Another Poke in the Eye
aka Ophthalmology Befuddler 032
A 57 year-old man presents to the emergency department after being accidentally poked in his left eye by his grandson. He complains of sharp pain on the surface of his eye and photophobia. He refuses to open his eyelids until you instill a few drops of topical anesthesia.
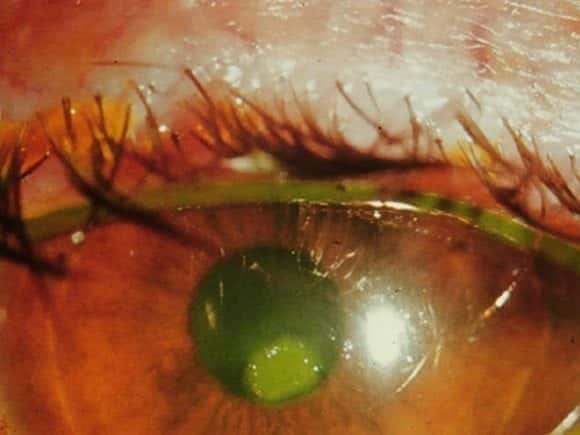
This is what you see after applying fluorescein to the eye:
Questions
Q1. What is shown?
Answer and interpretation
Corneal abrasion — there is an epithelial defect that takes up fluorescein.
Corneal abrasion (+/- foreign body) is the most common form of eye trauma presenting to the emergency department.
Q2. What are the important features on history and examination?
Answer and interpretation
History:
- History of trauma: scratching or hitting the eye, nature of the object, could a foreign body still be present?
- Symptoms: sharp pain, photophobia, foreign body sensation, tearing, discomfort with blinking.
- Contact lens use?
Examination:
- Visual acuity: may be reduced if central
- Slit lamp:
- Use topical anesthesia and identify an epithelial defect that stains with fluorescein.Assess size, depth, and location.Other features – conjunctival injection, edematous eyelid, mild AC reaction.
- Look for evidence of: infection — significant infiltrate, marked AC reaction, purulent discharge penetrating eye injury
Evert the eyelids to look for a foreign body!
Q3. What are the important differentials?
Answer and interpretation
Consider the possibility of:
- HSV keratitis
- recurrent corneal erosions
- superficial punctate keratopathy (SPK)
Q4. What is the management?
Answer and interpretation
Management:
- oral analgesia and topical cycloplegics
- topical antibiotic
- There is little evidence of efficacy
- The Australian Therapeutic Guidelines (2010) suggests chloramphenicol drops
- The Will’s Eye Manual suggests covering injuries due to fingernail scratches and vegetable matter with fluoroquinolones
contact lens wearers need anti-pseudomonal coverage (among other nasty bugs) and are best discussed with an ophthalmologist.
- consider removal of loose or hanging epithelium that may impair healing.
- tetanus prophylaxis if indicated.
Q5. What is the follow up?
Answer and interpretation
Review until healed. A small, peripheral lesion can be reviewed after about 3 days. A large or central lesion is best reviewed the next day.
Q6. What if the patient wears contact lenses?
Answer and interpretation
Contact lens wearers should be reviewed daily. Contact lenses should not be used until the defect is healed and the eye has felt back to normal for at least a week.
Q7. Why is it important to evert the eyelid during examination of the eye?
Answer and interpretation
To rule out the presence of an occult foreign body hidden under the upper eyelid. If missed ongoing trauma to the surface of the eye may occur.
Q8. How can the upper eyelid be everted?
Answer and interpretation
Here are 3 methods:
Method 1:
- Folding the upper eyelid on itself, using the tip of a cotton bud or similar device to help flex the lid ten hold it in place. This takes a surprising amount of skill and can make the novice look like, well, a novice.
- ask the patient to look down.
- place the cotton bud about 5 mm from the lid crease and apply light pressure.
- evert the over the cotton bud using the eyelashes to lift the eyelid up and away from the globe.
- hold in in the everted position with the tip of your cotton bud so that the eyelid doesn’t flick back, leaving you back where you started…
Method 2:
- Double-eversion using an eyelid retractor.
- If the upper eyelid is thoroughly anesthetised with topical anesthetic, the everted eyelid can be further everted using a modified paper clip (e.g. bed in half at 90 degrees and slide under the everted eyelid).
- It can give a great view, but its not always tolerated by the patient — despite what evangelists for the technique may say…
- Furthermore, flakes of metal from the paper clip can result in corneal abrasions.
Method 3 (ALIEM trick of the trade)
- An ingenious method I learned from Michelle Lin’s ‘Tricks of the Trade’ on Academic Life in Emergency Medicine is to use a cotton bud to roll the upper eyelid back on itself — too easy!

References
- Ehlers JP, Shah CP, Fenton GL, Hoskins EN. The Wills Eye Manual: Office and Emergency Room Diagnosis and Treatment of Eye Disease Lippincott Williams & Wilkins
- NSW Statewide Opthalmology Service. Eye Emergency Manual — An illustrated Guide. [Free PDF]

OPHTHALMOLOGY BEFUDDLER
Chris is an Intensivist and ECMO specialist at The Alfred ICU, where he is Deputy Director (Education). He is a Clinical Adjunct Associate Professor at Monash University, the Lead for the Clinician Educator Incubator programme, and a CICM First Part Examiner.
He is an internationally recognised Clinician Educator with a passion for helping clinicians learn and for improving the clinical performance of individuals and collectives. He was one of the founders of the FOAM movement (Free Open-Access Medical education) has been recognised for his contributions to education with awards from ANZICS, ANZAHPE, and ACEM.
His one great achievement is being the father of three amazing children.
On Bluesky, he is @precordialthump.bsky.social and on the site that Elon has screwed up, he is @precordialthump.
| INTENSIVE | RAGE | Resuscitology | SMACC
