Tension Pneumothorax – an alternative view
Ever since I was a junior medical officer and I was faced with a spontaneous tension pneumothorax at sea on a dived submarine…I have had an interest in managing pneumothorax.
A tension pneumothorax is the presence of intrapleural air that is under positive pressure throughout the entire respiratory cycle. It occurs when air enters the thorax through a pleural defect but can not leave (a one way cat flap). We have all been taught that we should never see a chest x-ray of a tension pneumothorax, with good reason. It is a diagnosis that should be made on clinical grounds only and certainly never have a chest x-ray performed to confirm your suspicion (although here is one… well, these things happen).
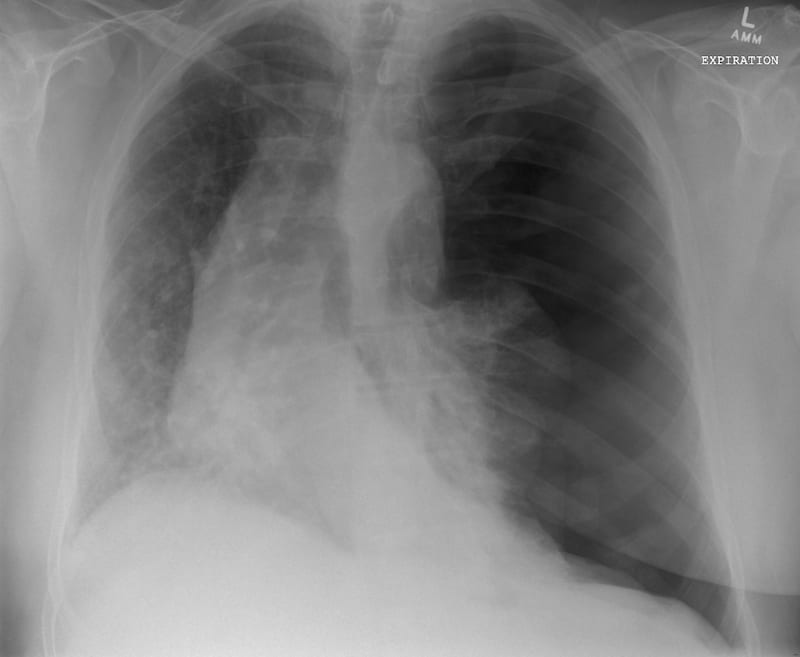
Of all of the clinical signs that we have been taught to recognise – it is the rapidity of deterioration of a patients’ clinical condition, in the context of known, or clinical signs of a pneumothorax that should make you think of the presence of a tension. Learned texts speak of distended neck veins, tracheal deviation and a displaced apex beat (very difficult to ascertain); these are late signs and clinicians should have considered and be acting upon the diagnosis before these are present.
Prompt recognition and treatment is key – traditionally we have been taught needle decompression in the second intercostal space, mid-clavicular line. Whilst this does facilitate timely access to the pleural space for some – it may not be the best anatomical choice for all – but more of that (and ideal needle length) another time…
So, if we are agreed that we should not be seeing chest x-rays of tension pneumothoraces – what about a CT scan of tension pneumothorax?
What features can been seen on this CT?
- Increased thoracic volume R side
- Displaced mediastinum
- Collapse and occlusion of the right main bronchus. Just distal to the carina it forms a crescent shape and then occludes. The whole of the right lung is collapsed as a result.
- Collapse of left lower lobe
- A large bore chest tube in situ in the right thoracic cavity with no apparent occlusion of the tube
It is worthwhile stopping and considering for a moment some of these features present on the scan. We are used to hearing about a displaced mediastinum which, as it worsens, we understand to gradually occlude the vena cava causing eventual reduction and cessation of venous return to the right ventricle. But what about complete collapse of the right main bronchus? Anatomically, there are intact concentric rings of cartilage at this point in the bronchial tree. To cause collapse and occlusion of these rings there must be a very considerable positive intrathoracic pressure acting upon them.
Experimental physiological data on this subject are sparse to give reliable estimates, but it is known that a pressure of 6Kpa (~60cm/H20) will cause the posterior membrane of human trachea to invaginate with surface contact between the membrane and lateral walls. The likelihood of collapse is greater when there is longitudinal tension or flexion on the trachea. In this case with right main bronchus collapse, the concentric cartilagenous rings should (in theory) be able to withstand more pressure before deformation or collapse than the incomplete ‘C’ shaped rings in the trachea. Perhaps in this case the additional longitudinal tension and/or flexion on the bronchial tree as the mediastinum was deviated modified that likelihood.
This individual already had a 28F chest tube in place following penetrating thoracic trauma and a haemopneumothorax – this was subsequent ‘traumagram’ CT. He was clinically stable going in – says he felt dreadful in the scanner, and quickly better when the gantry moved back out again. Considering the patient had a patent chest tube at the beginning of the investigation and a patent tube as we rushed in straight after the investigation – what could have happened?
So what happened?
We think that the chest drain tubing got snagged in the gantry as the patient moved into the scanner. This occluded the tube, stopping egress of air from the thoracic cavity, resulting in increasing intrathoracic pressure and ultimately a tension on the affected side.
Either way, this case allows you to appreciate the gross cardiopulmonary insult a tension pneumothorax can induce in a short space of time.
Take home message
Transfer of the traumatised and/or critically ill patient requires careful handing and planning ahead – particularly when moving parts are involved.
Tubes, lines and monitoring wires may all be sitting safely before the scan starts – but think ahead to where all these items will be when the patient has moved into the scanner!
LITFL Further Reading
- Brims F. Tension pneumothorax – time to change the old mantra? LITFL
- Johnston M. Searching for Smaug. LITFL
- Brims F. Tension Pneumothorax – an alternative view. LITFL
- Own the Chest Tube. CCC
- Rippey J. Lung ultrasound: Pneumothorax. LITFL
- Nickson C. Pneumothorax. CCC
- Top 100 CXR
References
- Brims F. Primary spontaneous tension pneumothorax in a submariner at sea. Emergency medicine journal: EMJ 2004;21:394
- Begis D, Delpuech C, Le Tallec P, Loth L, Thiriet M, Vidrascu M. A finite-element model of tracheal collapse. Journal of applied physiology 1988;64:1359-68.
- Leigh-Smith S, Harris T. Tension pneumothorax–time for a re-think? Emergency medicine journal : EMJ 2005;22:8-16.
- Brims F. Tension pneumothorax – time to change the old mantra?
[cite]

Critical Care
Compendium
Prof Fraser Brims Curtin Medical School, acute and respiratory medicine specialist, immediate care in sport doc, ex-Royal Navy, academic| Top 100 CXR | Google Scholar | ICIS Course ANZ
