Olanzapine toxicity
Olanzapine is a second generation atypical antipsychotic. Widely used in Australasia and therefore a fairly common presentation to the emergency department. Olanzapine like queitiapine has a predictable dose-dependent CNS depression.
Toxic Mechanism:
Olanzapine antagonises the mesolimbic dopamine (D2), serotonin, histamine the muscarninic M1 and peripheral alpha 1 receptors. This causes an anticholinergic effect (muscarinic receptors) in overdose and drowsiness (histamine receptor blockade).
Toxicokinetics:
- Rapidly absorbed, oral or sublingual
- Large volume of distribution 10-20 L/kg
- Large first pass effect
- Hepatic metabolism to inactive water-soluble metabolites
Resuscitation:
- Reduced GCS: Prompt intubation and ventilation
- Hypotension: Give 10 – 20 ml/kg of IV crystalloid, if response is not adequate start noradrenaline (adrenaline is contraindicated due to paradoxical hypotension from beta 2 mediated vasodilatation). Noradrenaline dose: 0.15mg/kg in 50ml D5W at 1-10ml/hr (0.05 – 0.5 mcg/kg/min)
- Seizures (rare)/agitation: IV benzodiazepines incrementally dosed every 5 minutes to effect.
- Check the patient is not in a dysrhythmia
- Can be managed with benzodiazepines (varying doses in the textbooks, easy method is 0.1mg/kg IV for lorazepam (max 4mg) / midazolam (max 10mg) / diazepam (max 10mg). Or…
- Lorazepam 0.1mg/kg max 4mg
- Diazepam 0.15mg/kg max 10mg
- Midazolam 0.2mg/kg max 10mg
Risk Assessment
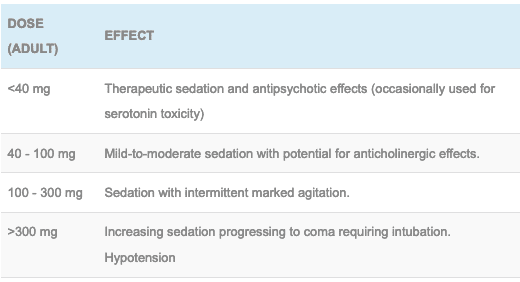
- Dose-related risk assessment:
- Children: the toxic dose is unclear but symptoms are likely to develop when >0.5 mg/kg have been ingested. Delayed extrapyramidal effects can occur in children days later.
- Clinical features should manifest within 2 – 4 hours and may last 48 hours (coma usually lasts 24 – 48 hours)
- Sedation, ataxia, miosis (unlike the mydriasis commonly seen with anticholinergics), fluctuating mental status.
- Reduced GCS, miosis and tachycardia is almost pathognomonic of olanzapine overdose in the western world.
- Tachycardia and orthostatic Hypotension
- Mild to moderate anticholinergic syndrome
Supportive Care
- Controlling the delirium can be difficult, things to consider include
- Titrated doses of benzodiazepines e.g. diazepam 2.5 – 5 mg every 5 minutes IV until gentle sedation is achieved (doses used may necessitate intubation).
- Controversially physostigmine has been used which has been reportedly reversed agitation and olanzapine comas but has its own side effect profile.
- Physical restraint
- Bladder scan and a catheter for urinary retention (no amount of benzodiazepines will fix this agitation)
Investigations
- Screening: 12 lead ECG, BSL, Paracetamol level
- Specific:
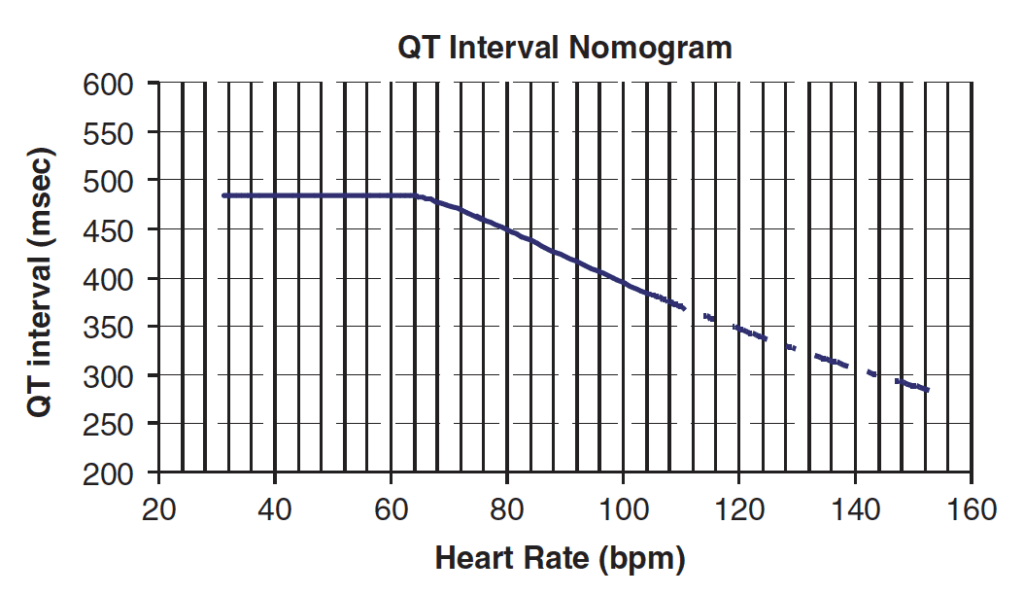
- ECG monitoring, do an ECG at presentation and 6 hours, if this is normal then cardiac monitoring may stop. If intubated then the patient will need ECG every 4 hours until clinical symptoms or cardiac abnormalities resolve. Non specific ST – T wave changes occur in 15%, minor QT prolongation but no Torsades de pointes reported
QT Nomogram
Decontamination:
- Rarely used as the onset of coma and resolution is rapid and good supportive care ensures a good outcome.
Enhanced Elimination
- Not clinical useful
Antidote
- None available
Disposition
- Children who have ingested >0.5 mg/kg should be observed in hospital for 4 hours, if asymptomatic they can be discharged but warned they may develop extrapyramidal movements up to 3 days later.
- Patients should be observed for 4 hours, if asymptomatic with a normal baseline ECG, no hypotension and eating and drinking they can be medically cleared
- Patients with any clinical features should be observed or treated as required until symptoms have resolved. Depending on severity patients may stay in an overnight observation ward or may need ICU.
References and Additional Resources:
Additional Resources:
- ECG Library – Drugs that cause QT prolongation
- Tox conundrum 046 – A fumbling, Mumbling Mess
- Neurological Mind-boggler 002 – Coma and small pupils
- Tox Flashcard – Anticholinergic Toxidrome
- Anticholinergic song
References:
- Burns MJ. The pharmacology and toxicology of atypical antipsychotic agents. Journal of Toxicology-Clinical Toxicology 2001;39(1):1-14.
- Palenzona S et al. Clinical picture of olanzapine poisoning with special reference to fluctuating mental status. Journal of Toxicology-Clinical Toxicology 2004;42(1):27-32.
Toxicology Library
DRUGS and TOXICANTS
Dr Neil Long BMBS FACEM FRCEM FRCPC. Emergency Physician at Kelowna hospital, British Columbia. Loves the misery of alpine climbing and working in austere environments (namely tertiary trauma centres). Supporter of FOAMed, lifelong education and trying to find that elusive peak performance.