Tension pneumothorax – time to change the old mantra?
Here is your ATMIST handover in resus: 28 year old male, injured 25 minutes ago, penetrating chest trauma, Asherman seal on anterior chest, RR 35, clearly deteriorating, high flow O2 administered.
Initial observations: A – moaning, distressed, mask fogging, B – RR is now more like 40, with reduced expansion on the right, and absent breath sounds
Are his neck veins distended? Trachea deviated?
You are swift, brave and decisive – in goes the 14G cannula, 2nd intercostal space, mid clavicular line and…nothing happens. In fact, the patient continues to deteriorate…
What is your next option?
Following the recent LITFL blog demonstrating a CT of a tension pneumothorax, we review some of the controversies in managing this much-maligned medical emergency.
Tension pneumothorax describes the progressive accumulation of air in the pleural cavity (normally a potential space) through a defect in the visceral pleura. This leads to positive pressure being maintained and increasing throughout the respiratory cycle causing vessels within the mediastinum to be compressed with catastrophic consequences if left untreated. Clinical signs include hypoxia, hypotension, tachycardia, reduced breath sounds and hyper resonance ipsilaterally, with tracheal deviation (away from the affected side) and distended neck veins being late clinical signs.
In treating a tension pneumothorax, we have traditionally been taught to place a large bore catheter in the second intercostal place (2nd ICS) mid-clavicular line, and this method is still advocated in ATLS guidelines. It is the obvious choice in terms of ease of anatomical location where speed is of the essence with a time-critical injury.
However, this approach may not be the most effective position to provide live-saving decompression and there is conflicting, and a lack of quality, evidence to support the 2nd ICS approach.
The 2nd ICS mid clavicular line approach for needle decompression
- Using a conventional 45 mm catheter, it may not be effective in 22-50% of trauma patients due to chest wall thickness
- Incorrect placement can cause internal mammary, subclavian and even cardiac damage
- The use of this approach seems to have developed in the absence of a sound evidence base for efficacy – it was probably advocated and has been used widely because of ease of access – with a patient supine or sat up, it is a straight forward approach.
But, what do we do with the up to 50% of patients it doesn’t work in?
What do you do it you don’t hear that famous affirming hiss from the pleural cavity?
The use of a longer needle (8.25cm) has been previously advocated. While this would likely guarantee reaching the pleural space, the risks may outweigh the benefits especially in cases where the patient has been misdiagnosed. Vascular, visceral and pulmonary parenchymal iatrogenic damage have all been reported.
Military conflict frequently acts as a catalyst for significant developments in trauma management and now, following the conflicts over the last 10 years, the military (and others) advocate using a mid axillary approach 5th intercostal space (5ICS: or a hands width from the axilla in the heat of battle). This approach is now recommended in patients where body habitus, pectoral muscle bulk or body armour may limit access to the pleural space. Remember, the trauma population is generally younger and male predominant, so some of the published studies on chest wall thickness may not be so relevant (particularly the cadaver studies: its too late by then!).
It is widely accepted that chest drains for definitive management are placed in the 5th ICS mid axillary line so why not opt for this site for emergency decompression?
- Advantages of the 5th ICS approach
- Thinner chest wall – increased chance of successful access to the pleural space
- Anatomically there are no major blood vessels nearby
- Disadvantages of the 5th ICS approach
- Less easy access
- Transport/movement of the patient – arms by the side will dislodge the catheter
So, what now – a longer needle? Or move and try again in the 5th ICS mid axillary line?
Assuming that your diagnosis is correct and accepting that each case should be taken on its own merits, we would suggest trying the 5th ICS mid axillary line approach. Pragmatically, the equipment is more quickly available (or even still in your hand from the first attempt) than a spinal needle and unless you are dealing with a particularly obese patient you are highly likely to access the pleural space with your 45mm catheter. Secondary options would be a longer needle or rapid blunt dissection down in the 5th ICS mid axillary line to ribs and then either passing the catheter or continue on to put a hole in the pleura yourself – i.e. straight to thoracostomy.
Why are we using IV cannulae to access the pleural space‽
There are very few bespoke kits available or accepted for this indication. More recently there have been a number of pleural thoracocentesis kits on the market which are comprised of 6 or 8F catheters which are longer, very hard to kink and more robust than IV cannulae and consequently are more effective and last longer. The development and validation of such adapted catheters (with an optimum length, position and kink resistance to be defined) for needle decompression of tension pneumothoraces should be supported and ultimately available for ED departments and pre-hospital care teams. Note, this is currently an unlicensed use of these products, but, when you think of it, so is using an IV cannula.
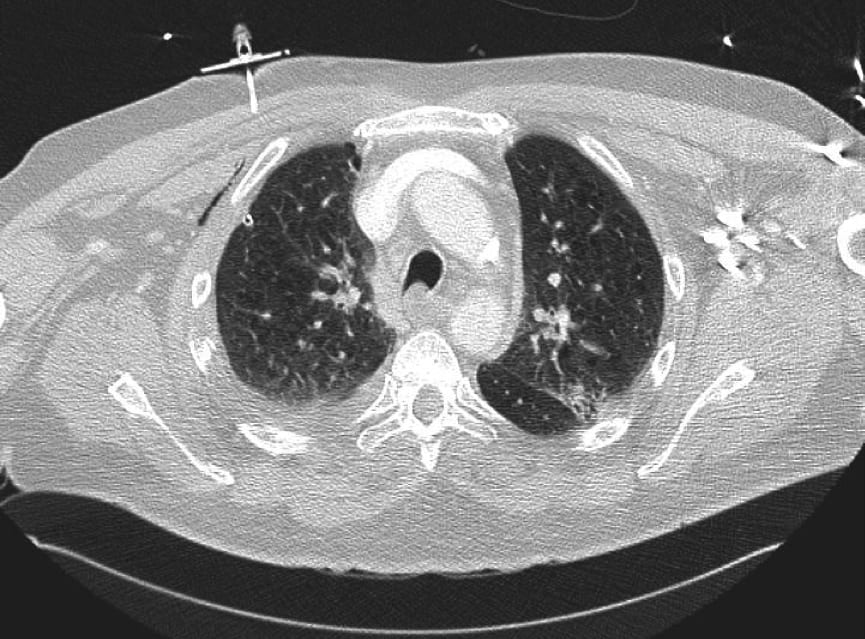
This is a CT image of a patient with COPD who presented with a secondary pneumothorax, who then tensioned in ED. The 6F pleural catheter is still in situ and patent (with the tip visible just inferior to the anterior rib).
The universal mantra from medical school of the 2nd ICS mid clavicular line approach is not wrong, it’s just that it might not work in a worst case of up to 50% of trauma patients. We all need to be cognisant that if the patient is obese or has a reasonable pectoral muscle mass, the 5th ICS mid axillary line should be the second port of call, or for some, may even be a more appropriate first line approach.
LITFL Further Reading
- Brims F. Tension pneumothorax – time to change the old mantra? LITFL
- Johnston M. Searching for Smaug. LITFL
- Brims F. Tension Pneumothorax – an alternative view. LITFL
- Own the Chest Tube. CCC
- Rippey J. Lung ultrasound: Pneumothorax. LITFL
- Nickson C. Pneumothorax. CCC
- Top 100 CXR
References
- Brims FJH. Primary spontaneous tension pneumothorax in a submariner at sea. Emerg Med J 2004;21:394–5. doi:10.1136/emj.2003.010462 [PMC 1726340]
- Beckett A, Savage E, Pannell D, et al. Needle Decompression for Tension Pneumothorax in Tactical Combat Casualty Care: Do Catheters Placed in the Midaxillary Line Kink More Often Than Those in the Midclavicular Line? The Journal of Trauma: Injury, Infection, and Critical Care 2011;71:S408–12. doi:10.1097/TA.0b013e318232e558 [PMID 22071996]
- Stevens RL, Rochester AA, Busko J, et al. Needle Thoracostomy for Tension Pneumothorax: Failure Predicted by Chest Computed Tomography. Prehosp Emerg Care 2009;13:14–7. doi:10.1080/10903120802471998 [PMID 19145519]
- Givens ML. Needle Thoracostomy: Implications of Computed Tomography Chest Wall Thickness. Academic Emergency Medicine 2004;11:211–3. doi:10.1197/j.aem.2003.09.015 [PMID 14759970]
- Yarmus L. Pneumothorax in the Critically Ill Patient. Chest 2012;141:1098–105. doi:10.1378/chest.11-1691 [PMID 22474153]
Beekley AC, Starnes BW, Sebesta JA. Lessons Learned from Modern Military Surgery. Surgical Clinics of North America 2007;87:157–84. doi:10.1016/j.suc.2006.09.008 [PMID 17127127] - Sujan MA et al. Emergency Care Handover (ECHO study) across care boundaries: the need for joint decision making and consideration of psychosocial history. Emerg Med J doi:10.1136/emermed-2013-202977 [BMJ Full text]
Beekley AC, Starnes BW, Sebesta JA. Lessons Learned from Modern Military Surgery. Surgical Clinics of North America 2007;87:157–84. doi:10.1016/j.suc.2006.09.008 [PMID 17127127]
Co-authored with Ian Duffus, a Medical Student based at Leeds Medical School in the UK.
[cite]

Critical Care
Compendium
Prof Fraser Brims Curtin Medical School, acute and respiratory medicine specialist, immediate care in sport doc, ex-Royal Navy, academic| Top 100 CXR | Google Scholar | ICIS Course ANZ
