Trigeminal autonomic cephalalgias
The trigeminal autonomic cephalalgias
We’ve already looked at cluster headaches, but there are three other trigeminal autonomic cephalalgias you should be familiar with:
- Paroxysmal hemicrania
- Hemicrania continua
- Short-lasting unilateral neuralgiform headaches with conjunctival injection and tearing (SUNCT)
Similar to cluster headaches, all of the trigeminal autonomic cephalalgias involve moderate to severe unilateral pain of the head or face and have features of autonomic nervous system activation.
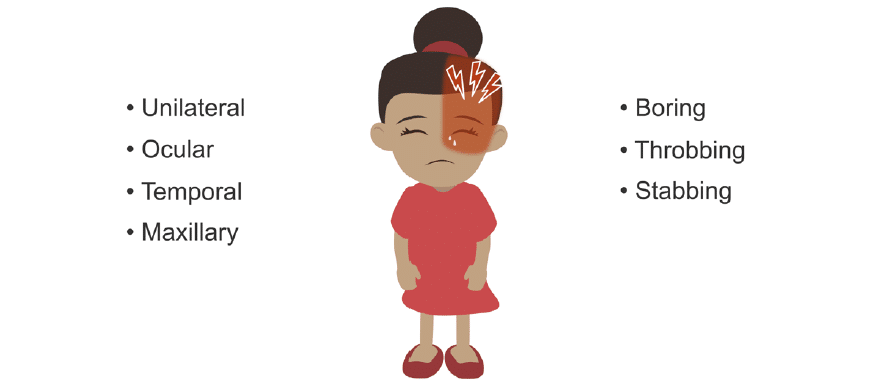
Paroxysmal hemicrania
Paroxysmal hemicrania affect females more than males (2:1) and is characterized by frequent, severe, unilateral head pain, usually in the ocular, temporal, and maxillary regions. The pain may also radiate behind the eye and / or into the shoulder and arm on the ipsilateral side. The pain is usually described as boring, throbbing, or stabbing.
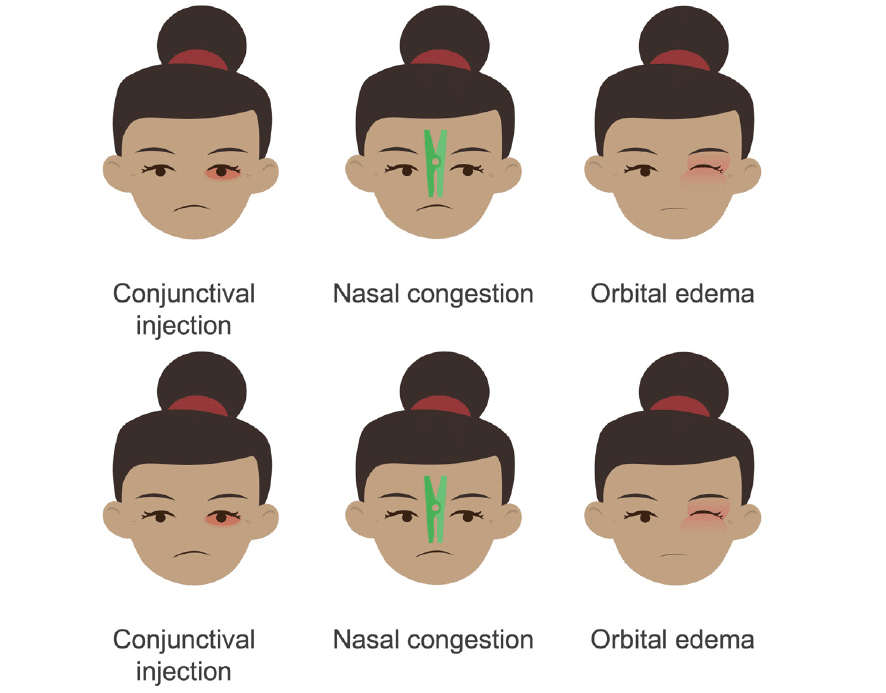
In this headache type, patients may also have trigeminal autonomic symptoms:
- Conjunctival injection
- Nasal congestion
- Periorbital oedema
- Miosis and / or ptosis (not necessary for diagnosis)
- Agitation or restlessness
There will be from 1 to 40 events daily, which may last from 2 to 120 minutes each, and these pain cycles occur in sudden attacks, which can last from one week to a year. Similar to cluster headaches, this syndrome has both episodic and chronic forms.
There are remissions in this disorder, but therapies for cluster headaches have no effect on paroxysmal hemicrania. However, paroxysmal hemicrania is responsive to indomethacin. Other non-steroidal anti-inflammatory drugs are not effective for these headaches.
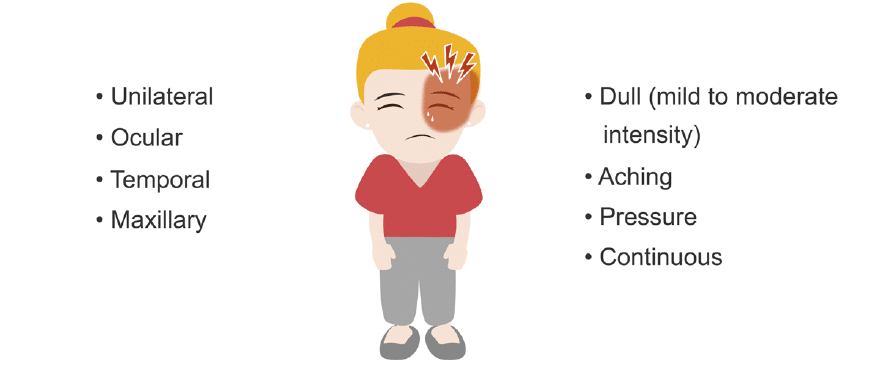
Hemicrania continua
Hemicrania continua headaches are unilateral, continuous, and have a mild to moderate intensity. There is a female predominance at a 2:1 ratio. Pain is generally not as severe as other headache types in this group. The pain is described as dull, aching, or pressure. It is ocular, temporal and / or maxillary in location. Events may last for 20 minutes.
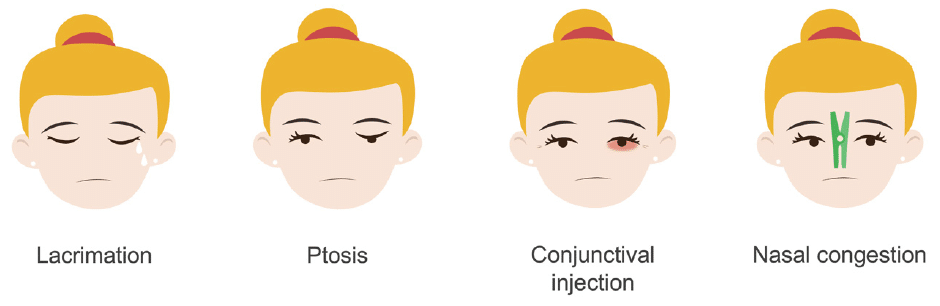
Like with other trigeminal autonomic cephalalgias there are autonomic phenomena you should watch for:
- Ipsilateral lacrimation
- Ptosis
- Conjunctival injection
- Nasal congestion
Similar to paroxysmal hemicrania, hemicrania continua can be treated with indomethacin.
SUNCT
Short-lasting unilateral neuralgiform headaches with conjunctival injection and tearing (SUNCT).
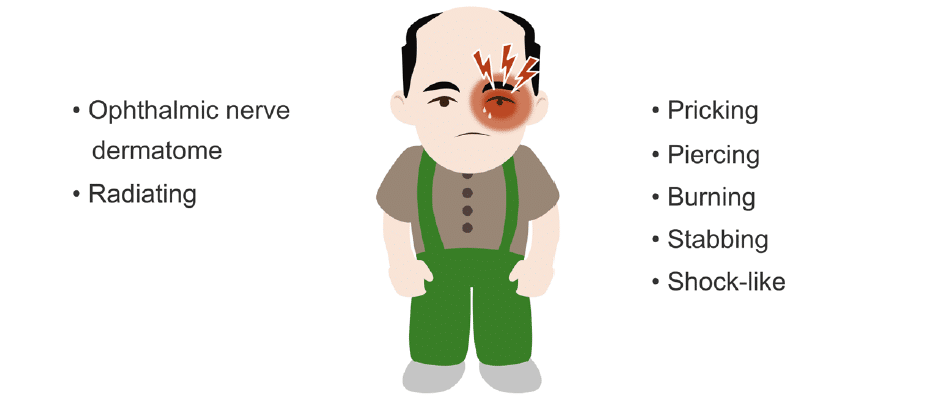
These headaches are the rarest of the trigeminal autonomic cephalalgias. The pain often affects the region innervated by the ophthalmic division of the trigeminal nerve, but may also occur with radiation into the forehead, temple, nose, cheek, palate, and even the periauricular region and the occiput.
The pain is pricking, piercing, burning, stabbing, or shock-like.
Although not present in all patients with SUNCT, there are four associated trigeminal autonomic dysfunctions you should be aware of:
- Ipsilateral conjunctival injection
- Lacrimation
- Nasal congestion
- Periorbital oedema
The headaches are very brief: pain maximizes very rapidly (in seconds), lasts for 5 to 250 seconds, and recurs multiple times a day.
Symptomatic periods last several days to months, with pain occurring once to 80 times a day, with an average of 30 episodes a day. Many patients say they have a dull pain between episodes.
The cycling of pain paroxysms with remissions is erratic in this disorder.
SUNCT can be episodic, with recurrences over seven days to a year but with pain free periods of at least three months. It is considered to be chronic when remissions last less than three months.
Since the individual episodes of pain are short-lived, treatment is usually focused on prevention. Drugs used include anticonvulsants such as lamotrigine, topiramate, gabapentin, and carbamazepine. Intravenous therapy (IV) lidocaine can abort a severe, frequently occurring event.
This is an edited excerpt from the Medmastery course Headache Masterclass by Robert Coni, DO, EdS, FAAN. Acknowledgement and attribution to Medmastery for providing course transcripts.
- Coni R. Headache Masterclass. Medmastery
- Coni R. Clinical Neurology Essentials. Medmastery
- Simmonds GR. Neurology Masterclass: Managing Common Diseases. Medmastery
- Simmonds GR. Neurology Masterclass: Managing Emergencies. Medmastery
References
- The International Classification of Headache Disorders 3rd edition
- Rizzoli P, Mullally WJ. Headache. Am J Med. 2018 Jan;131(1):17-24.
- Goadsby PJ. Trigeminal autonomic cephalalgias. Continuum (Minneap Minn). 2012 Aug;18(4):883-95
- Burish M. Cluster Headache and Other Trigeminal Autonomic Cephalalgias. Continuum (Minneap Minn). 2018 Aug;24(4, Headache):1137-1156
Neurology Library: The primary headache disorders
- Coni R. Deconstructing headache classification. LITFL
- Coni R. Headache aetiology. LITFL
- Coni R. Migraine headache. LITFL
- Coni R. Tension headache. LITFL
- Coni R. Cluster headache. LITFL
- Coni R. Trigeminal autonomic cephalalgias. LITFL
- Coni R. Other primary headaches. LITFL
- Coni R. Chronic daily headaches. LITFL
Neurology Library
Robert Coni, DO, EdS, FAAN. Vascular neurologist and neurohospitalist and Neurology Subspecialty Coordinator at the Grand Strand Medical Center in South Carolina. Former neuroscience curriculum coordinator at St. Luke’s / Temple Medical School and fellow of the American Academy of Neurology. In my spare time, I like to play guitar and go fly fishing. | Medmastery | Linkedin |
BMBS (The University of Nottingham) BMedSci (The University of Nottingham). Emergency Medicine RMO at Sir Charles Gairdner Hospital Perth, WA. Interested in Medical Education and Emergency Medicine. Swimmer and frequent concert attendee.


