Other primary headaches
Classifying other primary headache disorders
In addition to migraine, tension-type headache and trigeminal autonomic cephalalgias, the International Headache Society includes a fourth category of primary headache disorders. This group of primary headache disorders are a disparate group that may not have common characteristics. Some of these headaches even have secondary causes.
There are eight entities that fall into the category of other primary headaches:
- Stabbing headache
- Cough headache
- Exertional headache
- Headache with sexual activity
- Daily persistent headache
- Nummular headache
- Hypnic headache
- Thunderclap headache
Similar to cluster headaches, all of the trigeminal autonomic cephalalgias involve moderate to severe unilateral pain of the head or face and have features of autonomic nervous system activation.
Stabbing headache
Stabbing headaches are also called ice-pick headaches due to the type of pain experienced—described as sharp, pricking, or stabbing. These headaches are associated with spontaneous, paroxysmal attacks of fleeting head pain.
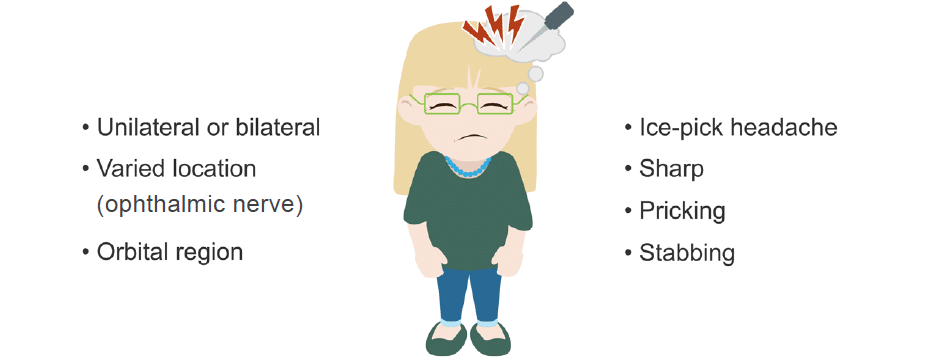
In general, these headaches occur irregularly but when they do occur, the pain lasts from one to ten seconds and the attacks range from rare to ≥ 50 per day.
These headaches usually respond to indomethacin.
Cough headache
As their name suggests, these headaches occur from coughing or performing the Valsalva manoeuvre.
Cough headaches are often described as sudden in onset and severe, reaching maximum intensity immediately. Because of this, patients may consider this headache ominous. The pain may last from a few seconds to minutes but may be present for up to two hours.
It is prudent to obtain a scan to exclude a structural abnormality such as a tumour in patients with this syndrome. Type 1 Arnold-Chiari malformations may be present in patients with cough headaches.
Treatment for cough headache includes indomethacin, diamox, and other nonsteroidal anti-inflammatory drugs. They preferentially affect men over the age of 40.
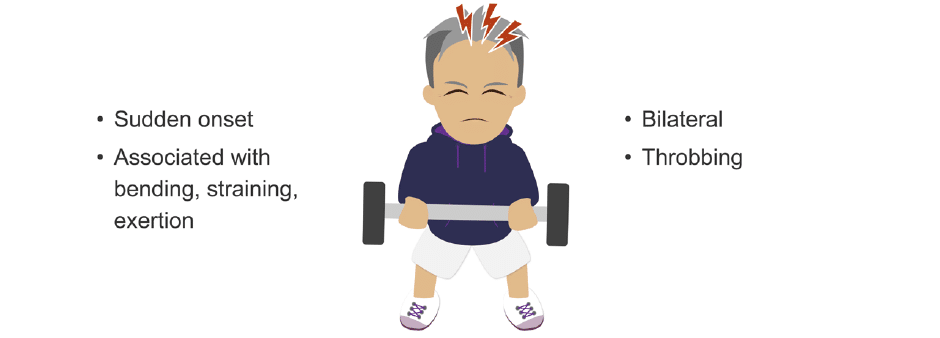
Exertional headache
True to their name, these headaches are associated with bending, straining, or effort such as physical exercise. They are sudden in onset and bilateral and throbbing in nature. These headaches generally resolve quickly but sometimes can last for a few days.
The first time this sudden onset headache presents, subarachnoid haemorrhage (SAH) should be suspected. All patients with exertional headache should have imaging to rule out SAH and posterior fossa abnormalities such as Arnold-Chiari malformation, neoplasm, and haematoma etc.
Treatment for exertional headaches includes non-steroidal anti-inflammatory drugs (NSAIDs) and indomethacin. Propranolol is sometimes helpful. Patients can be told to pre-treat before strenuous workouts with an NSAID.
Headache with sexual activity
These headaches are often referred to as orgasmic headaches or postcoital headaches due to the fact that the headache often occurs either at the time of orgasm, or just before. The cause is unknown. The headache is described as sudden in onset and explosive but with pain that is duller in nature. Sometimes there is radiation to the jaw and neck. These headaches affect men more than women.
Non-steroidal anti-inflammatory drugs, indomethacin and triptans, taken before sexual relations may help.
Daily persistent headache
This is a recently recognised syndrome and refers to a daily, unremitting headache pain which has features of both migraine and tension headache. It is usually bilateral, pressure-like and of mild to moderate intensity, without worsening during activity. It may be accompanied by nausea, photophobia and phonophobia. The daily persistent headache develops either acutely or over several days; those affected can clearly recall the onset date, and this has become part of the criteria.
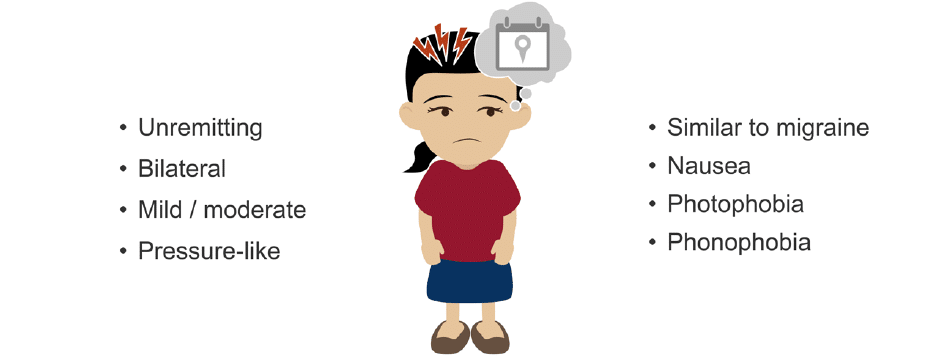
To diagnose a new daily persistent headache, the headache must be continuously present for more than three months. The headache pain occurs within a 24-hour period and is thereafter unremitting.
This headache does not respond to treatment.
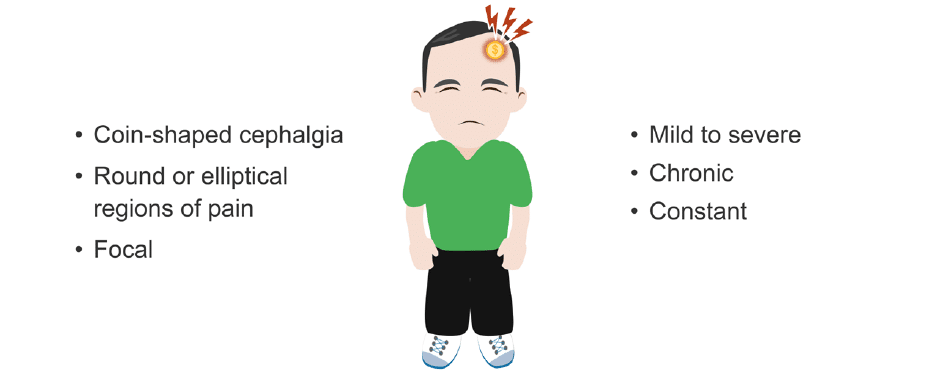
Nummular headache
A nummular headache is characterized by a focal circumscribed area of variable mild to severe pain, with occasional sensory disturbances. These regions are generally round or elliptical and measure from one to six cm in diameter; they are fixed in size, shape, and location.
Due to the shape of the pain distribution, this headache is also referred to as coin-shaped cephalgia. The pain within these regions is chronic, constant and can worsen. The cause is unknown but may be due to irritation of sensory nerve endings in a region.
Botulinum toxin (botox) injected over the region of pain may help many patients. Oral prophylactic medicines, such as amitriptyline, can also be used.
Hypnic headache
These are sleep-related headaches, also referred to as alarm clock headaches. They occur at nearly the same time each night, usually between 01:00 and 03:00. They can also occur during daytime naps. They resolve in 15 minutes to three hours.
Hypnic headaches are abrupt, throbbing, and involve the whole head (holocranial). Headache frequency is high, with four or more attacks per week in those affected.
These headaches begin later in life and involve women more than men. Treatment is with topiramate, indomethacin, and lithium.
Thunderclap headache
Thunderclap headaches can be a primary headache disorder or secondary to a medical cause. As a primary headache, thunderclap headaches have a very rapid onset of severe pain.
This is an edited excerpt from the Medmastery course Headache Masterclass by Robert Coni, DO, EdS, FAAN. Acknowledgement and attribution to Medmastery for providing course transcripts.
- Coni R. Headache Masterclass. Medmastery
- Coni R. Clinical Neurology Essentials. Medmastery
- Simmonds GR. Neurology Masterclass: Managing Common Diseases. Medmastery
- Simmonds GR. Neurology Masterclass: Managing Emergencies. Medmastery
References
- The International Classification of Headache Disorders 3rd edition
- Rizzoli P, Mullally WJ. Headache. Am J Med. 2018 Jan;131(1):17-24.
- Goadsby PJ. Trigeminal autonomic cephalalgias. Continuum (Minneap Minn). 2012 Aug;18(4):883-95
- Burish M. Cluster Headache and Other Trigeminal Autonomic Cephalalgias. Continuum (Minneap Minn). 2018 Aug;24(4, Headache):1137-1156
Neurology Library: The primary headache disorders
- Coni R. Deconstructing headache classification. LITFL
- Coni R. Headache aetiology. LITFL
- Coni R. Migraine headache. LITFL
- Coni R. Tension headache. LITFL
- Coni R. Cluster headache. LITFL
- Coni R. Trigeminal autonomic cephalalgias. LITFL
- Coni R. Other primary headaches. LITFL
- Coni R. Chronic daily headaches. LITFL
Neurology Library
Robert Coni, DO, EdS, FAAN. Vascular neurologist and neurohospitalist and Neurology Subspecialty Coordinator at the Grand Strand Medical Center in South Carolina. Former neuroscience curriculum coordinator at St. Luke’s / Temple Medical School and fellow of the American Academy of Neurology. In my spare time, I like to play guitar and go fly fishing. | Medmastery | Linkedin |
BMBS (The University of Nottingham) BMedSci (The University of Nottingham). Emergency Medicine RMO at Sir Charles Gairdner Hospital Perth, WA. Interested in Medical Education and Emergency Medicine. Swimmer and frequent concert attendee.


