ECG Case 128
Thank you to a reader for submitting this case for discussion.
A 46-year-old man presents with three days of intermittent left scapular pain, acutely worsening one hour ago. Past history includes hypertension, smoking. SpO2 100 RA, BP 163/67.
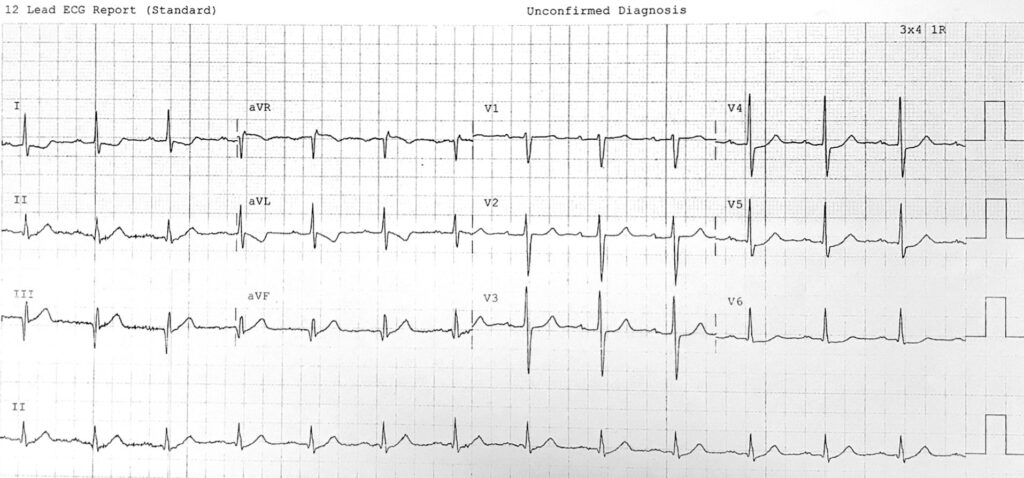
The computer reads:
Normal sinus rhythm
Inferior Q waves, likely old inferior MI
Lateral ST depression, consider ischaemia
Do you agree?
Describe and interpret this ECG
ECG ANSWER and INTERPRETATION
This ECG is concerning for rapidly evolving inferior occlusion myocardial infarction (OMI) that requires urgent reperfusion:
- There is 1st degree AV block, PR interval ~200ms
- Q waves in lead III are pathological and extend into adjacent inferior leads, predominantly aVF
- T waves in II, III and aVF are hyperacute in nature, with reduction in preceding QRS amplitude
- T-wave inversion in aVL is abnormal here, as there is a widened QRS-T wave axis
- Flattened ST segment in V2 is abnormal and concerning for “posterior” extension of infarct territory with right ventricular (RV) involvement
ST depression extends to V4-6 which may be reciprocal change to evolving inferior infarction, or due to diffuse subendocardial ischaemia in the context of undiagnosed triple vessel disease. However, it is unclear at this stage where the maximum ST depression will be when the full-blown ST vector becomes apparent. Localisation is always difficult with such subtle changes, and serial ECGs (ideally every 10 minutes) are of utmost importance for clarification.
OUTCOME
This patient was worked up for a possible “NSTEMI”. He was given antiplatelet therapy and IV opioid analgesia. Pain persisted with the following ECG taken one hour later:
What is your interpretation?
Reveal answer
- There is now an evolved inferior STEMI with marked ST elevation in III and aVF, and reciprocal ST depression in aVL
- ST elevation in III > II, and ST depression in V2 relative to V1, suggests RV infarction as earlier suspected
- Earlier seen 1st degree AV block has now progressed to type I 2nd degree AV block — note there is a 3-beat grouping sequence, with gradual prolongation of the PR interval within these sequences. Non-conducted P waves are buried in the preceding T wave
This patient suffered a VF arrest shortly after the above ECG was taken. CPR was commenced with subsequent ROSC. He was taken to the cath lab where a 100% mid-level right coronary artery occlusion was found, as well as severe triple vessel disease.
Despite subsequent PCI, the patient became severely bradycardic and a temporary pacing wire was floated to maintain perfusion.
CLINICAL PEARLS
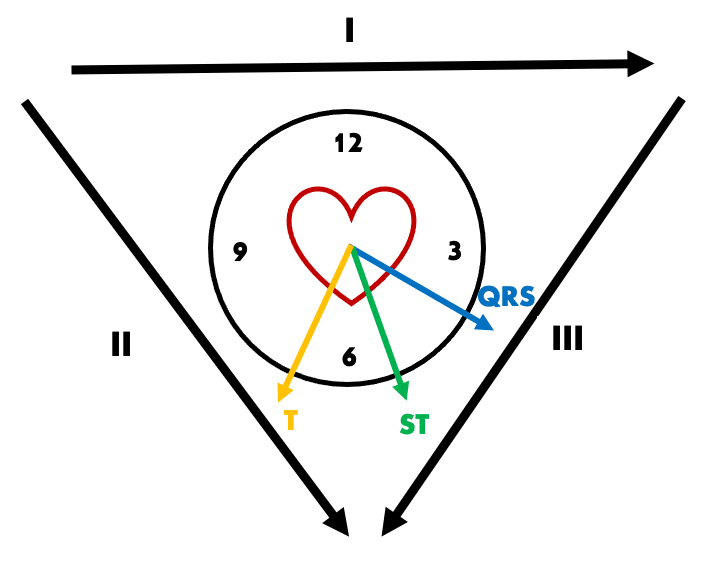
QRS-T wave angle as a marker of ischaemia
aVL is the only lead truly reciprocal to the inferior wall, and we often examine this lead closely for ST-T changes in suspected inferior OMI. Although ST depression in aVL is common in inferior OMI, it may not be evident at early stages of infarction. In our patient above, pathological T wave inversion in aVL precedes any other reciprocal change. We know that T-wave inversion in aVL can be a normal variant, and last week we discussed the QRS-T wave angle as an additional tool for differentiating such benign versus ischaemic T wave inversion.
In our patient above, QRS axis is + 30 degrees and T wave axis + 120 degrees, giving a QRS-T wave angle of 90 degrees. Such a wide angle (> 45 degrees) suggests T-wave inversion seen in lead I and aVL is pathological and due to a primary repolarisation abnormality of inferior infarction.
AV block in inferior MI
Varying degrees of AV nodal block are common in inferior MI, as the AV node is supplied by the RCA in approximately 80% of the population. 20% of patients with inferior OMI will develop 2nd or 3rd degree AV block — around half of these will demonstrate a step wise progression as with our patient above, with the other half suffering abrupt onset.
Such blockade may be subtle in early stages, especially as these patients do not always manifest bradycardia due to concurrent sympathetic drive from pain and ischaemia. Identifying such AV blockade may assist in making the early diagnosis of inferior OMI, and allow us to monitor for progression to fatal bradyarrhythmias.
Note: SA nodal dysfunction is also common in inferior OMI, as the SA node is supplied by the RCA in the majority (60%) of patients. Manifestations include sinus bradycardia, sinus pauses, or SA block.
“Flattened” V2 and RV infarction
Most “normal” ECGs demonstrate some degree of ST elevation in right precordial leads, especially V2-3. A completely isoelectric ST segment as seen in our patient’s first ECG is abnormal and indicates a relative degree of ST depression.
In the absence of dedicated right-sided leads, V1 is the only standard ECG lead that looks directly at the right ventricle. Any degree of ST depression in V2 relative to V1 is suggestive of right ventricular infarction (note that V1 will not always manifest ST elevation).
- In the early stages of inferior OMI, ST segment changes will not always be evident. Examine for other suggestive ECG features including reciprocal change in aVL, AV blockade, and flattening of the ST segment in V2 relative to V1
- Reciprocal ST depression in aVL may be preceded by T-wave inversion. The QRS-T wave angle can assist us to determine if such T-wave inversion is normal variant or due to evolving inferior infarction
- If in doubt, obtain serial ECGs early, ideally every 10 minutes in the initial assessment period!
Further reading
Related topics
- ECG Case 127
- Occlusion myocardial infarction (OMI)
- Inferior STEMI
- RV infarction
- 2nd degree AV block: type I
Expert Review
- Smith SW. Inferior subtle ST elevation. Dr Smith’s ECG Blog. 2019 June
TOP 150 ECG Series
MBBS DDU (Emergency) CCPU. Adult/Paediatric Emergency Medicine Advanced Trainee in Melbourne, Australia. Special interests in diagnostic and procedural ultrasound, medical education, and ECG interpretation. Co-creator of the LITFL ECG Library. Twitter: @rob_buttner
Interventional cardiologist, ECG and hemodynamics fan. MD, Assoc. Prof. at Marmara University, Pendik T&R Hospital, Assoc. Editor at Archives of TSC, ESC National Prevention Coordinator