Cardiac Megacode
aka Cardiovascular Curveball 003
As leader of the MET team you were called to a ‘Code Blue‘ to resuscitate a 57 year-old man who arrested on the ward post-operatively.
The initial rhythm was ventricular fibrillation.
Following defibrillation (1 x 200J biphasic), 1 mg adrenaline IV and 2 minutes of CPR he had an idioventricular rhythm with a rate of 40 but remained pulseless. CPR was continued for a further 2 minutes and 1.2 mg atropine was administered. The patient then had return of spontaneous circulation and was intubated as he remained unconscious.
This is his post-intubation ECG:
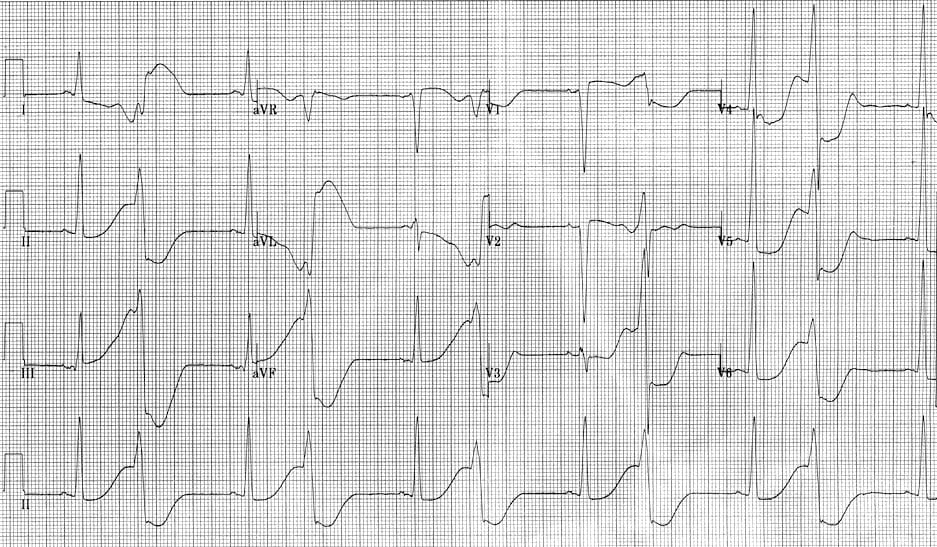
Q1. Describe this ECG.
Curveball Answer
This is an unusual ECG!
- There is an underlying sinus rhythm with normal axis.
- The QRS complexes are high voltage with markedly prolonged QT intervals (although the ends of many of the T waves are not easily seen).
- There is a broad complex (~120 msec) QRS occurring on every second T wave… This is consistent with bigeminal ventricular premature contractions (VPBs) with recurrent R-on-T phenomenon.
Q2. Can you guess what happened next?
Curveball Answer
He arrested again
- This time the ECG monitor was suggestive of torsades de pointes (‘twisting of the points’) – presumably because of the barn-door R-on-T phenomenon seen in the above ECG.
- He reverted to sinus rhythm following 1 x 200J biphasic defibrillation. However, the ECG monitor showed that he soon returned to the rhythm shown in his post-intubation ECG.
- His subsequent ECG revealed torsades de pointes

The features of torsades de pointes include:
- polymorphic ventricular tachycardia with a rate of >200/min.
- The axes of the QRS complexes undulate with the polarity of the complexes appearing to shift about the baseline.
- often occurs in short episodes (<90 seconds) but prolonged episodes can occur.
Q3. Post intubation arterial blood gas was performed. What does it show?
Curveball Answer
- The patient is ‘over-oxygenated‘.
- pH is normal with a mild respiratory acidosis and mild metabolic alkalosis.
- There is mild hyponatremia, hyperglycemia and a mild hyperlactemia.
- Overall this is a great gas for someone who just had a cardiac arrest!
The key abnormality though is the presence of hypokalemia, which is likely to have a causative role in this patient’s predilection for torsades.
Q4. What further management is necessary?
Curveball Answer
Correction of moderate hypokalaemia (1.5 – 3.5 mmol/L) with potassium and administration of magnesium for impending torsades de pointes.
- The patient was administered 20 mmol of KCl IV over 5 minutes via a central line and was administered 10 mmol MgCl2 IV.
- Note that 2015 ERC guidelines give the following recommendations for the rapid correction of hypokalaemia in the setting of impending cardiac arrest
Gradual replacement of potassium is preferable, but in an emergency, intravenous potassium is required. The maximum recommended IV dose of potassium is 20 mmol h−1, but more rapid infusion (e.g. 2 mmol min−1 for 10 min, followed by 10 mmol over 5–10 min) is indicated for unstable arrhythmias when cardiac arrest is imminent. Continuous ECG monitoring is essential during IV infusion and the dose should be titrated after repeated sampling of serum potassium levels.
20 mmol of KCl IV over 5 minutes via central line is more aggressive than the above recommendation (see comments on this post below).
Q5. Following appropriate treatment an ECG is taken. Describe the ECG.
Curveball Answer and interpretation
The ECG findings are:
- Atrial fibrillation (irregularly irregular with absent P waves) with a heart rate of ~ 100/min.
- Normal axis
- QRS complexes meets voltage criteria for left ventricular hypertrophy
- Sokolow-Lyon criteria: S(V1) + R(V5 or V6) > 35 mm;
- modified Sokolow criteria: S(V1 or V2) + R(V5 or V6) > 35 mm
- Cornell Criteria: R wave in aVL + S V3: > 28 mm (males) > 20 mm (females)
- Prolonged QT interval (QTc ~500)
- ST depression (up to 2-3 mm) predominantly in anterolateral leads (I,II, aVL and V3-V6)
- Widespread biphasic T waves
Review of this patient’s notes showed that a coronary angiogram 1 year previously has excluded coronary artery disease. However an echocardiogram was also performed at this time, the findings were consistent with severe hypertrophic obstructive cardiomyopathy (HOCM).
Emergency and critical care doctors need to look for the classic features of HOCM on the ECGs of patients presenting with syncope or arrhythmias.
The ECG is abnormal in about 90% of HOCM cases and features include:
- non-specific findings such as increased QRS voltage, QRS widening, ST segment and T waves changes consistent with hypertrophy.
- deep narrow Q waves in the lateral leads (I, II, aVL, V5, V6) with high voltage QRS’s in a younger patient with syncope is considered a specific finding highly suggestive of HOCM (not present in this patient’s ECG).
What does ST elevation in aVR mean?
Curveball Answer
Never forget to scrutinize aVR for ST elevation (STE) in a patient who may be having an acute coronary syndrome:
- It is 95% specific for left main coronary artery (LMCA) occlusion when there is evidence of ischaemia in other leads (typically widespread ST depression).
- Patients with significant STE in aVR due to an acute coronary syndrome have a 70% chance of developing cardiogenic shock or dying – and medical treatment (including thrombolysis) does nothing to change this… They need to go to the cath lab STAT!
The post-treatment ECG shown above has features consistent with an LMCA occlusion, however:
- the patient had atrial fibrillation and structural heart disease (HOCM) which may account for the ECG findings.
- the patient had a recent ‘normal’ coronary angiogram and an ECG at that time (although sinus rhythm was present) had a similar pattern of ST segment changes.
Finally, here are some more scary things to know about acute coronary syndromes with ST elevation in aVR (these do not apply in the absence of evidence of ischaemia in other leads, nor in the presence of supraventricular tachycardias):
- STE in aVR and aVL is highly specific for LMCA stenosis.
- STE in aVR and V1 is specific for proximal left anterior descending (LAD) or LMCA stenosis. If the STE in aVR is greater than the STE in V1 this indicates LMCA stenosis (81% sensitivity, 80% specificity, and 81% accuracy) rather than LAD stenosis.
- STE in aVR >1.5mm has ~75% mortality!
References
- Williamson K, Mattu A, Plautz CU, et al. Electrocardiographic applications of lead aVR. Am J Emerg Med 2006;24:864-874. PMID: 17098112.
- LITFL ECG Library – The R Wave
- LITFL ECG Library – LMCA
Further Reading
- Wiesbauer F, Kühn P. ECG Mastery: Yellow Belt online course. Understand ECG basics. Medmastery
- Wiesbauer F, Kühn P. ECG Mastery: Blue Belt online course: Become an ECG expert. Medmastery
- Kühn P, Houghton A. ECG Mastery: Black Belt Workshop. Advanced ECG interpretation. Medmastery
- Rawshani A. Clinical ECG Interpretation ECG Waves
- Smith SW. Dr Smith’s ECG blog.
- Wiesbauer F. Little Black Book of ECG Secrets. Medmastery PDF
CLINICAL CASES
Cardiovascular Curveball
Chris is an Intensivist and ECMO specialist at The Alfred ICU, where he is Deputy Director (Education). He is a Clinical Adjunct Associate Professor at Monash University, the Lead for the Clinician Educator Incubator programme, and a CICM First Part Examiner.
He is an internationally recognised Clinician Educator with a passion for helping clinicians learn and for improving the clinical performance of individuals and collectives. He was one of the founders of the FOAM movement (Free Open-Access Medical education) has been recognised for his contributions to education with awards from ANZICS, ANZAHPE, and ACEM.
His one great achievement is being the father of three amazing children.
On Bluesky, he is @precordialthump.bsky.social and on the site that Elon has screwed up, he is @precordialthump.
| INTENSIVE | RAGE | Resuscitology | SMACC



Nice, thank you so much!