Ocular Ultrasound Challenge
aka Ophthalmology Befuddler 015
Eyes are filled with fluid. This means they are the perfect organ for ultrasound assessment in the emergency department.
Think you know all about ocular ultrasound? Let’s find out…
Questions
Q1. In which 5 settings or emergency presentations should you consider using ocular ultrasound?
Answer and interpretation
- Decreased or loss of vision
- Suspected ocular foreign body
- Ocular pain
- Eye trauma
- Head injury or suspected raised intracranial pressure
Q2. Describe how ocular sonography is performed.
Answer and interpretation
Ocular ultrasound should be performed by an appropriately trained and accredited practitioner. This is how its done:
- Use a high-resolution (e.g. 7.5 MHz or higher) linear array ultrasound transducer.
- apply a large amount of standard water-soluble ultrasound transmission gel to the patient’s closed eyelid so that the transducer doesn’t actually need to touch the eyelid.
- adjust ‘DFG’ — adjust depth so that the image of the eye fills the screen, adjust the focus as required and turn up the gain to achieve acceptable imaging (to assess the vitreous chamber the eye should be examined at both ‘moderate’ and ‘high’ gain settings).
- Scan both eyes in both the sagittal and transverse planes through closed eyelids.
- Ask the patient to ‘look straight ahead with eyes closed’, but without clenching the eyelids. While scanning ask the patient to ‘look’ up, down, left and right
Nice work, you’ve just performed an ocular ultrasound!
This is what you see:
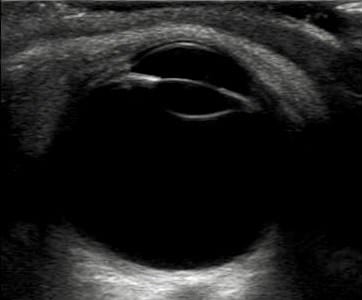
Q3. What does the image show? Describe the features.
Answer and interpretation
This is a normal eye!
The normal eye appears as a circular hypoechoic structure with the following structures:
- cornea — thin hypoechoic layer parallel to the eyelid.
- anterior chamber — filled with anechoic fluid and is bordered by the cornea, iris and anterior reflection of the lens capsule.
- iris and ciliary body — echogenic linear structures extending from the peripheral globe towards lens. Pupillary response can be assessed by shining a light in the fellow eye.
- lens — anechoic.
- vitreous chamber — filled with anechoic fluid in the young healthy eye.
- retina — cannot be differentiated from the other choroidal layers.
- retrobulbar area includes optic nerve, extraocular muscles and bony orbit — the optic nerve is visible posteriorly as a hypoechoic linear region radiating away from globe. Doppler can be used to assess the central retinal artery.
Q4. What traumatic eye injuries may be diagnosed using ultrasound?
Answer and interpretation
- globe perforation
- retrobulbar hematoma or emphysema
- retinal detachment
- lens subluxation/ dislocation
- vitreous hemorrhage and hyphema
- intraocular foreign body
Q5. What are the ultrasound findings of globe rupture?
Answer and interpretation
- decrease in the size of the globe
- anterior chamber collapse
- buckling of the sclera
Q6. What are the ultrasound findings of a dislocated lens?
Answer and interpretation
- the lens is displaced from its normal position, either anteriorly or posteriorly.
- this may be a result of trauma or occur in conditions like Marfan’s syndrome.
- other evidence of trauma, such as vitreous hemorrhage, globe rupture or retinal detachment may also be present.
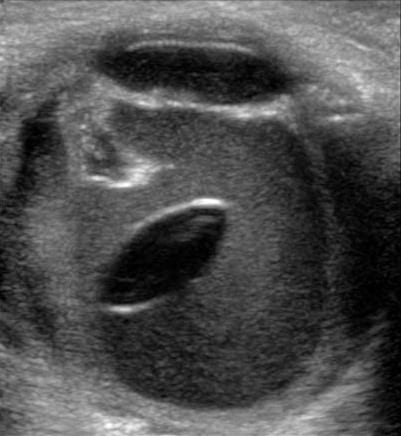
Traumatic posterior lens dislocation with an accompanying vitreous hemorrhage
Q7. What are the ultrasound findings of an intraocular foreign body?
Answer and interpretation
- bright echogenic acoustic profile of the foreign body
- shadowing or reverberation artifacts may be seen
Q8. What are the ultrasound findings of retinal detachment?
Answer and interpretation
- A thick hyperechoic undulating membrane in the posterior/ lateral globe
- in total retinal detachments the folded surface attaches to the ora serrata anteriorly and the optic nerve posteriorly.
- This condition is considered in Ophthalmology Befuddler 008
Q9. How can raised intracranial pressure be detected using ultrasound?
Answer and interpretation
Optic nerve sheath diameter (ONSD) correlates closely with ICP and can be measured using ocular ultrasound.
The normal optic nerve sheath is up to 5 mm in diameter. ONSD is higher in the presence of a raised ICP (>20 mmHg).
How to measure ONSD:
- take the measurement 3 mm posterior to the globe for both eyes (ultrasound contrast is high at this point and measurements are more reproducible)
- average two measurements
- suspect raised ICP if the average ONSD is >5 mm
The evidence:
- Kimberley et al (2008): ONSD > 5 mm detects ICP > 20 cm H2O with a sensitivity of 88% (95% CI = 47% to 99%) and specificity of 93% (95% CI = 78% to 99%)
- Moretti et al (2009): ONSD threshold of 5.2 mm as a predictor of ICP >20 mm Hg had sensitivity and specificity of 94% and 76%, respectively.
- Rajajee et al (2011): Optimal ONSD for detection of ICP > 20 mmHg was ≥0.48 cm with sensitivity 96% (95% CI 91-99%); specificity 94% (92-96%)
Q10. What are the ultrasound features of posterior vitreous detachment?
Answer and interpretation
Fine linear and granular appearing echodensities visible in the vitreous chamber when gain settings are ‘very high’. There is a swirling appearance when the patient moves his or her eyes.
Unlike retinal detachment, vitreous detachment:
- occurs in front of the optic disc and does not remained anchored to it.
- lacks a thickened hyperechogenic membrane.
This condition is considered in Ophthalmology Befuddler 012
Q11. what are the ultrasound features of vitreous hemorrhage?
Answer and interpretation
- Fresh mild hemorrhages — small dots or linear areas of areas of low reflective mobile vitreous opacities
- More severe and older hemorrhages — blood organizes and forms membranes.
- Vitreous hemorrhages may also layer inferiorly due to gravitational forces.
Ultrasound can also detect a hyphaema in eye trauma when the eyelids cannot be opened.
References
- Babineau MR, Sanchez LD. Ophthalmologic procedures in the emergency department. Emerg Med Clin North Am. 2008 Feb;26(1):17-34, v-vi. PMID: 18249255.
- Blaivas M, Theodoro D, Sierzenski PR. A study of bedside ocular ultrasonography in the emergency department. Acad Emerg Med. 2002 Aug;9(8):791-9. PMID: 12153883.
- Kimberly HH, Shah S, Marill K, Noble V. Correlation of optic nerve sheath diameter with direct measurement of intracranial pressure. Acad Emerg Med. 2008 Feb;15(2):201-4. PubMed PMID: 18275454.
- Liu Y, Chen J. Focused bedside ocular ultrasound. Acad Emerg Med. 2008 Aug;15(8):792. PMID: 18783493.
- Major R, al-Salim W. Towards evidence based emergency medicine: best BETs from the Manchester Royal Infirmary. BET 3. Ultrasound of optic nerve sheath to evaluate intracranial pressure. Emerg Med J. 2008 Nov;25(11):766-7. PMID: 18955621.
- McIlrath ST, Blaivas M, Lyon M. Diagnosis of periorbital gas on ocular ultrasound after facial trauma. Am J Emerg Med. 2005 Jul;23(4):517-20. PMID: 16032623.
- Moretti R, Pizzi B. Optic nerve ultrasound for detection of intracranial hypertension in intracranial hemorrhage patients: confirmation of previous findings in a different patient population. J Neurosurg Anesthesiol. 2009 Jan;21(1):16-20. PubMed PMID: 19098619.
- Rajajee V, Vanaman M, Fletcher JJ, Jacobs TL. Optic nerve ultrasound for the detection of raised intracranial pressure. Neurocrit Care. 2011 Dec;15(3):506-15. PubMed PMID: 21769456.
- Sawyer MN. Ultrasound imaging of penetrating ocular trauma. J Emerg Med. 2009 Feb;36(2):181-2. Epub 2007 Aug 29. PMID: 17976814.
- Shinar Z, Chan L, Orlinsky M. Use of Ocular Ultrasound for the Evaluation of Retinal Detachment. J Emerg Med. 2009 Jul 20. [Epub ahead of print] PMID: 19625159.
- Tayal VS, Neulander M, Norton HJ, Foster T, Saunders T, Blaivas M. Emergency department sonographic measurement of optic nerve sheath diameter to detect findings of increased intracranial pressure in adult head injury patients. Ann Emerg Med. 2007 Apr;49(4):508-14. Epub 2006 Sep 25. PMID: 16997419.

OPHTHALMOLOGY BEFUDDLER
Chris is an Intensivist and ECMO specialist at The Alfred ICU, where he is Deputy Director (Education). He is a Clinical Adjunct Associate Professor at Monash University, the Lead for the Clinician Educator Incubator programme, and a CICM First Part Examiner.
He is an internationally recognised Clinician Educator with a passion for helping clinicians learn and for improving the clinical performance of individuals and collectives. He was one of the founders of the FOAM movement (Free Open-Access Medical education) has been recognised for his contributions to education with awards from ANZICS, ANZAHPE, and ACEM.
His one great achievement is being the father of three amazing children.
On Bluesky, he is @precordialthump.bsky.social and on the site that Elon has screwed up, he is @precordialthump.
| INTENSIVE | RAGE | Resuscitology | SMACC
