Something in my eye, Doc
aka Ophthalmology Befuddler 010
A mechanic presents to the emergency department saying “I’ve got something in my eye, Doc“
Early in the day he was cleaning up the workshop and felt something get in his right eye, he then rinsed his eye out with water. Over the course of the day the irritation worsened, his eye is constantly watering and its becoming red.
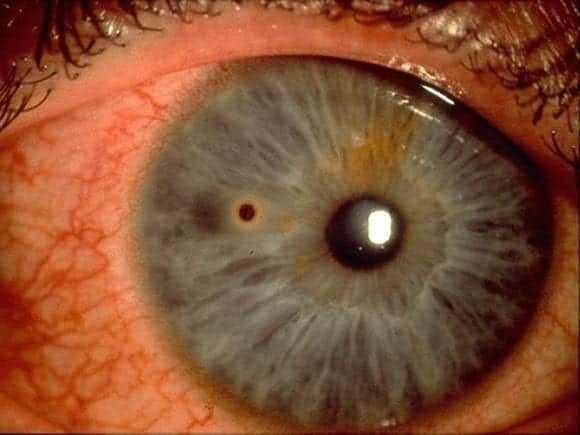
With the slit lamp you see this:
Questions
Q1. What is the diagnosis?
Answer and interpretation
Corneal foreign body with rust ring
The foreign body is at about 9 o’clock o the surface of the cornea, midway across the iris. A rust ring and conjunctival injection is present.
Q2. What the important features to consider on history and examination?
Answer and interpretation
History:
- What type of foreign body? — e.g. dirt or organic material (higher risk of infection), glass, metal (rust ring may lead to inflammation and a corneal epithelial defect), inorganic material
- Velocity of impact? — e.g. angle grinders, high speed drilling and ‘weed eater’ injuries are at risk of corneal or scleral penetration.
- Symptoms? — foreign body sensation, tearing, blurred vision.
- Use of eye protection?
Examination:
Visual acuity — reduced if central foreign body or penetrating trauma
Slit lamp exam and tonometry:
- Assess size, site, nature of foreign body, and depth of injury
- Determine if a rust ring is present.
- Conjunctival injection, eyelid edema, mild AC reaction, and SPK may be present.
- Examine closely for iris tears and transillumination defects, lens opacities, AC shallowing, and asymmetrically low IOP in the involved eye.
- Distortion of the cornea, anterior chamber, iris, pupil or lens indicates ocular penetration.
Handy tips:
- Remember to evert the eyelids in the quest for foreign bodies.
- Don’t fall into the trap of settling for one foreign body — there may be more!
- Beware of self-sealing lacerations — Seidel test may be helpful but does not rule out corneal lacerations. [Erich Seidel (1882 – 1948)]
Seidel positive Test (RootAtlas)
Q3. What features may indicate can occult foreign body under an eyelid?
Answer and interpretation
Vertically orientated linear corneal abrasions or the presence of superficial punctate keratopathy (SPK).
Q4. What features suggest concomitant infection in a patient with a corneal injury?
Answer and interpretation
The presence of a corneal infiltrate with:
- significant anterior chamber reaction
- pain
- severe conjunctival injection
- purulent discharge
If these features are present, the following may be required:
- eye swab and culture
- treat with antibiotics
- close follow up by an ophthalmologist.
Q5. What methods may be used for removing corneal foreign bodies? What are their advantages and disadvantages?
Answer and interpretation
The general procedure is:
- apply topical anesthesia e.g. 1% amethiocaine
- position the patient at the slit lamp — ask him or her to keep still by by pressing against the forehead rest and to focus on your ear (if its clean…) or a target over the your shoulder.
- focus the slit lamp on the foreign body.
- approach the foreign body from an oblique to reduce the risk of causing damage.
- steady the hand removing the foreign body on the frame of the slit lamp or head rest.
The foreign body may be removed using different devices:
- cotton bud aka Q-tip — good for superficial foreign bodies that can be swept away and atraumatic. Useless for adherent foreign bodies.
- 18G-30G needle — readily available, easily to perform with practice, and skilled practitioners leave little trauma. There is obvious potential for causing damage. The tip should always be pointed away from the globe so that the beveled edge is used to scrape the foreign body. Some patients freak out at the idea of a needle being in contact with their eye so the doctor needs a well developed sense of aequanimitas…
- Motorised dental burr — the lack of a sharp tip is reassuring but excessive use can create a significant epithelial defect.
Removing a metal foreign body from the cornea
Q6. Are conjuctival foreign bodies treated differently?
Answer and interpretation
These are generally less serious and can be removed using fine forceps or a cotton bud. A good tip is to soak the tip of the cotton bud in 2.5% phenylephrine to reduce bleeding if present. A sweep under the eyelids may be necessary.
Follow up is as required, or at 1 week if the foreign body was incompletely removed (it may surface with time).
Q7. Should you pad/ patch the eye?
Answer and interpretation
There is no evidence that eye patches are helpful. They may even be harmful due to loss of binocular vision. A meta-analysis has shown that for small corneal abrasions there is no benefit from patching the eye.
Q8. Should antibiotic eye drops or ointment be used?
Answer and interpretation
They are both effective. Drops have the advantages of being less messy and allow the patient to see out of both eyes.
Q9. What is appropriate follow up for a patient following removal of a corneal foreign body?
Answer and interpretation
Daily follow up for slit lamp and fluorescein examination to comparatively measure the extent of the defect and assess healing would be ideal, but in practice I tend to get them followed up after 2-3 days to save on slit lamp light bulbs…
Q10. When should a patient with a corneal foreign body be referred to an ophthalmologist?
Answer and interpretation
- If the foreign body — or an associated rust ring — is not completely removed follow up should be arranged within 24 hours.
- Opthalmology review is required if there is a persistent epithelial defect (>3 days)
- Ocular penetration
Q11. What advice should be given to a contact lens wearer who had a corneal foreign body?
Answer and interpretation
Contact lens use should be avoided until the defect is fully healed or feels normal for at least 1 week.
References
- Turner A, Rabiu M. Patching for corneal abrasion. Cochrane Database Syst Rev. 2006 Apr 19;(2):CD004764. PMID: 16625611.
- Ehlers JP, Shah CP, Fenton GL, Hoskins EN. The Wills Eye Manual: Office and Emergency Room Diagnosis and Treatment of Eye Disease Lippincott Williams & Wilkins
- NSW Statewide Opthalmology Service. Eye Emergency Manual — An illustrated Guide. [Free PDF]

OPHTHALMOLOGY BEFUDDLER
Chris is an Intensivist and ECMO specialist at The Alfred ICU, where he is Deputy Director (Education). He is a Clinical Adjunct Associate Professor at Monash University, the Lead for the Clinician Educator Incubator programme, and a CICM First Part Examiner.
He is an internationally recognised Clinician Educator with a passion for helping clinicians learn and for improving the clinical performance of individuals and collectives. He was one of the founders of the FOAM movement (Free Open-Access Medical education) has been recognised for his contributions to education with awards from ANZICS, ANZAHPE, and ACEM.
His one great achievement is being the father of three amazing children.
On Bluesky, he is @precordialthump.bsky.social and on the site that Elon has screwed up, he is @precordialthump.
| INTENSIVE | RAGE | Resuscitology | SMACC
