Activate or Wait – 003
58 year-old man with one week of pleuritic chest pain and shortness of breath. Background of previous pericarditis, no other cardiac risk factors. BP 135/75.
ETA 10 minutes.
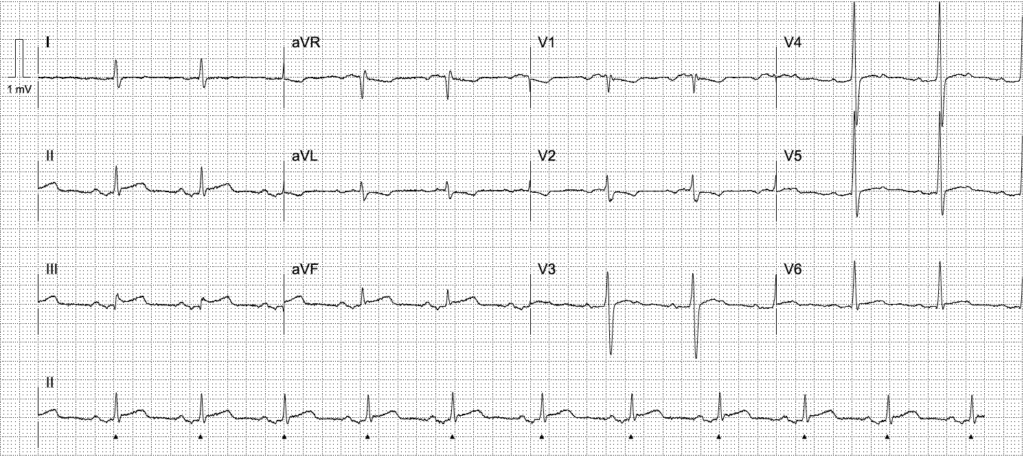
ECG interpretation
- Inferior ST elevation in leads II, III, aVF
- Reciprocal ST depression and TWI in aVL, V1-2
- Downsloping TP segment in V3-5 (Spodick sign)
Despite the history, this should be assumed to represent inferior OMI until angiography proves otherwise. Pericarditis virtually never has reciprocal ST depression except in aVR, and is a relatively rare diagnosis compared to OMI – the pre-test probably of pericarditis in this age group is low. In addition, ST elevation seen here is not diffuse, and there is hardly any PR depression (most specific sign of pericarditis). Remember, you diagnose pericarditis at your own peril.
AI interpretation by PMcardio

PMcardio’s AI ECG model identified a STEMI/STEMI equivalent. The explainability feature offers insights into problematic patterns in the respective leads, providing a clear rationale for the diagnosis.
Further reading
Outcome
The cath lab was not activated prior to arrival. The patient was reviewed in ED by the cardiology team and taken to emergent angiography due to concern for ECG findings.
Key Finding:
No obstructive coronary artery disease. Likely myocarditis.
Findings:
- Left Main Coronary Artery – normal
- Left Anterior Descending Coronary Artery – Type III vessel. Mild coronary plaque proximal vessel. Mild diffuse disease throughout remainder of vessel
- Left Circumflex Coronary Artery – mild diffuse disease. Moderate marginal disease.
- Right Coronary Artery – large dominant vessel. Mild diffuse disease
- Left Ventriculogram – normal systolic function
Plan:
1. Serial troponins
2. Transthoracic echocardiogram
3. Ongoing aggressive cardiovascular risk factor management
4. Admit CCU
Clinical Pearls
Initial troponin sent shortly after arrival returned markedly elevated and later peaked in the thousands. There are two differentials for a patient with this presentation and a normal angiogram – myocarditis and MINOCA (myocardial infarction with non-obstructive coronary arteries).
- MINOCA can occur if the artery spontaneously reperfuses prior to the time of angiogram. The diagnosis of myocarditis can be made by cardiac MRI, or an ECG showing that ST elevation was still present at the time of angiography.
- ECG changes in myocarditis can be localised and produce ST segment and T wave changes that are indistinguishable from acute coronary occlusion. Angiography is required in cases of acute presentation such as this.
References
Further reading
- Witting MD, Hu KM, Westreich AA, Tewelde S, Farzad A, Mattu A. Evaluation of Spodick’s Sign and Other Electrocardiographic Findings as Indicators of STEMI and Pericarditis. J Emerg Med. 2020 Apr;58(4):562-569.
- Bischof JE, Worrall C, Thompson P, Marti D, Smith SW. ST depression in lead aVL differentiates inferior ST-elevation myocardial infarction from pericarditis. Am J Emerg Med. 2016 Feb;34(2):149-54.
- Burn E, Buttner R. Pericarditis. LITFL
Online resources
- Wiesbauer F, Kühn P. ECG Mastery: Yellow Belt online course. Understand ECG basics. Medmastery
- Wiesbauer F, Kühn P. ECG Mastery: Blue Belt online course: Become an ECG expert. Medmastery
- Kühn P, Houghton A. ECG Mastery: Black Belt Workshop. Advanced ECG interpretation. Medmastery
- Rawshani A. Clinical ECG Interpretation ECG Waves
- Smith SW. Dr Smith’s ECG blog.
ACTIVATE or WAIT
EKG Interpretation
MBBS DDU (Emergency) CCPU. Adult/Paediatric Emergency Medicine Advanced Trainee in Melbourne, Australia. Special interests in diagnostic and procedural ultrasound, medical education, and ECG interpretation. Co-creator of the LITFL ECG Library. Twitter: @rob_buttner
Dr. Stephen W. Smith is a faculty physician in the Emergency Medicine Residency at Hennepin County Medical Center (HCMC) in Minneapolis, MN, and Professor of Emergency Medicine at the University of Minnesota. Author of Dr Smith's ECG Blog | Bibliography | X |
Dr. Robert Herman is the Co-founder and Chief Medical Officer of PMcardio by Powerful Medical. He is a cardiovascular researcher at the Cardiovascular Center Aalst in Belgium, specializing in applying AI to enhance the detection and referral of cardiovascular patients. LinkedIn | X (formerly Twitter) | Get in Touch




Excellent, but truly a difficult ECG case! I answered “activate” on this one, thinking that the T wave inversion in aVL was a reciprocal change. I also find the ST segments to be not so concave. Great case to learn from!