Airway Ultrasound
Ultrasound (US) is an accessible, non-invasive portable imaging modality which has utility in upper airway assessment.
Uses in critical care:
- Airway size and prediction of required ETT size
- Prediction of difficult laryngoscopy
- Airway device placement and depth (including confirmation of adequate ventilation with bilateral lung sliding)
- Assisting with placement of surgical airway
- Predicting post-extubation stridor or failure
- Evaluation of the epiglottis
Advantages:
- US readily available in most critical care settings
- Non-invasive with no radiation and minimal discomfort
- Quick and easy to perform
Disadvantages:
- Inter-operator variability
- Still not accepted as gold standard in many institutions for uses such as confirmation of ETT placement
- Lack of validated cut-off values for use in predicting difficult laryngoscopy or predicting post-extubation stridor/failure
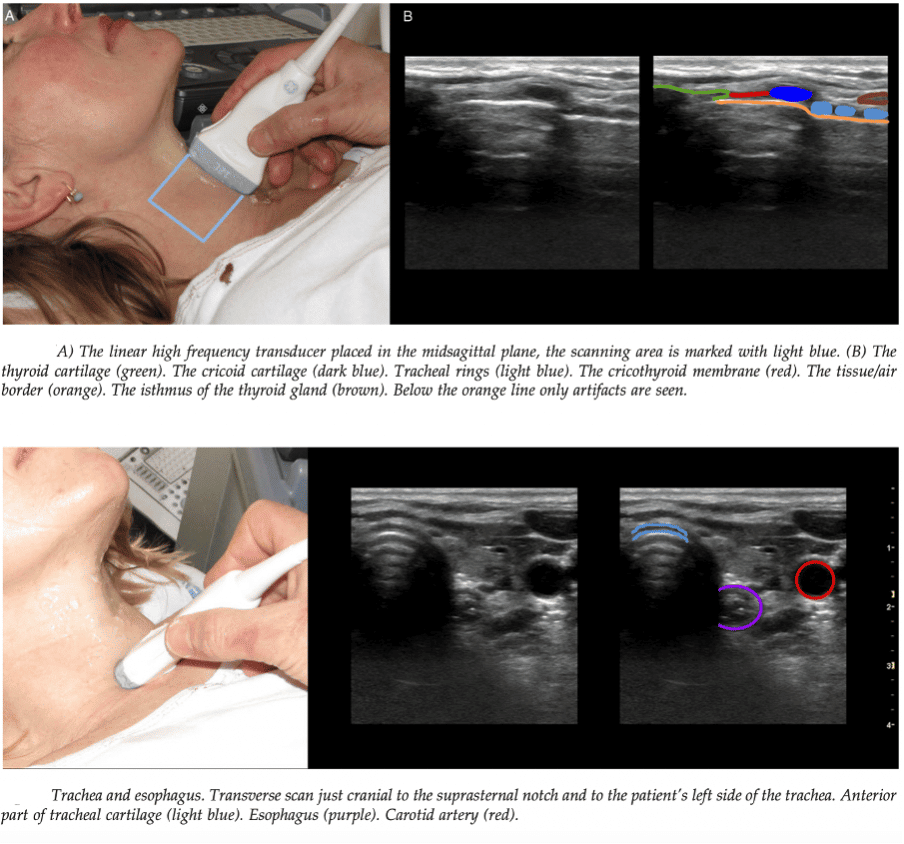
Overview of common ultrasound upper airway views:
For summary of US airway views, see LITFL US airway pages
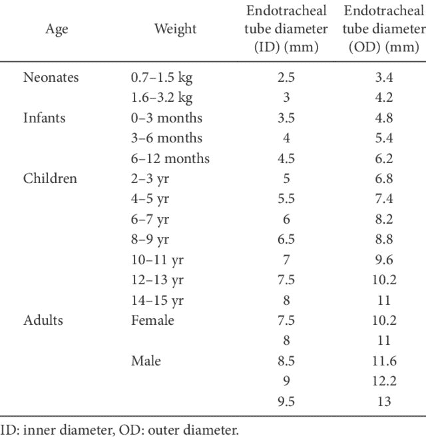
Airway size and prediction of required ETT size:
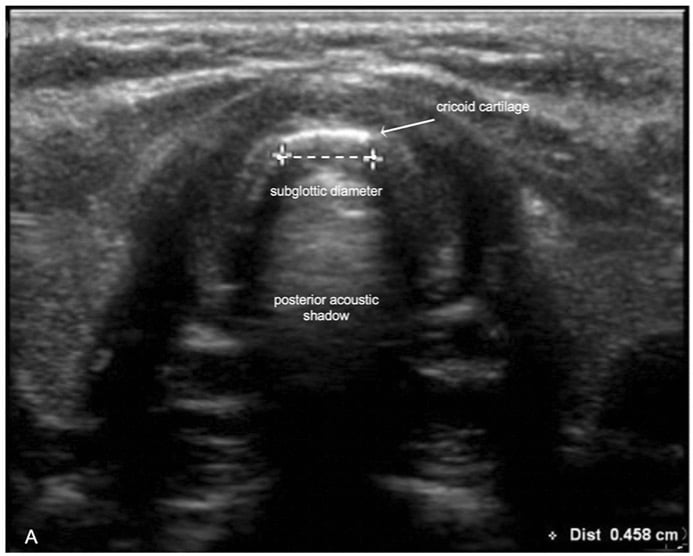
- The narrowest diameter of the subglottic upper airway in healthy adults is the width of the air-column at the level of the cricoid cartilage. (7)
- The selected ETT size should take into account the narrowest diameter of airway in order to minimise incidence of complications such as tracheal wall ischaemia, ulceration or necrosis, tracheal stenosis, and recurrent laryngeal nerve injury.
- Subglottic diameter at lower edge of cricoid cartilage can be measured and used to predict appropriate ETT size with better accuracy than age and/or weight-based formulae. (6)
- The outer diameter of the ‘best-fit’ ETT should be less than the subglottic diameter at the cricoid level by 0.1-1.7 mm. (9)
Prediction of difficult laryngoscopy:
Multiple different approaches to using US to predict difficult laryngoscopy:
- Ability to visualize hyoid bone on sublingual ultrasound is strongly associated with laryngoscopic Cormack-Lehane grading scale of 1-2. (11)
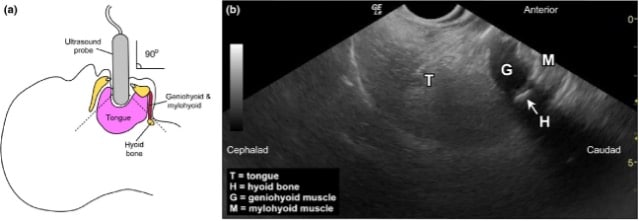
(b) Representative ultrasound image showing view of the hyoid bone.
Hui CM, Tsui BC. Sublingual ultrasound as an assessment method for predicting difficult intubation: a pilot study. Anaesthesia. 2014 Apr;69(4):314-9
Other useful measures to predict difficult laryngoscopy:
- Distance from anterior neck skin surface to epiglottis
- Distance from anterior neck skin surface to hyoid bone
- Hyomental distance
- Hyomental distance ratio
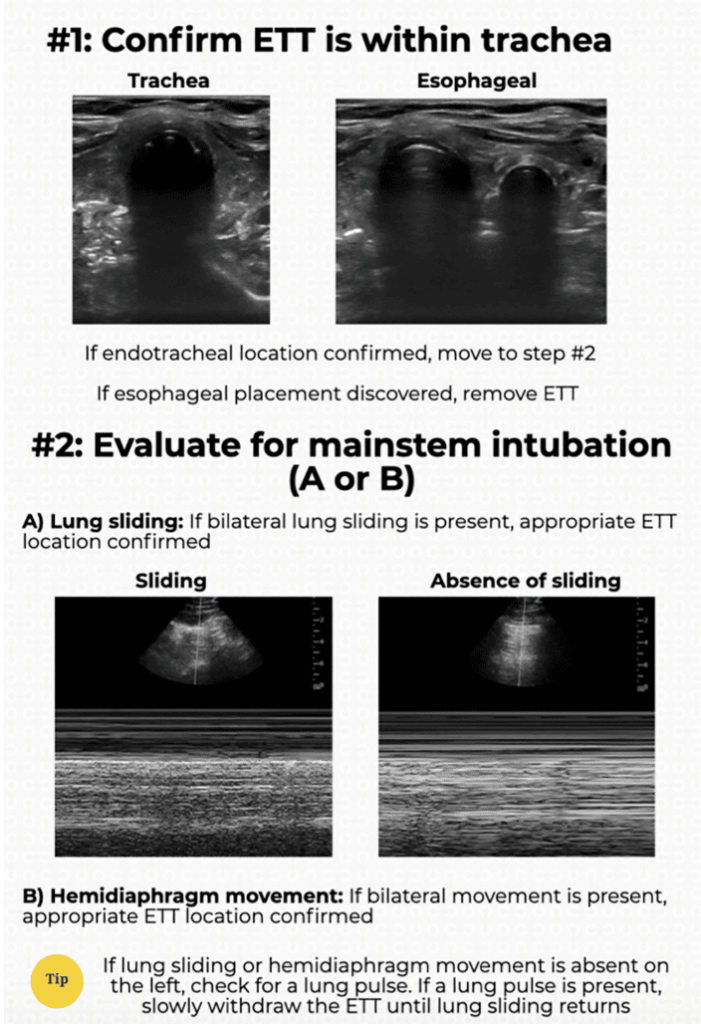
Airway device placement and depth:
- Ultrasound of the anterior neck can be used real-time to directly observe an ETT being passed into the trachea, or an accidental oesophageal intubation.
- During intubation, curvilinear probe placed over cricothyroid membrane, angled 45˚ cranially (towards occiput) – very sensitive if performed during intubation
- Tracheal intubation seen as brief flutter deep to thyroid cartilage
- Oesophageal intubation seen as clear hyperechoic (bright white) curved line with shadowing – either side of, and deep to, the trachea.
- Advantage of immediately identifying oesophageal intubation prior to ventilation and thus accidental insufflation of stomach. Allows rapid removal of oesophageal ETT and reattempt at tracheal intubation.
- To assess ETT depth once tube determined to be in trachea, move probe to mid-axillary line to assess for bilateral lung sliding.
- If bilateral lung sliding present – suggests ETT in adequate position for ventilation.
- If unilateral lung sliding with contralateral lung pulse present – suggests intubation of main stem bronchus –-> slowly retract ETT until bilateral lung sliding is seen.
- Sensitivity of ultrasound to predict adequate ETT placement above 90% in most studies (including large meta-analyses). (13)
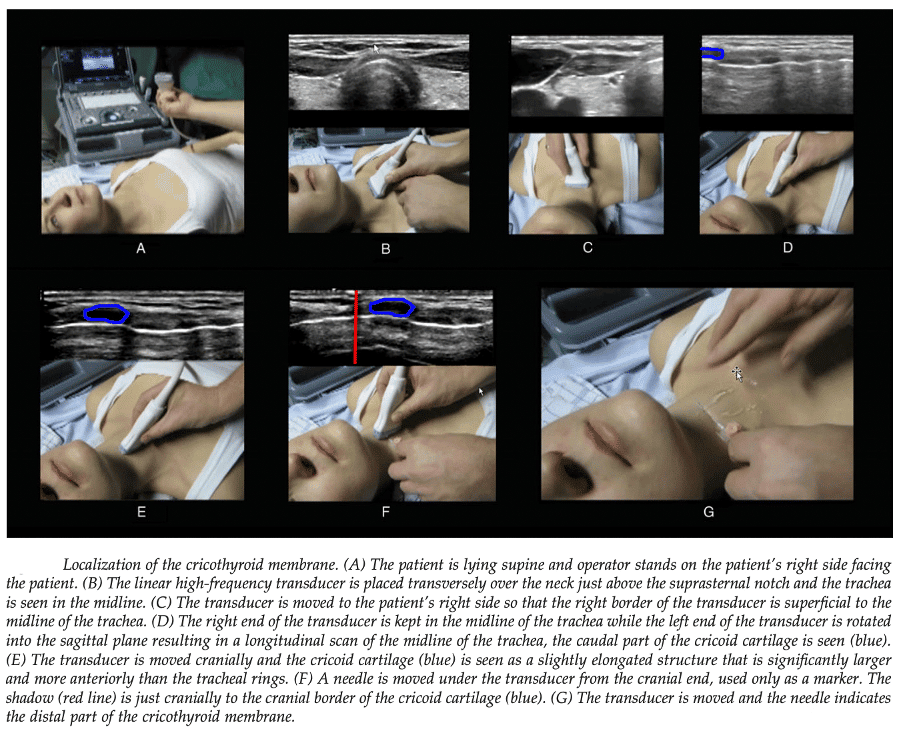
Assisting with placement of surgical airway:
See LITFL Surgical cricothyroidotomy and LITFL Can’t Intubate Can’t Oxygenate
- Ultrasound can be used to accurately identify cricothyroid membrane and any surrounding anatomical structures which may be at risk of injury from procedure.
Predicting post-extubation stridor:
- Some small studies suggest that by measuring air column width pre- and post-ETT cuff deflation, stridor post-extubation could be predicted with significant accuracy (5), although larger studies are required to determine robust quantitative cut-off points to predict post-extubation stridor.
Predicting post-extubation failure:
- Extubation outcome directly correlated with respiratory muscle endurance/strength
- Respiratory muscular strength can be directly observed by movement of diaphragm, and subsequent excursion of liver and spleen
- Measurement of liver and spleen displacement during spontaneous breathing trial prior to extubation can be helpful in predicting failure – with a cutoff of 1.1cm median displacement suggesting successful extubation with 81.8% positive predictive value. (4)
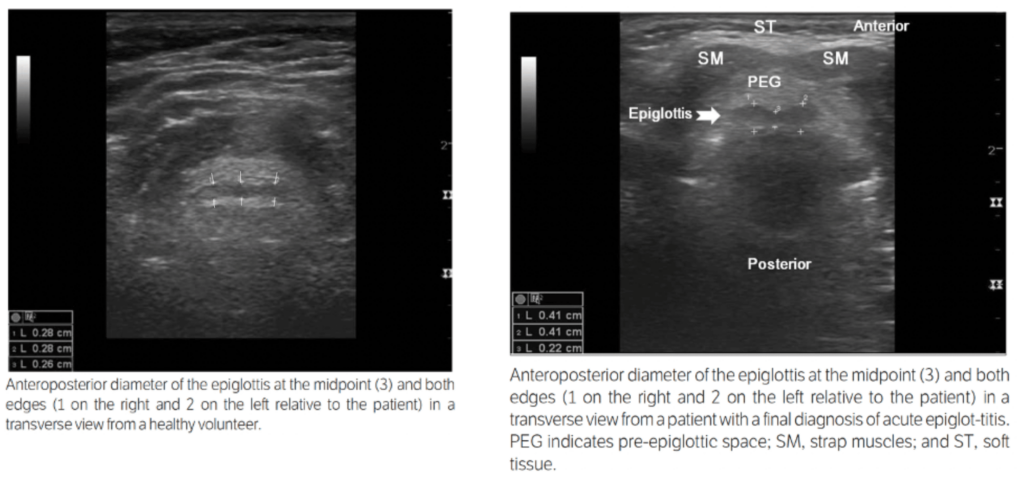
Evaluation of the epiglottis:
Utility in diagnosing epiglottitis:
- Linear probe placed on anterior neck at level of thyrohyoid membrane.
- Anteroposterior thickness of epiglottis at the midpoint, and the left and right edges is recorded.
- From a small Korean study (Ko et al., 2011), a cutoff of 3.2mm at both lateral edges is recorded as normal in healthy individuals, and patients with epiglottitis had lateral edges above 3.6mm thick. There was statistically significant difference and no overlap between these two groups.
- There was statistically significant difference between midpoint values as well, however there was overlap between thickness of healthy and affected individuals.
References
LITFL
- Rippey J. Airway Ultrasound – Ultrasound Library
- Rippey J. Airway ultrasound transverse views – Ultrasound Library
- Rippey J. Airway ultrasound longitudinal views – Ultrasound Library
- Rippey J. Airway ultrasound the oesophagus – Ultrasound Library
- Nickson C. Surgical Cricothyroidotomy
- Duller A., Nickson C. Can’t Intubate, Can’t Oxygenate
Publications
- Osman A, Sum KM. Role of upper airway ultrasound in airway management. J Intensive Care. 2016 Aug 15;4:52
- Šustić A. Role of ultrasound in the airway management of critically ill patients. Crit Care Med. 2007 May;35(5 Suppl):S173-7.
- Kristensen MS. Ultrasonography in the management of the airway. Acta Anaesthesiol Scand. 2011 Nov;55(10):1155-73 [PDF]
- Jiang JR, Tsai TH, Jerng JS, Yu CJ, Wu HD, Yang PC. Ultrasonographic evaluation of liver/spleen movements and extubation outcome. Chest. 2004 Jul;126(1):179-85
- Ding LW, Wang HC, Wu HD, Chang CJ, Yang PC. Laryngeal ultrasound: a useful method in predicting post-extubation stridor. A pilot study. Eur Respir J. 2006 Feb;27(2):384-9.
- Shibasaki M, Nakajima Y, Ishii S, Shimizu F, Shime N, Sessler DI. Prediction of pediatric endotracheal tube size by ultrasonography. Anesthesiology. 2010 Oct;113(4):819-24.
- Lakhal K, Delplace X, Cottier JP, Tranquart F, Sauvagnac X, Mercier C, Fusciardi J, Laffon M. The feasibility of ultrasound to assess subglottic diameter. Anesth Analg. 2007 Mar;104(3):611-4.
- Deekiatphaiboon C, Oofuvong M, Karnjanawanichkul O, Siripruekpong S, Bussadee P. Ultrasonography measurement of glottic transverse diameter and subglottic diameter to predict endotracheal tube size in children: a prospective cohort study. Sci Rep. 2022 Sep 8;12(1):15215.
- Al-Mazrou KA, Abdullah KM, Ansari RA, Abdelmeguid ME, Turkistani A. Comparison of the outer diameter of the ‘best-fit’ endotracheal tube with MRI-measured airway diameter at the cricoid level. Eur J Anaesthesiol. 2009 Sep;26(9):736-9
- Gupta B, Gupta L. Significance of the outer diameter of an endotracheal tube: a lesser-known parameter. Korean J Anesthesiol. 2019 Feb;72(1):72-73.
- Hui CM, Tsui BC. Sublingual ultrasound as an assessment method for predicting difficult intubation: a pilot study. Anaesthesia. 2014 Apr;69(4):314-9
- Gottlieb M, Alerhand S, Long B. Point-of-Care Ultrasound for Intubation Confirmation of COVID-19 Patients. West J Emerg Med. 2020 Aug 17;21(5):1042-1045.
- Congedi S, Savio F, Auciello M, Salvadori S, Nardo D, Bonadies L. Sonographic Evaluation of the Endotracheal Tube Position in the Neonatal Population: A Comprehensive Review and Meta-Analysis. Frontiers in Pediatrics, 2022; 10.
- Ko DR, Chung YE, Park I, Lee HJ, Park JW, You JS, Chung TN, Park YS, Chung SP, Kim S. Use of bedside sonography for diagnosing acute epiglottitis in the emergency department: a preliminary study. J Ultrasound Med. 2012 Jan;31(1):19-22.
[cite]

Critical Care
Compendium
Critical Care Trainee and Surgical Research Assistant, BMed (UNE/UoN). Clinical Associate Lecturer with the University of Sydney School of Medicine. Born and raised in Sydney but contemplating an escape to the country. Passion for simulation-based teaching, peri-operative research, and FOAMed. Enjoys trail running, gardening (edible stuff), and cooking (with edible stuff from garden).
Chris is an Intensivist and ECMO specialist at The Alfred ICU, where he is Deputy Director (Education). He is a Clinical Adjunct Associate Professor at Monash University, the Lead for the Clinician Educator Incubator programme, and a CICM First Part Examiner.
He is an internationally recognised Clinician Educator with a passion for helping clinicians learn and for improving the clinical performance of individuals and collectives. He was one of the founders of the FOAM movement (Free Open-Access Medical education) has been recognised for his contributions to education with awards from ANZICS, ANZAHPE, and ACEM.
His one great achievement is being the father of three amazing children.
On Bluesky, he is @precordialthump.bsky.social and on the site that Elon has screwed up, he is @precordialthump.
| INTENSIVE | RAGE | Resuscitology | SMACC

