Can’t Intubate, Can’t Oxygenate
OVERVIEW
Can’t Intubate, Can’t Oxygenate/Ventilate (CICO) scenarios are rare but critical airway emergencies which can quickly progress to severe hypoxia and death if not managed effectively by the healthcare team. There are many different approaches to the difficult or failed airway, all ultimately culminating in a last-line attempt at an emergency surgical airway (ESA)/front of neck access (FONA)/surgical cricothyroidotomy, or a needle cricothyroidotomy.
- Incidence of ~1:10,000 anaesthetics
- Call for help early
- Prepare for ESA/needle cricothyroidotomy, fibre-optic intubation (FOI), or blind nasal intubation
- Use emergency O2 flush if there is access to ventilator circuit, or high-flow oxygen through face mask
Note – Ultrasound can be used to assist with placement of surgical airway and quick assessment of successful intubation.
RECOGNISING A CICO SCENARIO
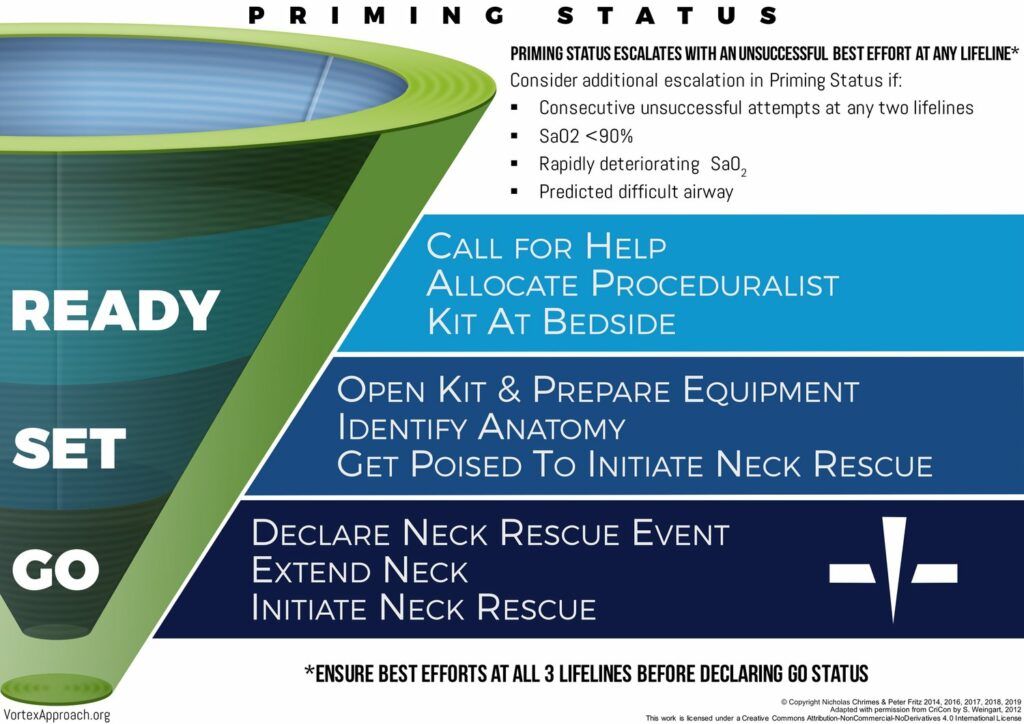
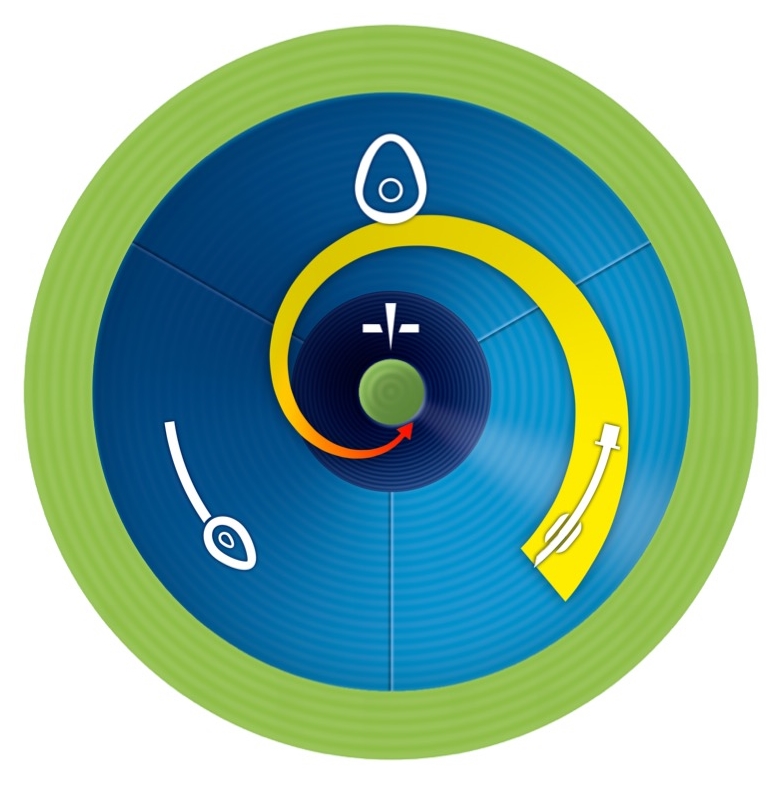
ANZCA in their Airway Management resources refer to a model devised by Dr Nick Chrimes called the ‘Vortex Approach’ for recognising and responding to a CICO scenario.
The Vortex Approach:
Note: The Vortex Approach advocates for a single phonetic pronunciation of ‘CICO’ as Ky-Koh to avoid misunderstanding.
- Aimed at all members of the team involved in potential difficult airways (critical care doctors, nurses, surgeons, paramedics, etc.).
- Applies to any clinical context which involves airway management.
- Preparing (or ‘Priming’) for a CICO scenario and eventual CICO Rescue during any airway management should be done simultaneously throughout attempts at Lifelines.
- As any airway difficulty progresses, CICO Status should be escalated. CICO Status should be escalated after an unsuccessful best effort at any lifeline, or earlier if anticipated possible difficult airway or deteriorating clinical picture.
- Dropping oxygen saturation or prolonged time attempting to establish an airway should immediately trigger simultaneous preparation for CICO Rescue.
RESPONDING TO A CICO SCENARIO
- 3 upper airway ‘Lifelines’ (ETT, LMA/SGA, Face Mask) followed by progression to CICO Rescue (also referred to as surgical airway).
- There should be a ‘best attempt’ at each upper airway Lifeline (in any order), after which if still unsuccessful, progression to surgical airway should immediately follow
- There should be no more than 3 attempts at each Lifeline, and something should be changed between each attempt to improve the chance of success
- 5 changes that can be made for each Lifeline:
- Manipulations
- Adjuncts
- Face mask: Guedel airway/Oropharyngeal airway (OPA), Nasopharyngeal airway (NPA)
- ETT: Fibre-optic intubation (FOI), Shikani optical stylet, video laryngoscopy, different laryngoscope blades
- Size/Type
- Suction/Increased flow
- Muscle tone
- After each ‘best attempt’ at an upper airway Lifeline, declare this out loud so that all members of the team are aware.
- Once a best attempt has been made at all 3 Lifelines, proceed immediately to CICO Rescue (surgical airway).
- Note: SpO2 is not a factor in the decision to proceed to CICO Rescue, as although SpO2 may demonstrate adequate oxygenation, it cannot evaluate safe apnoea time or physiological oxygen reserve which is likely fast depleting. Oxygen saturations are an important consideration, however, in making the context-specific decision as to when a ‘best effort’ at a Lifeline has been made. For example, if SpO2 is critically low, the airway team may make the decision to only have one ‘best attempt’ at each lifeline before moving to the next Lifeline or to CICO Rescue.
References and Links
CCC Airway Series
Emergencies: Can’t Intubate, Can’t Intubate, Can’t Oxygenate (CICO), Laryngospasm, Surgical Cricothyroidotomy
Conditions: Airway Obstruction, Airway in C-Spine Injury, Airway mgmt in major trauma, Airway in Maxillofacial Trauma, Airway in Neck Trauma, Angioedema, Coroner’s Clot, Intubation of the GI Bleeder, Intubation in GIH, Intubation, hypotension and shock, Peri-intubation life threats, Stridor, Post-Extubation Stridor, Tracheo-esophageal fistula, Trismus and Restricted Mouth Opening
Pre-Intubation: Airway Assessment, Apnoeic Oxygenation, Pre-oxygenation
Paediatric: Paediatric Airway, Paeds Anaesthetic Equipment, Upper airway obstruction in a child
Airway adjuncts: Intubating LMA, Laryngeal Mask Airway (LMA)
Intubation Aids: Bougie, Stylet, Airway Exchange Catheter
Intubation Pharmacology: Paralytics for intubation of the critically ill, Pre-treatment for RSI
Laryngoscopy: Bimanual laryngoscopy, Direct Laryngoscopy, Suction Assisted Laryngoscopy Airway Decontamination (SALAD), Three Axis Alignment vs Two Curve Theory, Video Laryngoscopy, Video Laryngoscopy vs. Direct
Intubation: Adverse effects of endotracheal intubation, Awake Intubation, Blind Digital Intubation, Cricoid Pressure, Delayed sequence intubation (DSI), Nasal intubation, Pre-hospital RSI, Rapid Sequence Intubation (RSI), RSI and PALM
Post-intubation: ETT Cuff Leak, Hypoxia, Post-intubation Care, Unplanned Extubation
Tracheostomy: Anatomy, Assessment of swallow, Bleeding trache, Complications, Insertion, Insertion timing, Literature summary, Perc. Trache, Perc. vs surgical trache, Respiratory distress in a trache patient, Trache Adv. and Disadv., Trache summary
Misc: Airway literature summaries, Bronchoscopic Anatomy, Cuff Leak Test, Difficult airway algorithms, Phases of Swallowing
Journal articles
- Heard AM, Green RJ, Eakins P. The formulation and introduction of a ‘can’t intubate, can’t ventilate’ algorithm into clinical practice. Anaesthesia. 2009;64:(6)601-8. [pubmed] [full text]
FOAM and web resources
- Keith Greenland on ‘Emergency Surgical Airway: Facts and Fiction’ (video lecture)
- ANZCA CPD Handbook, Appendix 12. Available from: https://www.anzca.edu.au/getattachment/eef6dd32-fe98-4230-8e2f-b32f20cdab30/Appendix-12-Can-t-Intubate,-Can-t-Oxygenate-(CICO)
- Chrimes N. The Vortex approach to airway management [Internet].
Critical Care
Compendium
Critical Care Trainee and Surgical Research Assistant, BMed (UNE/UoN). Clinical Associate Lecturer with the University of Sydney School of Medicine. Born and raised in Sydney but contemplating an escape to the country. Passion for simulation-based teaching, peri-operative research, and FOAMed. Enjoys trail running, gardening (edible stuff), and cooking (with edible stuff from garden).
Chris is an Intensivist and ECMO specialist at The Alfred ICU, where he is Deputy Director (Education). He is a Clinical Adjunct Associate Professor at Monash University, the Lead for the Clinician Educator Incubator programme, and a CICM First Part Examiner.
He is an internationally recognised Clinician Educator with a passion for helping clinicians learn and for improving the clinical performance of individuals and collectives. He was one of the founders of the FOAM movement (Free Open-Access Medical education) has been recognised for his contributions to education with awards from ANZICS, ANZAHPE, and ACEM.
His one great achievement is being the father of three amazing children.
On Bluesky, he is @precordialthump.bsky.social and on the site that Elon has screwed up, he is @precordialthump.
| INTENSIVE | RAGE | Resuscitology | SMACC

