Radial Nerve Lesions
Radial nerve lesions are characterized predominantly by wrist drop and inability to extend the elbow.
Variable anaesthesia is experienced over the lateral half of the dorsum of the hand and lateral forearm.
Common causes include:
- Trauma
- Compartment syndromes
- Sustained pressure to the axilla
Investigation and management depend on the cause, onset, and severity.
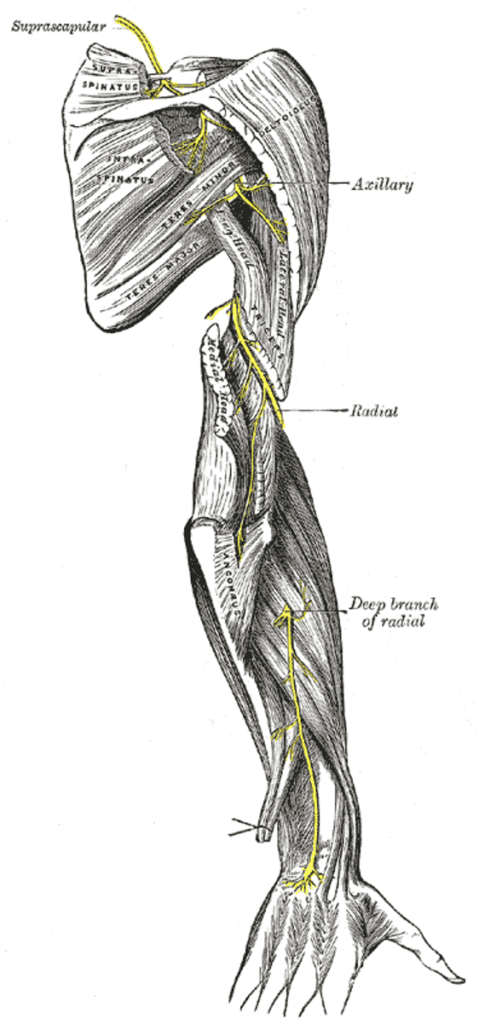
Anatomy
Course of the radial nerve
- Origin: C5–T1, from the posterior cord of the brachial plexus
- Travels between the long and medial heads of triceps, through the spiral groove with the profunda brachii artery
- Pierces the lateral fascial septum above the elbow, enters the cubital fossa
- Divides at lateral epicondyle into:
- Superficial branch: sensory
- Deep branch (posterior interosseous nerve): motor
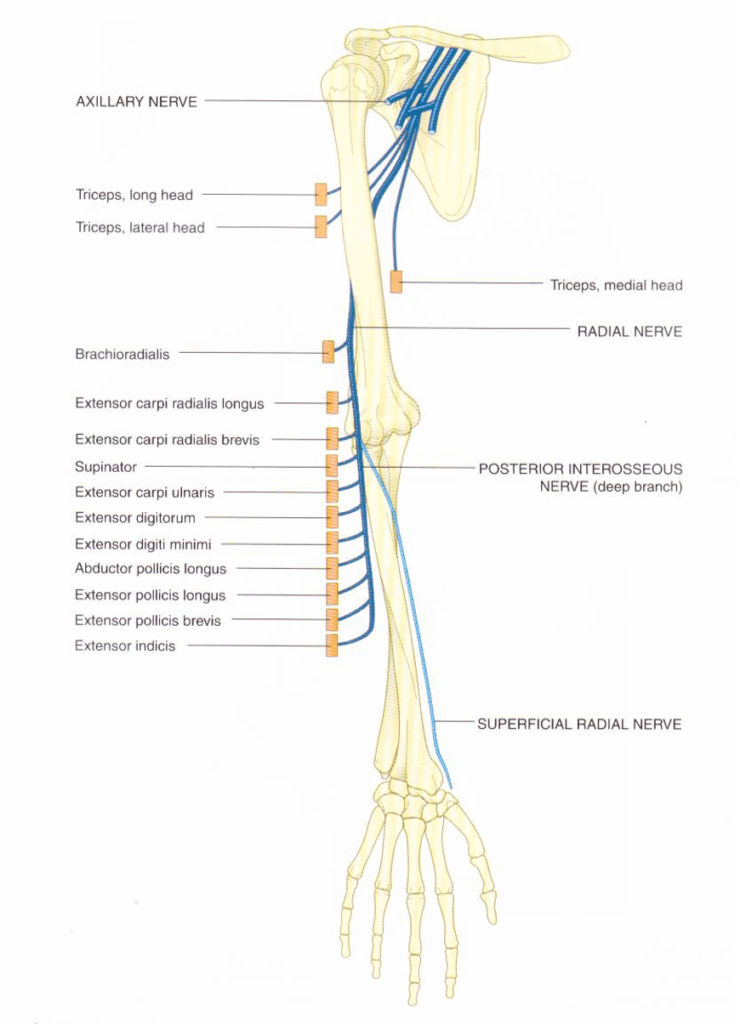
Radial nerve innervations
In axilla:
- Triceps (long and medial heads)
- Posterior cutaneous brachial nerve
In spiral groove:
- Lateral and medial heads of triceps, anconeus
- Lower lateral brachial cutaneous nerve
- Posterior cutaneous nerve of forearm
At cubital fossa:
- Lateral part of brachialis
- Supinator
- Brachioradialis
- Extensor carpi radialis longus
Superficial branch:
- Sensation to lateral 2/3 of dorsum of hand, lateral 2½ fingers
Deep branch:
- Extensor muscles of the posterior forearm
Actions of Radial Nerve-Innervated Muscles
| Muscle | Action |
|---|---|
| Triceps | Elbow extension |
| Lateral part of brachialis | Elbow flexion |
| Supinator | Forearm supination |
| Brachioradialis | Elbow flexion, brings forearm to mid-prone |
| Extensors of forearm | Extend wrist, MCP, PIP and DIP joints; thumb abduction/extension |
Pathology
Causes of radial nerve lesions
- Trauma:
- Blunt or penetrating trauma
- Fractures:
- Humeral shaft (esp. middle third)
- Monteggia fracture
- Shoulder/elbow dislocations
- Neuropraxia:
- Commonly due to axillary compression
- “Saturday night palsy” or “honeymooners palsy”
- Mass lesions:
- Tumours, abscesses
- Neuropathies:
- Diabetes mellitus
- Malignancy (compression, paraneoplastic)
- Infection: leprosy, HIV
- CTDs: RA, SLE, PAN, scleroderma, sarcoidosis
- Others: amyloidosis, Lyme disease, heavy metals
Clinical Assessment

Right: testing brachioradialis, (C5, 6), the patient flexes the forearm against resistance with the
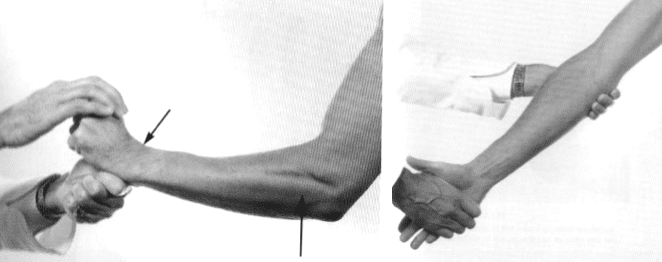
Right: testing supinator, (C6, 7), the patient supinates the forearm against resistance, with the forearm extended at the elbow
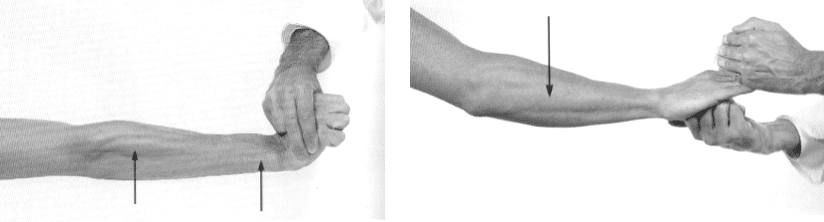
Right: testing extensor digitorum, (posterior interosseous nerve, C7, 8), extension at the MCP joints is maintained against resistance. The muscle belly and tendon can be seen and felt.
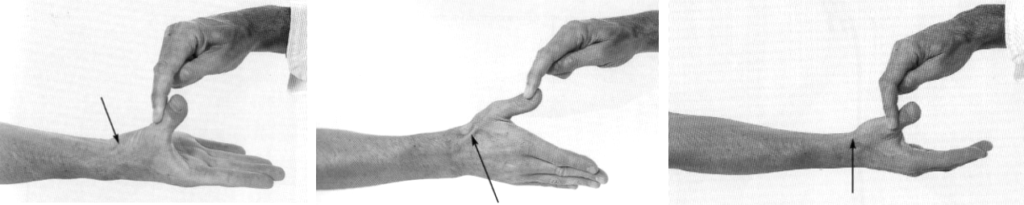
Middle: testing extensor pollicus longus, (posterior interosseous nerve, C7, 8), the patient extends the thumb at the IP joint against resistance. The tendon can be seen and felt.
Right: testing extensor pollicis brevis, (posterior interosseous nerve, C7, 8), the patient extends the thumb at the MCP joint against resistance. The tendon can be seen and felt
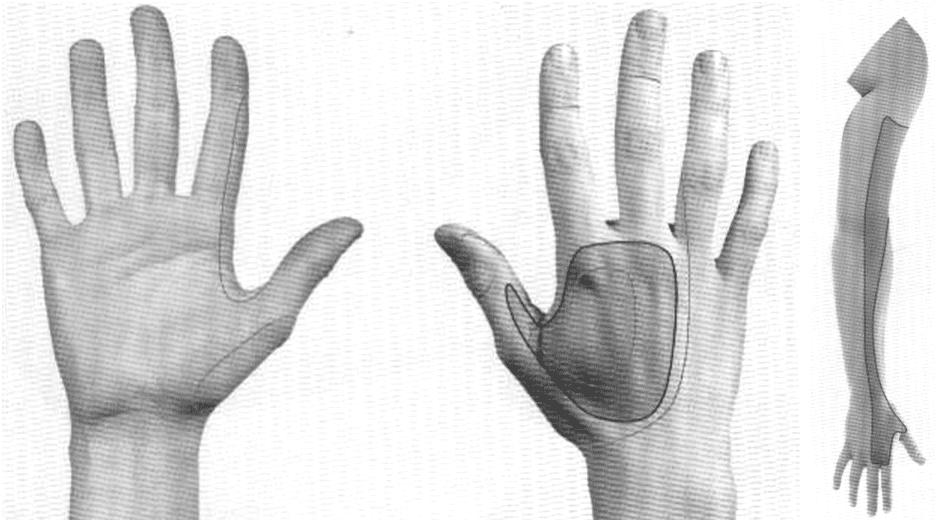
Right: The approximate area within which sensory changes may be found in high lesions of the radial nerve, (above the origin of the posterior cutaneous nerves of the arm and forearm). The average area is usually considerably smaller, and in fact absence of sensory changes has been recorded.
Radial Nerve Deficits
Axilla lesions:
- Paralysis: triceps, anconeus, extensors
- Wrist drop, inability to grip
- Sensory loss: posterior arm/forearm, dorsum of lateral hand and fingers
Spiral groove lesions:
- Paralysis: wrist/finger extensors
- Triceps and cutaneous branches spared
- Wrist drop, ± small dorsal sensory deficit
Deep branch injury:
- Motor loss to posterior forearm extensors (except supinator, ECRL)
- No wrist drop
- No sensory loss
Superficial branch injury:
- Pure sensory deficit over dorsum of hand and lateral fingers
Investigations
- Nerve conduction studies: diagnosis, rule out generalised disease, predict prognosis
- Blood tests: FBC, U&Es, glucose, CRP, ESR, heavy metals if indicated
- CT/MRI: delineate compressive lesions, visualise nerve pathology
- Biopsy: rarely indicated for mononeuritis, suspected leprosy
Management
- Treat the underlying cause
- Compartment syndrome:
- Fasciotomy if indicated
- Occupational therapy:
- Splinting, functional supports
- Physiotherapy:
- Rehabilitation and prevention of complications
Disposition
Depends on:
- Cause of lesion
- Severity
- Onset
Appendix 1
Median Nerve Anatomy
Appendix 2
References
Publications
- Brazis PW, Masdeu JC, Biller J. Localization in Clinical Neurology. 8e 2021
- Fuller G. Neurological Examination Made Easy. 6e 2019
- O’Brien M. Aids to the Examination of the Peripheral Nervous System. 6e 2023
FOAMed
- Cadogan M. Sir Henry Head (1861-1940). LITFL
- Cadogan M. Holstein–Lewis fracture. LITFL
- Coni R. Neuro 101: Peripheral Nervous System. LITFL
- Nickson C. Myotomes and Differentiating Nerve Lesions. LITFL
Fellowship Notes
MBBS DDU (Emergency) CCPU. Adult/Paediatric Emergency Medicine Advanced Trainee in Melbourne, Australia. Special interests in diagnostic and procedural ultrasound, medical education, and ECG interpretation. Co-creator of the LITFL ECG Library. Twitter: @rob_buttner
Educator, magister, munus exemplar, dicata in agro subitis medicina et discrimine cura | FFS |


