Activate or Wait – 004
86 year-old woman with two hours of dull chest pain and dizziness. Ex-smoker with hypertension and dyslipidaemia.
ETA 20 minutes.
ECG interpretation
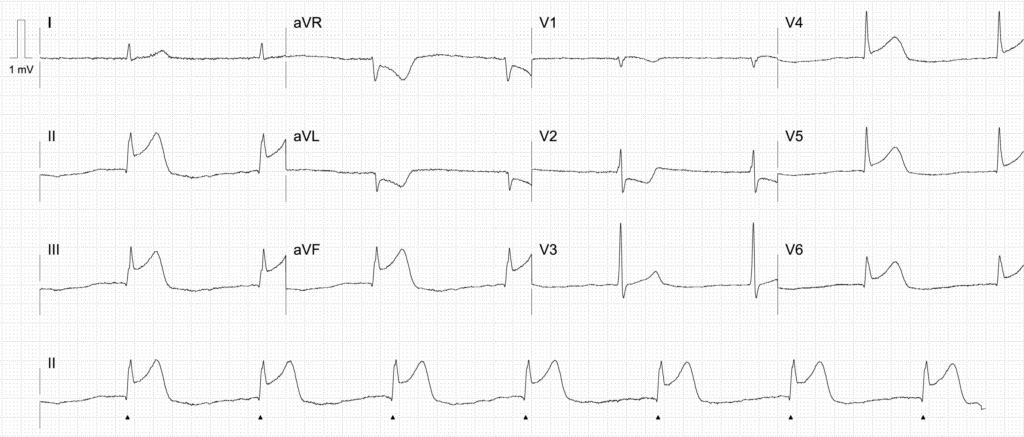
Inferolateral OMI complicated by junctional bradycardia and RV infarction
- Marked inferolateral ST elevation in leads II, III, aVF and V4-V6
- Reciprocal ST depression in aVR, aVL and V2
- Hyperacute T-waves seen inferiorly
- There is a touch of ST elevation in V1. With the ST depression in V2, one would also expect ST depression in V1. However, something is “pulling up” the ST segment here – this suggests RV infarction
- Junctional bradycardia with a heart rate of 42 beats per minute
The presence of widespread inferolateral ST elevation and anterior ST depression indicates a large territory right coronary artery (RCA) infarct affecting the inferior, lateral, and posterior walls.
Junctional bradycardia is likely due to a combination of:
- Sinus node dysfunction due to impaired blood flow via the sinoatrial nodal artery, which arises from the proximal RCA in 60% of people
- Vagal effects of an inferior STEMI (the Bezold-Jarisch reflex). Atropine is usually effective in these cases
The extent of the ST changes, and the presence RV infarction and junctional bradycardia suggests proximal RCA occlusion and a higher risk case.
Note that the terms junctional bradycardia and junctional escape rhythm are synonymous, simply referring to an escape rhythm arising at the AV node. Because the rate of spontaneous depolarisation at the level of the AV node is usually 40-60 bpm, this is often a bradyarrhythmia.
AI interpretation by PMcardio

PMcardio’s AI ECG model identified a STEMI/STEMI equivalent.
The explainability feature offers insights into problematic patterns in the respective leads, providing a clear rationale for the diagnosis.
Further reading
Outcome
Key Finding:
Proximal right coronary artery (RCA) occlusion with thrombus.
Findings:
- Left Main Coronary Artery — normal
- Left Anterior Descending Coronary Artery — mild coronary artery disease
- Left Circumflex Coronary Artery — normal
- Right Coronary Artery — proximal occlusion with thrombus
Plan:
- Proximal RCA occlusion with thrombus
- Proceed to percutaneous coronary intervention of proximal RCA.
Clinical Pearls
- Suspect RV infarction in inferior OMI if there is ST depression in V2, with an isoelectric ST segment or ST elevation in V1. This suggests there is something “pulling up” the ST segment in V1, which is a rightward facing lead.
- RV infarction occurs about 25% of the time in proximal RCA occlusion, as there are often collaterals from the LAD to the RV. However, its presence indicates a proximal occlusion with a large infarct territory and high risk of bradyarrhythmias. These patients are preload dependent and can have significant deterioration with administration of nitrates. Administer fluids and anticipate the need for medical or mechanical pacing.
- Bradyarrhythmias are common in inferior MI due to impaired blood flow via the sinoatrial nodal artery and/or AV nodal artery. Atropine is often effective. The presence of sinus node dysfunction (sinus bradycardia, sinuses pauses, junctional bradycardia) indicates a more proximal RCA or left circumflex occlusion and a higher risk patient.
References
Further reading
- Smith SW. The resident made the diagnosis immediately. The faculty was not as certain. Dr Smith’s ECG blog.
- Buttner R, Burns E. Inferior STEMI. LITFL
- Nickson C. STEMI Management. LITFL
Online resources
- Wiesbauer F, Kühn P. ECG Mastery: Yellow Belt online course. Understand ECG basics. Medmastery
- Wiesbauer F, Kühn P. ECG Mastery: Blue Belt online course: Become an ECG expert. Medmastery
- Kühn P, Houghton A. ECG Mastery: Black Belt Workshop. Advanced ECG interpretation. Medmastery
- Smith SW. Dr Smith’s ECG blog.
- Rawshani A. Clinical ECG Interpretation ECG Waves
ACTIVATE or WAIT
EKG Interpretation
MBBS DDU (Emergency) CCPU. Adult/Paediatric Emergency Medicine Advanced Trainee in Melbourne, Australia. Special interests in diagnostic and procedural ultrasound, medical education, and ECG interpretation. Co-creator of the LITFL ECG Library. Twitter: @rob_buttner
Dr. Stephen W. Smith is a faculty physician in the Emergency Medicine Residency at Hennepin County Medical Center (HCMC) in Minneapolis, MN, and Professor of Emergency Medicine at the University of Minnesota. Author of Dr Smith's ECG Blog | Bibliography | X |
Dr. Hana Hybasek Dzurikova, MRCVS, PGCert MEd is a medical educator driving innovation and change in health professions education through technology-enhanced learning.




Does anyone have any explanation as to how the lateral leads get ST elevation when the RCA is occluded? Does the RCA somehow provide perfusion to the lateral wall as well? Thanks.