral nervous system impairments.
Upper extremity motor examination
The strongest muscles in the upper arms are the flexors. The most likely muscles to show subtle weakness are the extensors. Assess pronator drift to look for lateralized muscle weakness. Observe for atrophy and fasciculations.
- C5: shoulder abduction, elbow flexion → biceps reflex
- C6: elbow flexion (semi-pronated) → brachioradialis reflex
- C7: elbow extension, finger extension → triceps reflex
- C8: finger flexion → finger flexor reflex
- T1: intrinsic hand muscles → finger abduction test
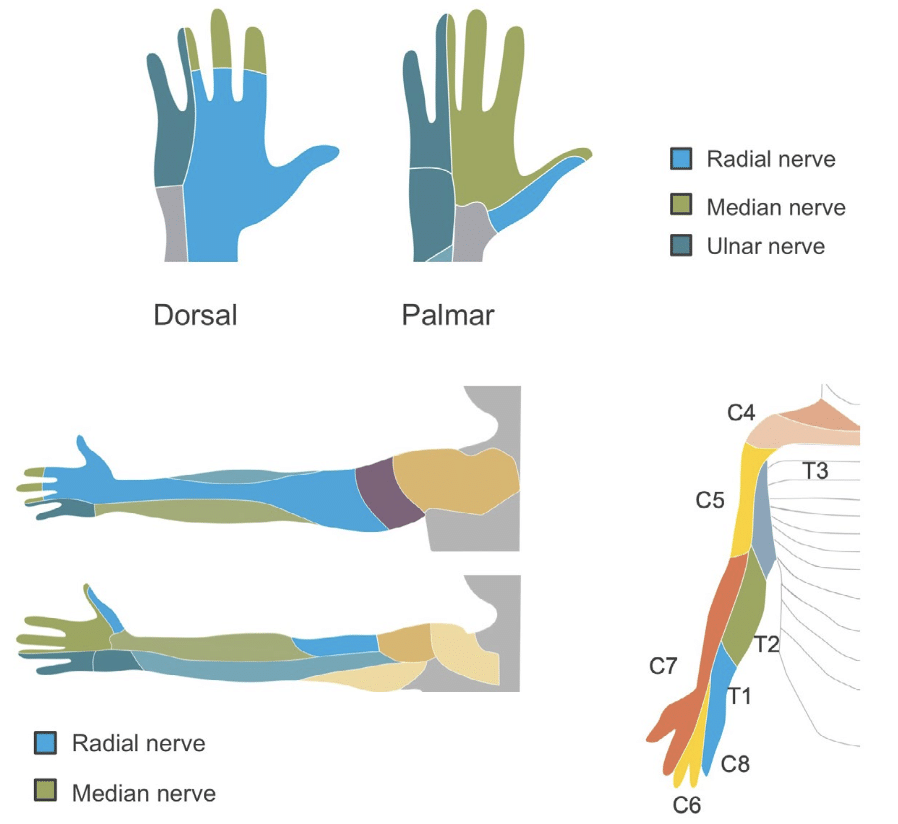
Important motor nerves
- Axillary: innervates deltoid muscle (movements of the shoulder)
- Musculocutaneous: innervates muscles important for flexion of arm at the elbow
- Radial: innervates all extensor muscles of upper extremity
- Ulnar: innervates all but four intrinsic hand muscles
- Median: innervates most flexor and pronator muscles of forearm and several intrinsic hand muscles
Upper extremity sensory examination
- Musculocutaneous
- Median
- Ulnar
- Radial
Lower extremity motor examination
The strongest muscles in the lower extremities are the extensor muscles. Weakness is more easily shown in the flexor groups. Observe for atrophy, fasciculations, and trophic changes such as changes in hair patterns, thinning of skin, and changes in arches.
In the leg, as in the arm, all muscles are innervated by more than one nerve root so that recognition of patterns of weakness become most important in peripheral neurological assessment. This can be accomplished best by reviewing general motor control and reflexes by nerve root.
- L1–L2: hip flexion → test patient laying down—have them flex hip and hold against resistance
- L3–L4: knee extension → knee jerk reflex
- L5: foot dorsiflexion, inversion, eversion, big toe extension
- S1: hip extension, knee flexion, foot plantarflexion → ankle reflex
Important motor nerves
- Femoral: supplies muscles associated with knee extension
- Sciatic: supplies knee flexion; separates into tibial and common peroneal branches
- Tibial: supplies foot plantar flexion and inversion as well as small muscles of foot
- Common peroneal: supplies dorsiflexion of foot and eversion of ankle
Lower extremity sensory examination
- Dermatomes: L4, L5, S1 commonly affected by radiculopathy
- Nerves: anterior femoral cutaneous, medial femoral cutaneous, saphenous, sciatic branches
Common Peripheral Neuropathies
Carpal tunnel syndrome
- Median nerve compression at wrist
- Nocturnal paraesthesia, positive Tinel test and Phalen tests (elicits paresthesia)
Pronator teres syndrome
- Median nerve compression passing through pronator teres muscle
- Pain in forearm and hand; less pain at night
- Daytime symptoms, pain with pronation against resistance
- Weakness of wrist pronators and distal finger flexors; Difficulty pinching
- Positive Tinel; Negative Phalen
Ulnar neuropathy
- Compression at medial epicondyle or Guyon’s canal
- Tingling in medial hand, weakness of intrinsic hand muscles
- Difficulty with fine motor control of hand (due to weakness of intrinsic muscles)
Saturday night palsy
- Compression of radial nerve in spiral groove
- Radial nerve compression → wrist drop
- Weak finger extension at metacarpophalangeal joints
Posterior interosseous syndrome
- Compression of posterior interosseous nerve (branch of radial) between heads of supinator muscle
- Radial nerve branch compression
- Weak finger extension, radial deviation of wrist
Peroneal neuropathy
- Compression of common peroneal nerve as it winds around fibular head
- Foot drop, weakness of dorsiflexion and eversion
L5 radiculopathy
- Root compression → lancinating leg pain, weakness of inversion and big toe extension
Meralgia paraesthetica
- Compression of the lateral femoral cutaneous nerve beneath inguinal ligament
- Anterolateral thigh pain and paresthesia
Diseases Affecting the Neuromuscular Junction
The neuromuscular junction is a specialized synapse allowing the conversion of nerve electrical action potentials to chemical impulses, which transmit the message for a muscle to contract.
There are multiple clinical syndromes affecting the neuromuscular junction, with the most common being myasthenia gravis.
Myasthenia gravis
- Autoimmune acetylcholine receptor disorder
- Generally occurs in younger women or in older men
- Fluctuating weakness, facial and limb involvement, ptosis, diplopia, dysphagia, respiratory fatigue
Testing
- Repetitive movement testing
- Respiratory fatigue testing
- Extended upgaze for ptosis
- Ice pack test; improvement of ptosis suggests neuromuscular junction problem (not stroke or nerve injury)
This is an edited excerpt from the Medmastery course Clinical Neurology Essentials by Robert Coni, DO, EdS, FAAN. Acknowledgement and attribution to Medmastery for providing course transcripts.
- Coni R. Headache Masterclass. Medmastery
- Simmonds GR. Neurology Masterclass: Managing Common Diseases. Medmastery
- Simmonds GR. Neurology Masterclass: Managing Emergencies. Medmastery
Clinical Neurology Essentials
- Coni R. Neuro 101: Neurological Examination. LITFL
- Coni R. Neuro 101: Cerebral Hemispheres. LITFL
- Coni R. Neuro 101: Cerebellum and Basal Ganglia. LITFL
- Coni R. Neuro 101: Brainstem. LITFL
- Coni R. Neuro 101: Cranial Nerves. LITFL
- Coni R. Neuro 101: Spinal Cord. LITFL
- Coni R. Neuro 101: Peripheral Nervous System. LITFL
References
Further reading
- Brazis PW, Masdeu JC, Biller J. Localization in Clinical Neurology. 8e 2021
- Campbell WW. DeJong’s The Neurologic Examination. 8e 2019
- Fuller G. Neurological Examination Made Easy. 6e 2019
- Kiernan J. Barr’s The Human Nervous System: An Anatomical Viewpoint. 10e 2015
- O’Brien M. Aids to the Examination of the Peripheral Nervous System. 6e 2023
- Patten JP. Neurological Differential Diagnosis. 2e 1996
- Waxman SG. Correlative Neuroanatomy. 23e 1996
Publications
- Flanigan RM, DiGiovanni BF. Peripheral nerve entrapments of the lower leg, ankle, and foot. Foot Ankle Clin. 2011 Jun;16(2):255-74
- Limthongthang R, Bachoura A, Songcharoen P, Osterman AL. Adult brachial plexus injury: evaluation and management. Orthop Clin North Am. 2013 Oct;44(4):591-603.
- Neal S, Fields KB. Peripheral nerve entrapment and injury in the upper extremity. Am Fam Physician. 2010 Jan 15;81(2):147-55
- Watson JC, Dyck PJ. Peripheral Neuropathy: A Practical Approach to Diagnosis and Symptom Management. Mayo Clin Proc. 2015 Jul;90(7):940-51
Neurology Library
Robert Coni, DO, EdS, FAAN. Vascular neurologist and neurohospitalist and Neurology Subspecialty Coordinator at the Grand Strand Medical Center in South Carolina. Former neuroscience curriculum coordinator at St. Luke’s / Temple Medical School and fellow of the American Academy of Neurology. In my spare time, I like to play guitar and go fly fishing. | Medmastery | Linkedin |

